Multivalvular heart disease is a common condition whose incidence will continue to increase as a result of demographic change. A combination of aortic stenosis and mitral regurgitation is most common. A crucial role in treatment is played by the cooperation of cardiologists and cardiac surgeons in the heart team.
Multivalvular heart disease (“MVD”) refers to the combination of valvular vitiation (stenosis or insufficiency) at two or more heart valves [1]. It has a high prevalence. In the Euro Heart Survey, which collected data from over 5000 patients in 25 countries, 20.2% of patients with native valvular heart disease had MVD [2]. The mean age of patients was 64 years and 83.6% were male. In the PARTNER trials, approximately 20% of patients with severe aortic stenosis (AS) had concomitant moderate to severe mitral regurgitation (MI) [3]. For a long time, the majority of MVD was of rheumatic origin [4]. Currently, due to the decreasing incidence of rheumatic fever on the one hand and the increase in the aging population on the other hand, a growing proportion of degenerative valvular heart disease is emerging as a cause of MVD. In the Euro Heart Survey, degeneration was clearly the most common etiology with 82% in AS and 61% in MI [5].
Pathophysiology
The clinical expression of MVD depends on many factors and can be very complex. These include the severity of each valve defect, the combination of valves involved, the type of valve disease (primary or secondary), the hemodynamic effects, and the ventricular compensatory mechanisms. The severity and clinical symptoms may vary if hemodynamics change or one of the valve defects is treated. This complex and dynamic pathophysiology makes the diagnosis and treatment of MVD very challenging.
AS and MI influence each other and may, among other things, exacerbate the hemodynamic effects of the other valve defect.
AS leads to increased afterload and subsequent hypertrophy of the left ventricle. Pressure loading of the left ventricle can lead to systolic dysfunction, dilatation of the mitral valve annulus, and thereby functional (secondary) MI [6]. Pressure loading from an AS can exacerbate an existing MI. AS often occurs in combination with coronary artery disease (CAD) because both are due to the same systemic atherosclerotic processes. Therefore, the occurrence of functional MI with ischemic cause due to CHD is another genesis [7]. In this case, valve function is impaired by dysfunction of the papillary muscles and adjacent myocardial segments. In addition, of course, a combination of AS and degenerative MI may occur.
Concomitant MI may exacerbate the clinical expression of AS. The increased ejection resistance due to AS promotes systolic reflux through the leaky mitral valve [8]. This further reduces the antegrade ejected blood volume and increases the forward failure of the left ventricle. MI causes a “low-flow status” over the aortic valve [6]. Atrial fibrillation often occurs in combination with MI, which may worsen the clinical symptoms of AS because the lack of synchronous atrial contraction and the high heart rate reduce LV diastolic filling. Atrial fibrillation is poorly tolerated by patients with AS, often leading to decompensation. Even without the presence of MI, AF leads to increased mortality in patients with AS [9].
Diagnostics
The diagnosis and evaluation of heart valves in MVD is significantly more difficult due to altered hemodynamics [6]. On clinical examination, auscultation may be misinterpreted because heart sounds are altered in timing and intensity. Other signs, such as the pulse curve, may also present as atypical for the particular valve defect.
Echocardiography: The most important diagnostic tool for the evaluation of heart valves is echocardiography. This should include quantification of stenosis or insufficiency and evaluation of valve anatomy and function. In addition, an assessment of the right and left ventricles must be performed and the effect of valve defects on hemodynamics must be visualized [10]. It should be noted that many of the measurement parameters commonly used to assess heart valves have been validated only in isolated valve defects. In general, altered hemodynamics should be considered in the echocardiographic diagnosis of MVD [1]. Current European Society of Cardiology (ESC) guidelines emphasize that different echocardiographic measurements should be combined to include interaction between valve defects [11].
On echocardiographic assessment of AS, MI may favor a “low-flow/low-gradient status” because the existing insufficiency flow decreases the gradient across the aortic valve. This complicates AS quantification and may lead to underestimation of AS severity (Fig. 1) [12]. In addition, there is a risk that the cw Doppler measurement of AS will include the mitral valve insufficiency jet. This would lead to an overestimation of the AS.
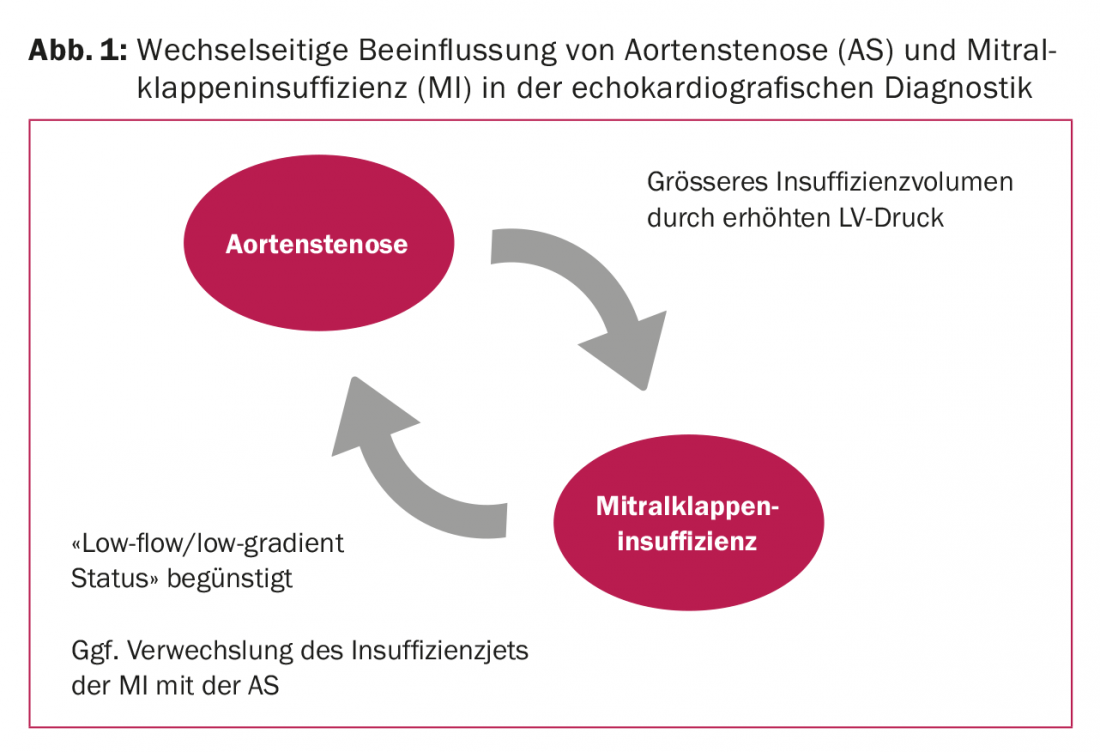
The increased left ventricular pressure in AS increases the volume of insufficiency across the mitral valve and presents disproportionately high compared with the effective regurgitant orifice area (ERO). The insufficiency volume here shows the hemodynamic load and often correlates with the patient’s clinical symptoms. However, ERO should be used to evaluate the mitral valve, as it is less affected by AS.
Because functional measurements (gradients, flow, etc.) are confounded by altered hemodynamics, special emphasis should be placed on morphologic assessment of the valves (structural changes, such as degree of calcification). Transesophageal echocardiography is usually more informative than transthoracic echocardiography.
Complementary diagnostics: If a clear diagnosis cannot be made by conventional echocardiography, other diagnostic procedures are required. An accurate diagnosis is essential to make the correct treatment decision. In cases of reduced LV pump function, dobutamine stress echocardiography should be performed if transthoracic echocardiography reveals a “low-flow/low-gradient status” (stroke volume index <35 ml/min/m²) to rule out pseudosevere AS. Quantification of the degree of calcification of the aortic valve by CT is becoming increasingly important in the diagnosis of AS [11,13]. This parameter is completely independent of hemodynamics.
Therapeutic regime
Because there is very little literature on MVD, the current ESC guideline makes only recommendations that are not evidence-based (evidence level C) [11].
The therapeutic decision must be made in synopsis of all valve defects and should be made by a so-called multidisciplinary cardiac team (interventional cardiologists, imaging experts, cardiac surgeons, anesthesiologists, and others). Importantly, surgery on more than one valve increases operative risk. In the Euro Heart Survey, patients with MVD had a postoperative hospital mortality of 6.5%, whereas patients who had surgery on only one valve had a hospital mortality of 0.9 to 3.9% [2]. Another study showed a postoperative mortality of 10.7% for combined aortic and mitral valve surgery [14]. Main risk factors for increased mortality appear to be pulmonary hypertension and advanced heart failure with NYHA stage IV. However, after surgery, studies show significant clinical improvement and better long-term prognosis. When deciding which surgical (or interventional) therapy to use, it is important to consider that any reoperation on the second valve defect that may be necessary significantly increases the surgical risk and worsens long-term survival.
After replacement of the stenosed aortic valve, left ventricular pressure decreases, which also relieves the mitral valve and may improve MI [8]. Therefore, the new ESC guidelines recommend a rather cautious surgical approach to the mitral valve if no structural changes such as leaflet abnormalities are present [11].
Interventional valve replacement: Percutaneous valve therapies are increasingly performed in patients with high and intermediate surgical risk. During transcatheter aortic valve implantation (TAVI), concomitant moderate- or high-grade MI increases 30-day mortality compared with patients with low-grade MI [15]. After 30 days, no differences are found in both groups. Patients with moderate- or high-grade MI show equal survival rates compared with patients with low-grade MI, even after two years.
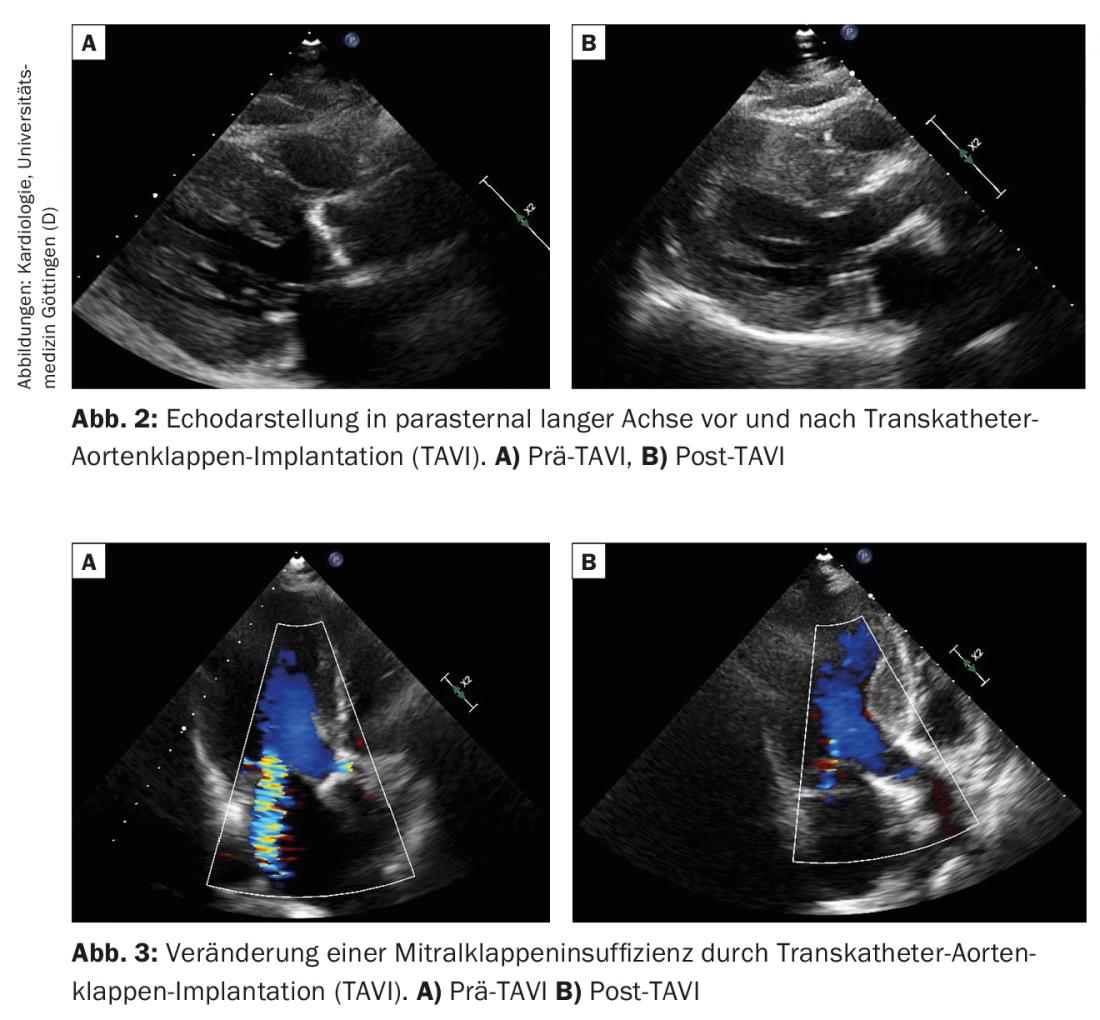
After TAVI, functional MI can improve significantly (Figs. 2 and 3) . However, the response of the mitral valve is very heterogeneous. Immediately after TAVI, MI decreases in a majority of patients. A study of 478 patients showed that moderate- or high-grade MI was reduced in 61% of patients after TAVI [15]. After one year, MI had improved in 55%, was unchanged in 16%, and had worsened in 1%. Factors associated with a reduction in MI after TAVI include: no atrial fibrillation, no pulmonary hypertension, and a particularly high transvalvular gradient across the aortic valve preoperatively (>40 mmHg). Functional MI is more likely to decrease in MI severity after TAVI than degenerative (primary) MI.
Very few data exist to date on combined percutaneous therapy of the aortic valve and mitral valve. In the few patients studied, a two-stage approach has proven effective. First, AS was treated by TAVI and, in the second step, a MitraClip® was implanted if moderate- to high-grade MI and symptoms persisted three months after TAVI. The success rates of the procedure were very good. At six months, improved functional status and good short-term survival were evident [16]. However, complementary long-term studies with larger patient groups are needed to verify the benefit of this approach.
Conclusion
MVD is a common condition whose incidence will continue to increase as a result of demographic change. A combination of AS and MI is most common. The most important diagnostic tool is echocardiography. It should be noted here that a combination of AS and MI in particular may confound measurements of hemodynamics. Surgical valve replacement increases mortality due to a second valve defect. An alternative to this may be percutaneous valve intervention, although a two-stage procedure is recommended to allow re-evaluation after therapy of one valve. Further clinical studies are needed to enable evidence-based recommendations. A crucial role in treatment is played by the cooperation of cardiologists and cardiac surgeons in the heart team.
Take-Home Messages
- One-fifth of patients with native valve disease have multivalvular heart disease (MVD), most commonly a combination of aortic valve stenosis (AS) and mitral regurgitation (MI).
- Functional diagnosis is complicated by the mutual influence of valve defects.
- Morphologic evaluation of the valves by echocardiography and CT is particularly important in MVD (degree of calcification).
- There are no evidence-based treatment recommendations for MVD. The therapy decision should be made individually by the heart team.
- Surgery on more than one heart valve increases perioperative risk.
- After transcatheter aortic valve implantation (TAVI), functional MI can improve significantly. If necessary, a two-stage procedure with subsequent MitraClip® can be considered.
Literature:
- Unger P, et al: Pathophysiology and management of multivalvular disease. Nat Rev Cardiol 2016; 13(7): 429-440.
- Iung B, et al: A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. European Heart J 2003; 24(13): 1231-1243.
- Leon MB, et al: Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010; 363(17): 1597-1607.
- Roberts WC, Sullivan MF: Clinical and necropsy observations early after simultaneous replacement of the mitral and aortic valves. The American Journal of Cardiology 1986; 58(11): 1067-1084.
- Iung B, Vahanian A: Epidemiology of valvular heart disease in the adult. Nat Rev Cardiol 2011; 8(3): 162-172.
- Unger P, et al: Mitral regurgitation in patients with aortic stenosis undergoing valve replacement. Heart (British Cardiac Society) 2010; 96(1): 9-14.
- Paradis JM, et al: Aortic stenosis and coronary artery disease: what do we know? What don’t we know? A comprehensive review of the literature with proposed treatment algorithms. European Heart J 2014; 35(31): 2069-2082.
- Unger P, et al: Effects of valve replacement for aortic stenosis on mitral regurgitation. The American Journal of Cardiology 2008; 102(10): 1378-1382.
- Burup Kristensen C, et al: Atrial fibrillation in aortic stenosis-echocardiographic assessment and prognostic importance. Cardiovasc Ultrasound 2012; 10: 38.
- Lancellotti P, et al: Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2013; 14(7): 611-644.
- Baumgartner H, et al: 2017 ESC/EACTS Guidelines for the management of valvular heart disease: The Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2017; 38(36): 2739-2791.
- Unger P, et al: Management of multiple valve disease. Heart (British Cardiac Society) 2011; 97(4): 272-277.
- Clavel MA, et al: The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. Journal of the American College of Cardiology 2013; 62(24): 2329-2338.
- Vassileva CM, et al: Outcome characteristics of multiple-valve surgery: comparison with single-valve procedures. Innovations (Philadelphia, Pa) 2014; 9(1): 27-32.
- Toggweiler S, et al: Transcatheter aortic valve replacement: outcomes of patients with moderate or severe mitral regurgitation. Journal of the American College of Cardiology 2012; 59(23): 2068-2074.
- Kische S, et al: Staged total percutaneous treatment of aortic valve pathology and mitral regurgitation: institutional experience. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions 2013; 82(4): E552-63.
CARDIOVASC 2018; 17(2): 22-25











