From the age of five, daytime wetting is considered incontinence. Treatment is preferably multimodal. In certain cases, referral to a specialized pediatric clinic should be made.
The bladder, as a low-pressure system, is responsible for the storage and coordinated emptying of urine. Voluntary control of the bladder and regulation of micturition require a complex interaction between autonomic and somatic pathways with connections to multiple centers in the brain and spinal cord. In children, unlike in adults, certain processes are subject to maturation and the question arises as to when incontinence in children is considered pathological and should be further clarified. Children reach daytime urinary incontinence at an average age of 3.5 years, girls slightly earlier than boys. By the age of six, almost all children are continent. There is usually an interval of about four months between achieving daytime and nighttime continence [1,2].
Definition incontinence
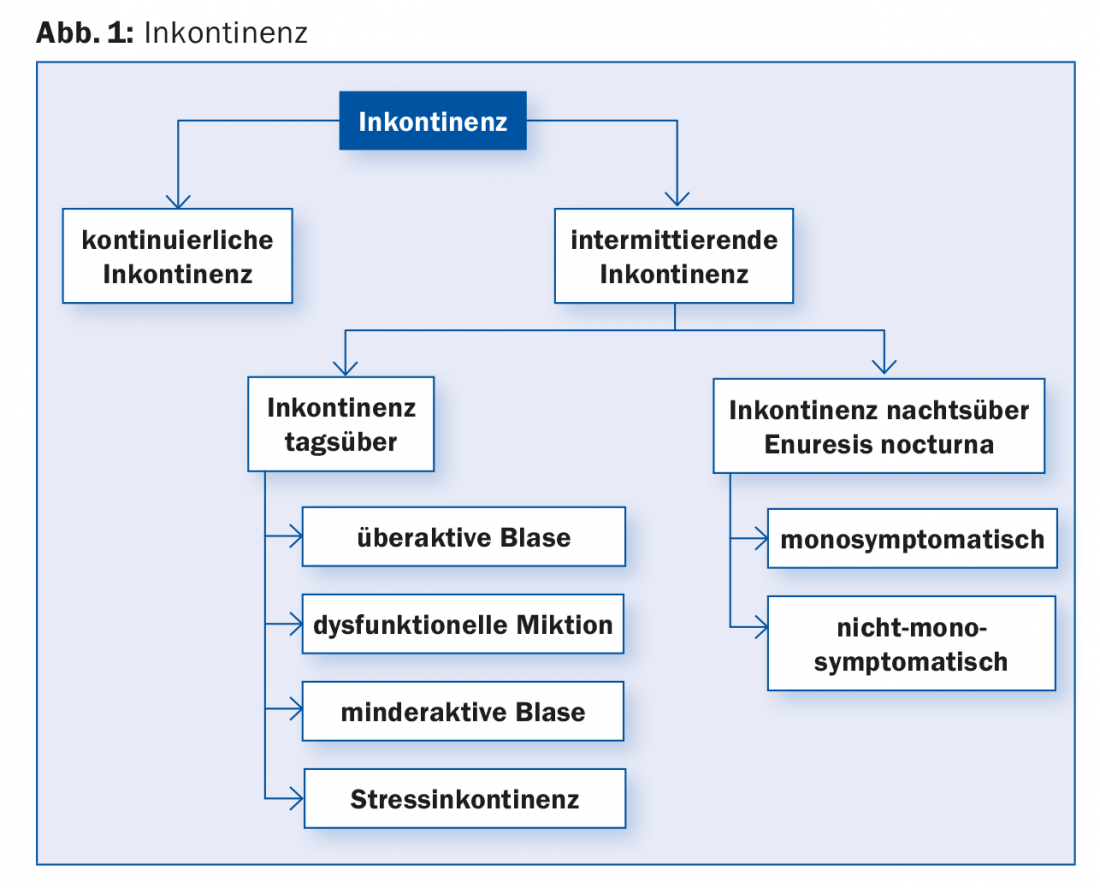
According to the ICCS (International Children’s Continence Society), daytime incontinence is said to occur in a child over the age of five. Incontinence means involuntary loss of urine that is intermittent or continuous and occurs more than once a month or three times in three months. A distinction is made between daytime incontinence (the term enuresis diurna should no longer be used) and nighttime incontinence, enuresis nocturna (Fig. 1) [3]. Daytime incontinence occurs with an incidence of up to 6.3% [4]. Behavioral problems including attention deficit hyperactivity disorder, defiant behavior, and anxiety disorders can be seen in up to 30% of cases [3].
Genesis
The interaction of detrusor and sphincter is subject to a developmental process. In overactive bladder, the genesis is controversial. Several studies indicate that it is a disorder of cortical detrusor inhibition rather than immaturity [5].
Clarification
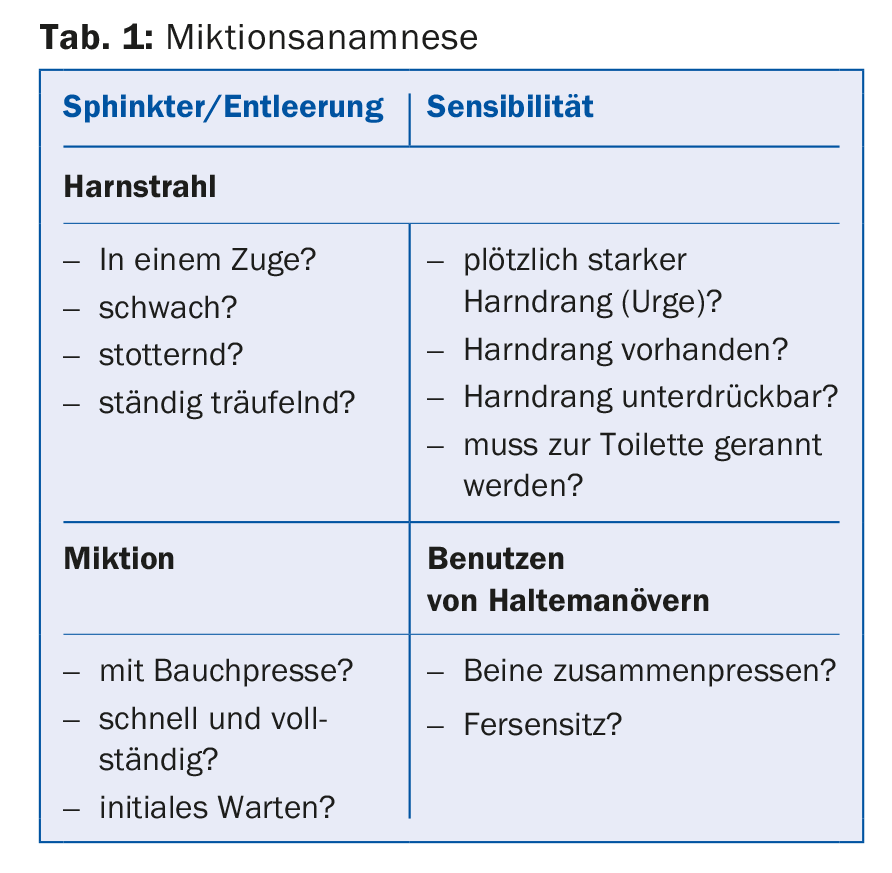
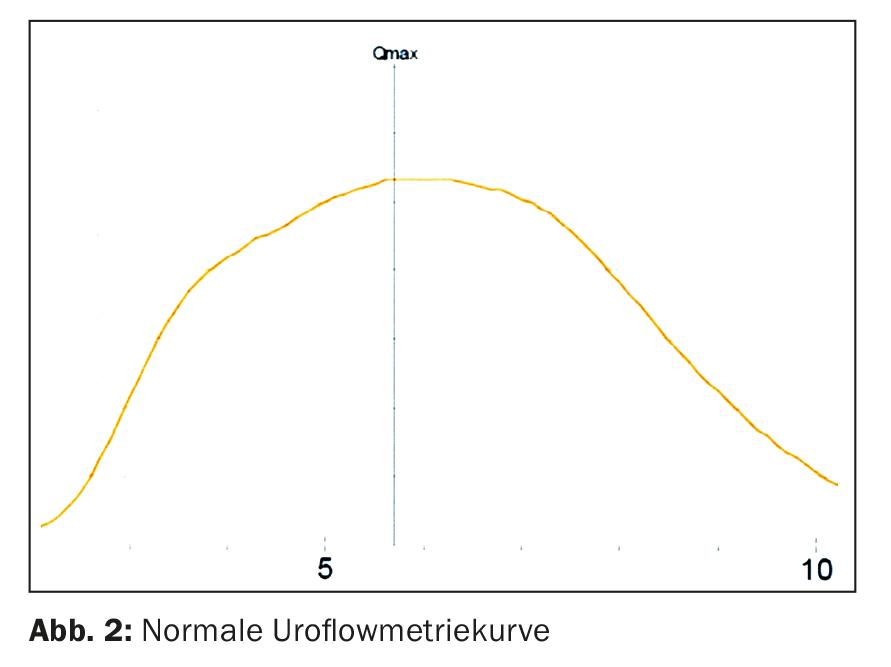
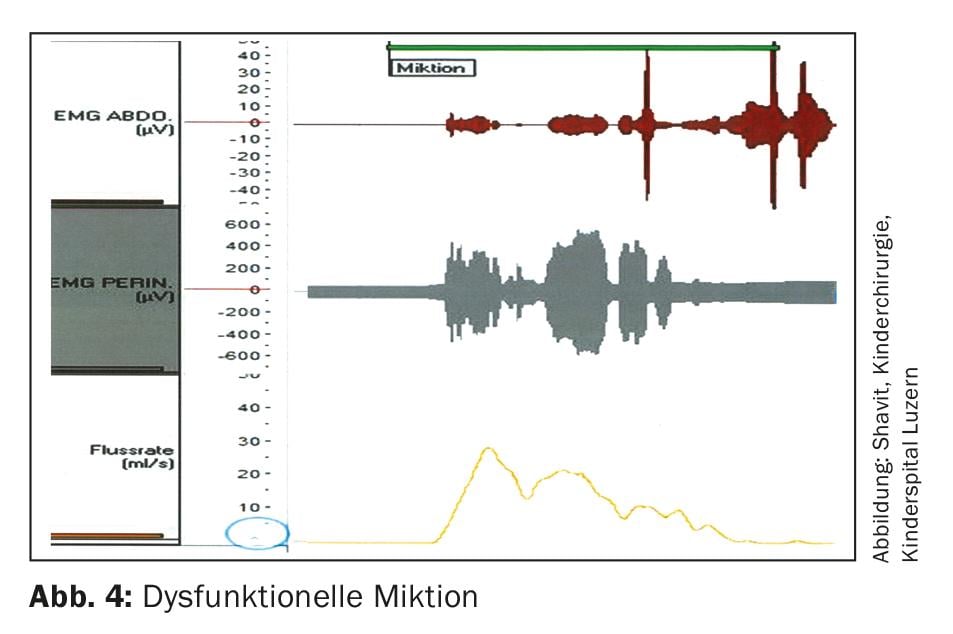
A precise micturition history including information on storage and voiding dysfunctions is required to identify micturition dysfunction (tab. 1). A micturition log over two to three days with a note of the wetting phases provides further helpful information. Family history regarding enuresis nocturna, muscular and neurological disorders should not be omitted. A physical status including genital status and a neurological status complete the clinical examination. Sonography of the kidneys and urinary tract to exclude pathology should be performed, as well as uroflowmetry with EMG derivation and residual urine determination. Uroflowmetry is an excellent screening method for lower urinary tract dysfunction (Fig. 2) . An analysis of the urine with urine status, specific gravity and, if the question is specific, a urine culture should be arranged. The detection of constipation is of utmost importance, as it negatively affects the bladder situation. Invasive examinations such as micturition cystogram, cystoscopy and urodynamic examination are performed only when specifically indicated.
Diagnoses
In case of incontinence, an organic cause (double kidneys in girls with ureters opening into the vestibule ectopic, posterior urethral valves in boys, tethered cord) must be considered, which requires an extended work-up at a specialized pediatric clinic. Functional micturition disorders with daytime and/or nighttime incontinence involve storage, voiding, or even both together. Based on the medical history and the clarifications performed, the micturition disorder can usually be well determined and the appropriate therapy can be administered. The overactive bladder manifests itself as primal symptoms with incontinence during the day and possibly also at night, an increased frequency of micturition and emptying of small portions of urine. Holding maneuvers such as leg clenching and heel sitting are used in heaps. Deferral of micturition results in infrequent micturitions and voiding of large portions of urine. In the course, an underactive bladder may occur with pressmicturization, residual urine formation, and recurrent urinary tract infections (Fig. 3).
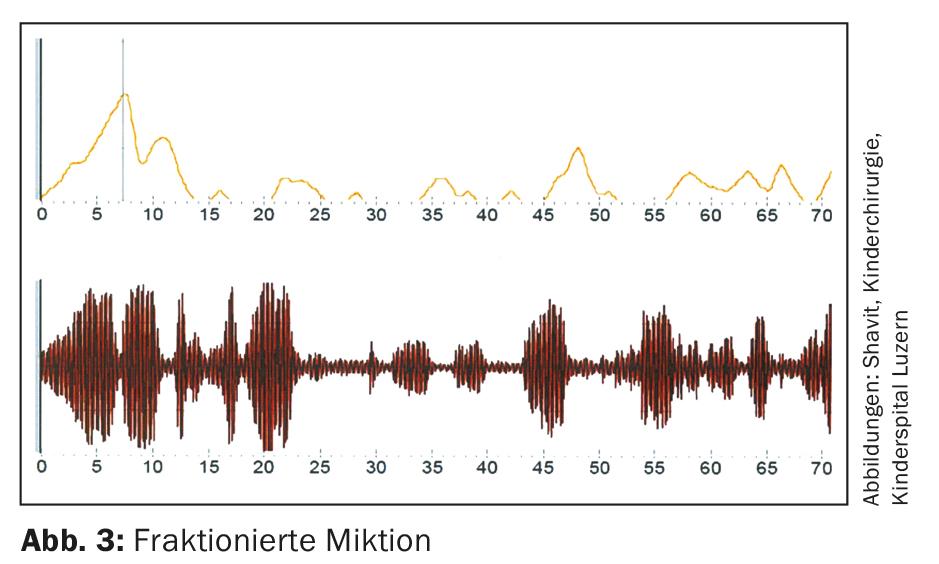
In dysfunctional micturition, there is a voiding dysfunction. During micturition, the pelvic floor is not relaxed or contracted, which is shown in uroflowmetry with EMG derivation. This leads to “staccato-micturition” (Fig. 4) with residual urine formation and recurrent urinary tract infections. Vaginal influx in girls causes incontinence during the day due to post-micturition dribbling of urine. Changing the sitting position (e.g., using the toilet astride), resting the legs on a stool, or cleaning the genitals with a little pressure on the perineum can counteract post-dripping. Stress incontinence is extremely rare in children. Children with cystic fibrosis should receive protective pelvic floor physical therapy. “Giggle incontinence” is complete emptying of the bladder during boisterous laughter. The younger the child, the more pronounced the symptoms. The genesis is not fully understood [6]. During treatment, pelvic floor physiotherapy has proven to be effective.
The “daytime only urinary frequency” syndrome is manifested by urge without incontinence. The children visit the toilet up to 30 times a day, but sleep through the night. The symptomatology appears suddenly without any apparent cause and disappears spontaneously within six to twelve months. No stress situations are found. Antimuscarinics show little effect [7].
If constipation is present, it is recommended to treat it primarily. This often improves incontinence during the day. Antimuscarinics should be used with caution because they may worsen constipation. If incontinence occurs during the day with overflow copresis, it is referred to as bladder-intestinal dysfunction [3].
Therapy
Bladder training involves going to the toilet at fixed times every two to three hours with legs propped up on a stool, even when children do not feel the need to urinate. In everyday life, going to the toilet at mealtimes has proven successful: Morning meal/”Znüni”/lunch/”Zvieri”/night meal and before going to bed.
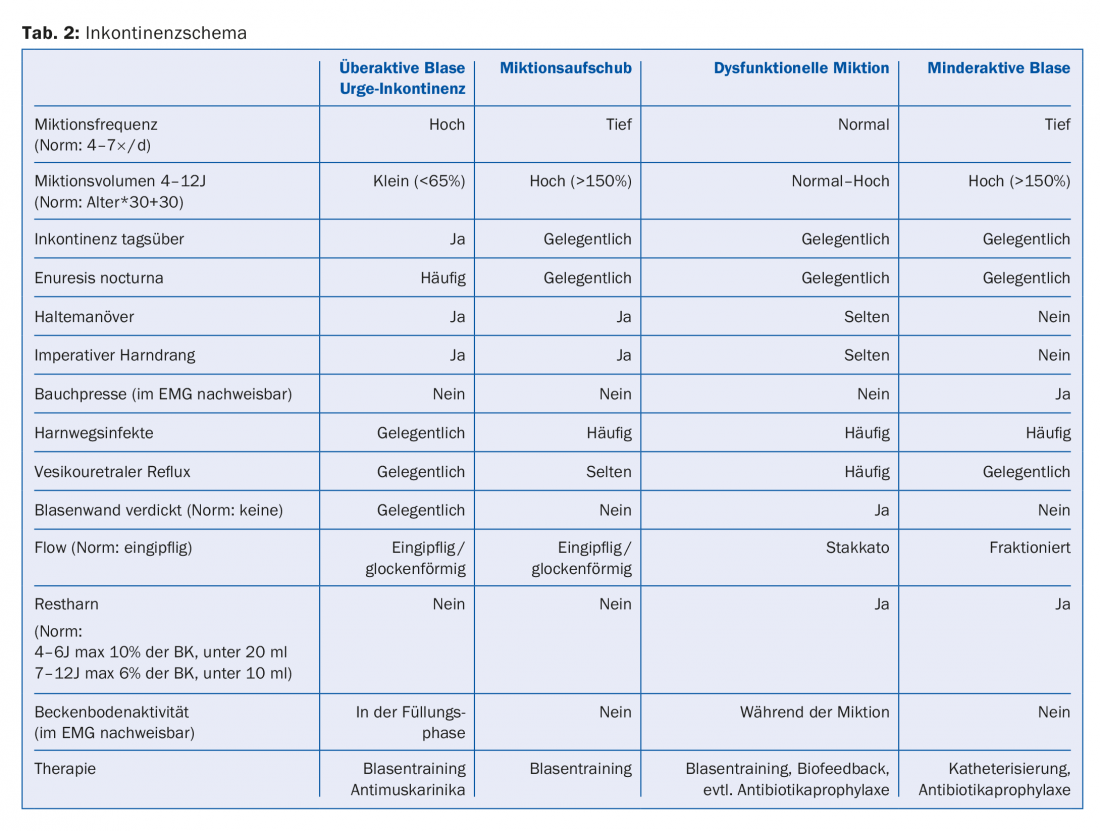
In Switzerland, the only antimuscarinic drug approved in children is oxybutynin (0.5 mg/kgKG divided into two to three doses per day). Central side effects (increased aggressiveness and/or concentration disturbances) are to be expected due to the cerebrospinal fluid (CSF) receptivity of the degradation products. It is recommended that the drug be phased in, and a discontinuation attempt should be made every four months. Transcutaneous neuromodulation over the S3 dermatome using a TENS unit with specially deposited frequencies offers a good alternative to antimuscarinic therapy with a success rate up to 70% [8]. Pelvic floor physiotherapy or biofeedback therapy for dysfunctional micturition should be performed by specially trained pediatric physical therapists. Children learn to relax the pelvic floor during micturition. The use of different therapeutic modalities improves the chances of success [9]. Table 2 summarizes the normal values and the most common micturition disorders with symptoms and treatment options.
Incontinence at night, enuresis nocturna
A distinction is made between primary and secondary enuresis nocturna. If a child has been continent at night for six months or more and begins to wet the bed again, this is called secondary enuresis nocturna. Primary enuresis nocturna is divided into monosymptomatic and non-monosymptomatic forms. Monosymptomatic enuresis nocturna is understood to be only nocturnal enuresis without the presence of other micturition disorders during the day, otherwise it is referred to as non-monosymptomatic enuresis nocturna. Approximately 10% of 7 year olds are affected, adults are still affected 1% [3,10].
Genesis
Several mechanisms play an etiologic role: increased nocturnal urine production (>130% of calculated bladder capacity), nocturnal detrusor overactivity, and delayed development of wakefulness. Enuresis nocturna occurs sporadically in about 30%, whereas it is inherited in an autosomal dominant manner in about 50% [10].
Clarification
As with daytime incontinence, a complete work-up including a micturition log and urinalysis with determination of specific gravity in fasting urine, which should be above 1015, is recommended for enuresis nocturna. In the differential diagnosis of enuresis nocturna, organic diseases such as diabetes mellitus, diabetes insipidus or uropathies must be excluded.
If secondary enuresis nocturna occurs, a psychological stress situation must be considered or the simultaneous occurrence of a micturition disorder that negatively affects the situation during the night.
Therapy
Therapeutic options include desmopressin and the arousal apparatus.
Desmopressin shows good effect in nocturnal polyuria. However, if the focus is on a functionally reduced bladder capacity, the use of the awakening apparatus is recommended. Besides conditioning, it leads to the increase of bladder capacity during the day [11].
Take-Home Messages
- Daytime wetting is considered incontinence after the age of five.
- Any constipation present must be treated first.
- Multimodal treatment of incontinence improves the chances of success.
- Behavioral problems occur in up to 30% of cases, and psychological stress situations are sought in secondary monosymptomatic enuresis nocturna.
- In cases of continuous incontinence and/or recurrent urinary tract infections and/or massive residual urine formation, referral to a specialized pediatric clinic should be made.
Literature:
- Largo RH, Gianciaruso M, Prader A: The development of bowel and bladder control from birth to 18 years of age. Schweiz Med Wochenschr 1978; 108(5): 155-160.
- Jansson UB, et al: Voiding pattern and acquisition of bladder control from birth to age 6 years – a longitudinal study. J Urol 2005; 174: 289-293.
- Austin PF, et al: The Standardization of Terminology of Lower Urinary Tract Function in Children and Adolescents: Update Report from the Standardization Committee of the International Children’s Continence Society. J Urol 2014; 191(6): 1863-1865.e13.
- Swithinbank LV, et al: The natural history of daytime urinary incontinence in children: a large British cohort. Acta Paediatrica 2010; 99: 1031-1036.
- Sillen U: Bladder Function in healthy Neonates and its Development during Infancy. J Urol 2001; 166: 2376-2381.
- Logan BL, Blais S: Giggle incontinence: evolution of concept and treatment. J Pediatric Urol 2017 Oct; 13(5): 430-435.
- Bergmann M, et al: Childhood extraordinary daytime urinary frequency – a case series and a systematic literature review. Pediatr Nephrol 2009; 24: 789-795.
- Lordêlo P, et al: Transcutaneous Electrical Nerve Stimulation in Children With Overactive Bladder: A Randomized Clinical Trial. J Urol 2010; 184: 683-689.
- Thom M, et al: Management of lower urinary tract dysfunction: A stepwise approach. Journal of Pediatric Urology 2012; 8: 20-24.
- von Gontard A, Heron J, Joinson C: Family History of Nocturnal Enuresis and Urinary Incontinence: Results From a Large Epidemiological Study. J Urol 2011; 185: 2303-2306.
- Hivistendahl GM, et al: The Effect of Alarm Treatment on the Functional Bladder Capacity in Children with Monosymptomatic Nocturnal Enuresis. J Urol 2004; 171: 2611-2614.
HAUSARZT PRAXIS 2018; 13(5): 11-14