The possible link between osteoarthritis (OA) and an atopic disease such as atopic dermatitis (AD) or bronchial asthma was investigated by US scientists. Their finding: patients with asthma or AD are more likely to develop osteoarthritis. And those who suffer from both diseases live at particularly high risk.
Since there are limited treatment options for OA, it is of great interest to determine whether the disease can be prevented by certain preventive measures. Dr. Matthew Baker of the Department of Immunology and Rheumatology at Stanford University and colleagues conducted a retrospective cohort study using data from the CDM (Optum’s de-identified Clinformatics Data Mart Database) and STARR (Stanford Research Repository) registries from 2003 to 2020 [1].
From the Optum CDM insurance registry, 117,346 exposed patients with asthma or atopic dermatitis (mean age 52 years; 60% women) and 1,247,196 unexposed controls (mean age 50 years; 48% women) were included who were over 18 years of age, had been insured with Optum for at least seven years, and had no diagnosed OA or atopic disease in the first 2 years, as well as no history of inflammatory arthritis. The STARR group used the same definitions as Optum CDM, except that the observation period was five years instead of seven.
Risk increased by 58
After propensity score matching, the incidence of OA was higher in patients with asthma or AD than in unexposed patients (26.9 vs. 19.1 per 1000 person-years), with an adjusted odds ratio (aOR) of 1.58 for the development of OA (95% CI 1.55-1.62). This effect was even more pronounced in patients who had both asthma and AD compared with nonexposed patients (aOR=2.15; 95% CI 1.93-2.39) and in patients with asthma compared with those with COPD (aOR=1.83; 95% CI 1.73-1.95) (Fig. 1). In the STARR group, which included additional body mass index data, the aOR for the development of OA in asthmatics or patients with AD versus nonexposed patients was 1.42 (95% CI 1.36-1.48).
The STARR cohort included 114 427 patients, including 43 728 affected individuals with asthma or AD and 70 699 unexposed controls without atopic disease. Those with asthma or atopic dermatitis were younger (mean age 51 vs. 53 years), more often female (64% vs. 61%), had a higher mean Charlson Comorbidity Score (0.9 vs. 0.8), fewer outpatient visits per year (3.9 vs. 4.1), and a slightly higher mean BMI (27.3 vs. 27.0).
Close links in the development of disease
Here, too, the increased risk of osteoarthritis was confirmed, although not quite as pronounced as in the Optum CDM group: after adjustment for, among other things, age, sex, ethnicity, and Charlson Comorbidity Score the aOR for developing OA in patients with asthma or atopic dermatitis compared with unexposed patients was 1.47 (95% CI 1.42-1.53, p<0.001); in patients with both diseases, the value was 1.25 (95% CI 1.16-1.34, p<0,001). After additional adjustment for BMI, the aOR in patients with asthma or AD was 1.42 (95% CI 1.36-1.48, p<0.001) and 1.19 (95% CI 1.11-1.28, p<0.001), respectively.
There is now a cluster of data pointing to close links between a number of allergic pathways and the development of OA, the authors write. These include:
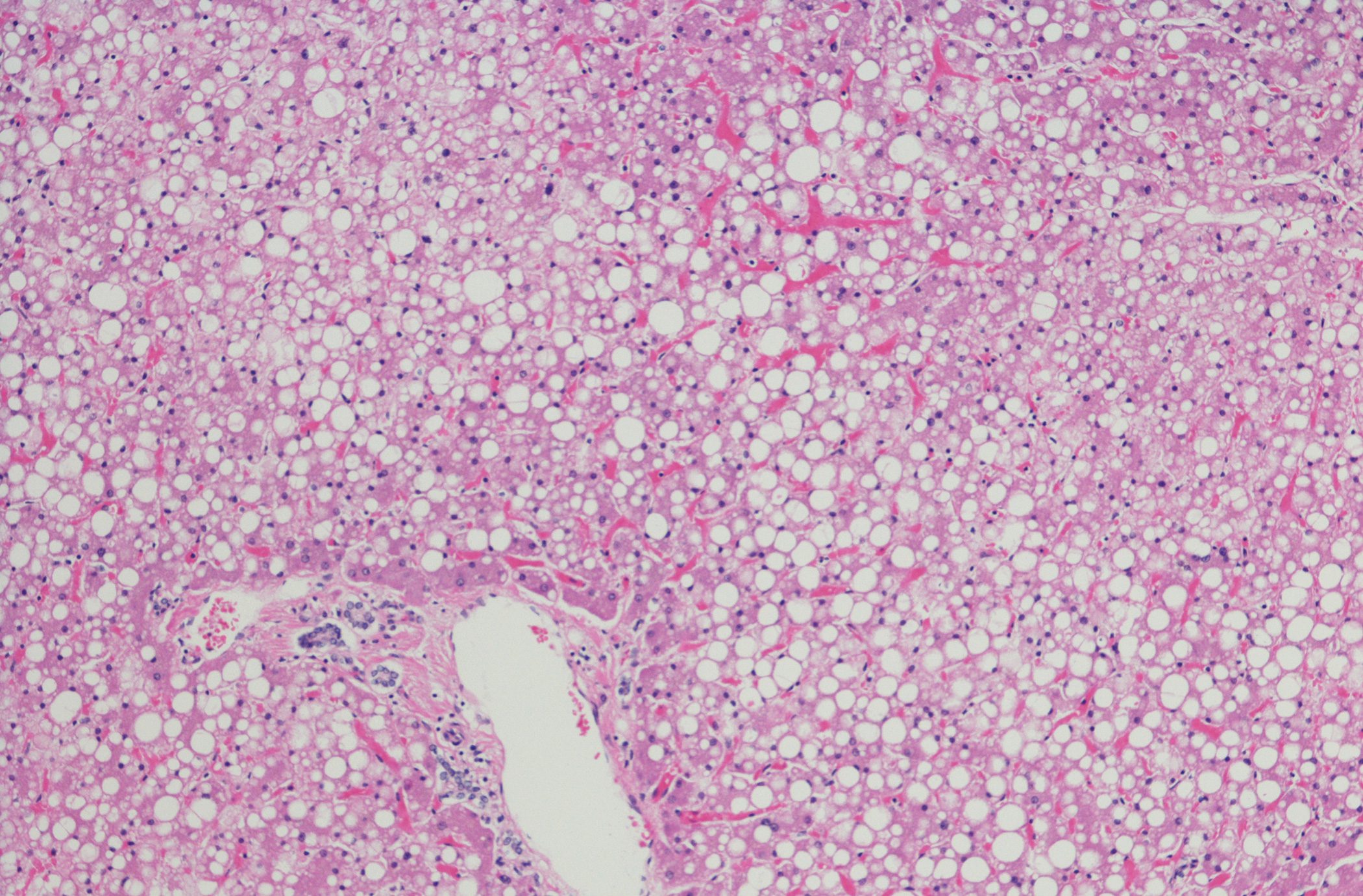
- Activated and degranulating mast cells were found in greater numbers in the synovium of patients with OA [6].
- Mast cell activation and tryptase release mediates synovitis and joint tissue breakdown in OA [6–8].
- Genomic analyses have discovered associations between IL-4 and IL-4 receptor gene polymorphisms and the development of OA [9–11].
- Increased presence of mast cells along with increased tryptase has also been associated with the pathogenesis of asthma [12].
Dr. Baker and colleagues refer to a Korean study that had shown an increased prevalence of OA in asthma patients compared with patients with COPD and controls [2]. In this earlier work (425 patients with asthma [135 mit OA] and 1131 patients with COPD [201 mit OA]), it had been limited to draw conclusions about the order of disease development and thus to determine whether atopic disease directly contributed to the development of OA. However, the findings would support the current results. The current analysis was extended to use two independent, much larger cohorts that included patients with atopic dermatitis in addition to asthma. The design of their study also allowed them to identify patients who were definitively diagnosed with atopic disease before they were diagnosed with OA, the authors said.
The study had shown a strong association between asthma and OA but not between COPD and OA, supporting the hypothesis that type 2 immune responses specifically contribute to the risk of developing OA but not lung disease in general. If the current observations are confirmed, nonatopic patients may benefit from treatment that inhibits mast cells and allergic cytokines to prevent the development of osteoarthritis, Dr. Baker et al conclude.
Literature:
- Baker MC, Sheth K, Lu R, et al: Increased risk of osteoarthritis in patients with atopic disease. Ann Rheum Dis 2023; 82: 866-872; doi: 10.1136/ard-2022-223640.
- Koo HK, Song P, Lee JH: Novel association between asthma and osteoarthritis: a nationwide health and nutrition examination survey. BMC Pulm Med 2021; 21: 59; doi: 10.1186/s12890-021-01425-6.
InFo RHEUMATOLOGY 2023; 5(1): 29.