In a significant proportion of patients with kidney disease requiring dialysis, high blood pressure is a major factor in the advanced stage of the disease. Antihypertensive therapy may reduce the risk of end-stage renal dysfunction.
Most kidney disease is associated with high blood pressure, and conversely, people with hypertension have an increased risk of developing kidney disease. The interactions in this structure are complex and have to do with the control of blood pressure and fluid balance by the hormone and urine production of the kidney. This is reflected, among other things, in the fact that renal insufficiency leads to fluid and pressure overload in the bloodstream.
Hypertension increases risk of terminal kidney injury
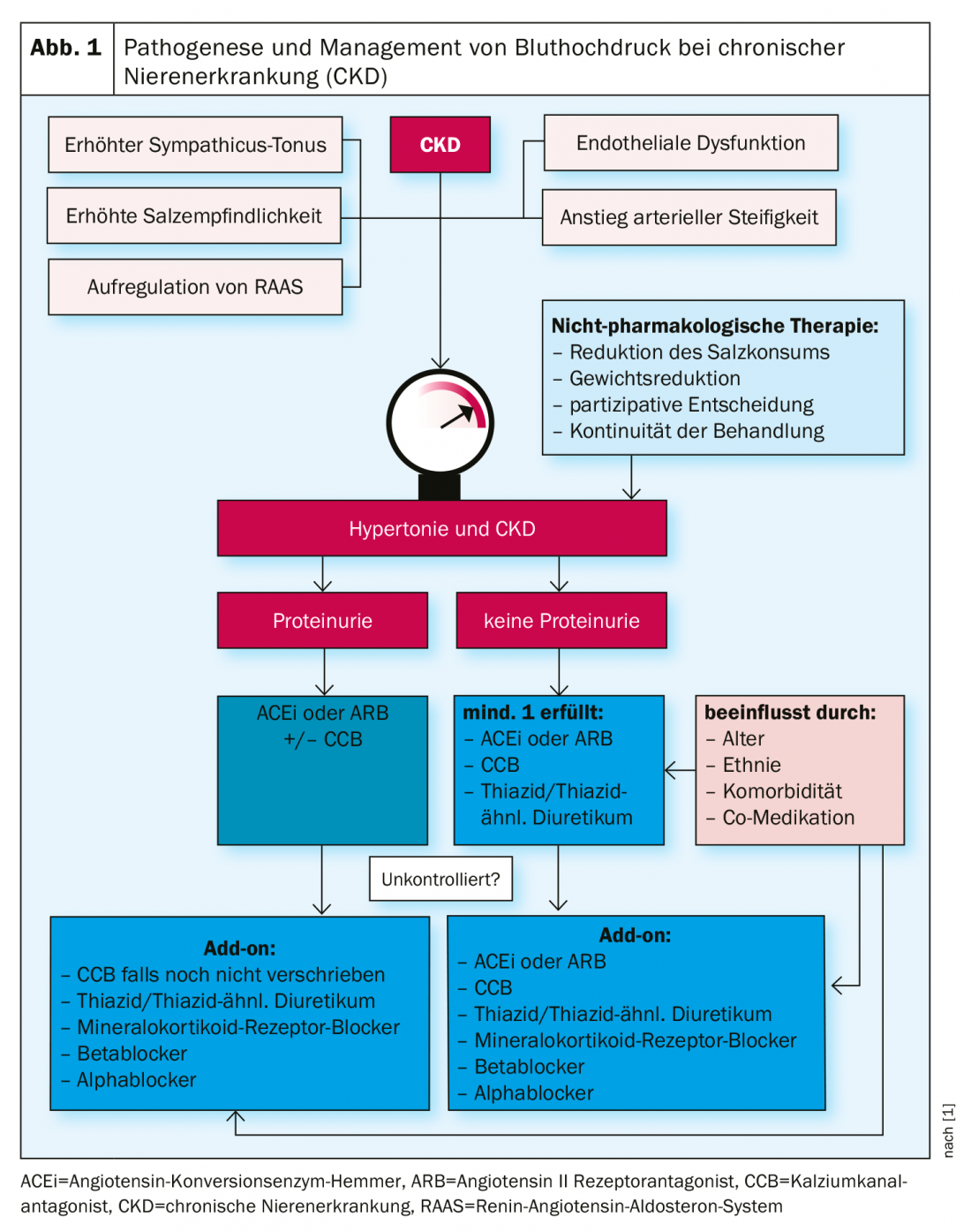
Chronic kidney disease (CKD) is an increasingly common health problem worldwide and a significant risk factor for cardiovascular disorders [1]. Excessive blood pressure is both a cause and an effect of CKD and affects a large proportion of people with chronic kidney disease. The prevalence of hypertension is up to 90% in European patients with CKD, approximately three times higher than in the general adult population [1]. If left untreated, hypertension leads to renal failure and the need for renal replacement therapy in patients with renal impairment. According to epidemiological data from Europe, high blood pressure is the cause of end-stage renal disease in 10-19% of patients requiring dialysis [2]. According to figures from the US Renal Data System [3], high blood pressure is the second most common cause of dialysis, and blood pressure-related damage to the kidneys is the main reason for renal replacement therapy in almost 30% of patients.
Monitoring of blood pressure is important
Early detection and treatment of high blood pressure can delay or even prevent terminal kidney disease. The current ESH guidelines recommend lifestyle factor measures (e.g., reduction of salt intake) for values >130/80 mm Hg and the use of antihypertensive medications for values >140/90 mmHg [4]. In patients with CKD, antihypertensives should be prescribed earlier because they have renal protective effects. Many patients with mild renal dysfunction are unaware that consistent blood pressure reduction can prevent the progression of kidney disease.
Blood pressure reduction decisive influencing factor for eGFR
A decrease in estimated glomular filtration rate (eGFR) is associated with an increase in the incidence and severity of hypertension [5]. Both chronic kidney disease and high blood pressure are unaffected risk factors for cardiovascular disorders. If these two health problems are comorbid, the risk of cardiovascular disease and mortality is increased [6]. According to the KDIGO guidelines (“Kidney Disease: Improving Global Outcomes”), the risk of cardiovascular mortality is higher than the risk of end-stage renal disease when CKD is grade 3 (eGFR 30-59 mL/min/1.73 m2) or grade 4 (eGFR 15-29 mL/min/1.73 m2) [7]. Blood pressure lowering may slow eGFR decline, delay the development of ESRD, and reduce the risk of cardiovascular events in this patient population.
Lower target values associated with lower MACE rate
A randomized-controlled trial [8] demonstrated that in patients with chronic kidney disease and hypertension, a target systolic value of <120 mmHg compared with <140 mmHg resulted in a reduction in cardiovascular events and all-cause mortality. Subjects received either intensive therapy (n=1330; target systolic <120 mmHg) or standard therapy (n=1316; target systolic <140 mmHg). Those patients who underwent intensive blood pressure therapy had a nearly 20% lower risk of a major adverse cardiovascular event (MACE) over a 3.3-year period than subjects in the standard of care condition.
Literature:
- Pugh D, Gallacher PJ, Dhauncorresponding N: Management of Hypertension in Chronic Kidney Disease Drugs 2019; 79(4): 365-379.
- ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2017; available at: https://era-edta-reg.org/files/annualreports/pdf/AnnRep2017.pdf
- Saran R, et al: US Renal Data System 2014 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2015; 66: Svii (S1-S305).
- Hamrahian SM, Falkner B: Hypertension in Chronic Kidney Disease. Adv Exp Med Biol 2017; 956: 307-325. doi: 10.1007/5584_2016_84.
- Muntner P, et al: Chronic Renal Insufficiency Cohort (CRIC) Study Investigators. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 2010; 55(3): 441-451.
- Gansevoort RT, et al: Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013; 382: 339-352.
- Stevens PE, Levin A: Evaluation and management of chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2012 clinical practice guideline. Ann Intern Med 2013; 158: 825-830.
- Cheung AK, et al: Effects of intensive BP control in CKD. J Am Soc Nephrol 2017; 28: 2812-2823.
HAUSARZT PRAXIS 2019; 14(11): 18-19