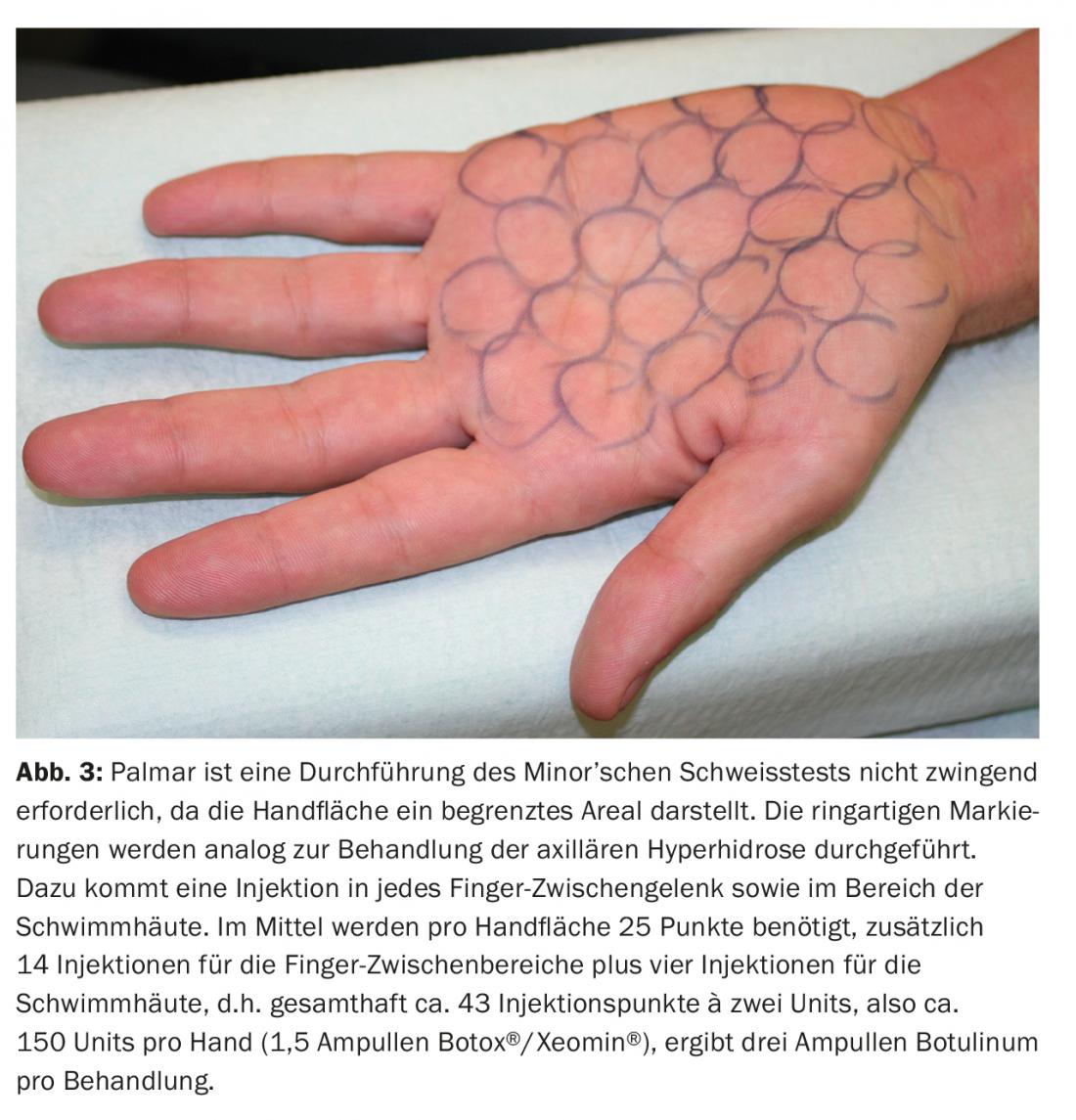
The triumph of Botox® in aesthetic dermatology would probably not have happened without the indication of focal hyperhidrosis. Per injection point, 2 U Botox®/Xeomin® resp. 6 U Dysport® applied. Circular injection marks with a diameter of 1 cm are recommended.
In this issue, I am pleased to present the fourth and final part of the botulinum continuing education course as part of the Aesthetic Dermatology continuing education series. In the first part (DP 01/2015) we discussed the basics, the second part (DP 02/2016) was dedicated to aesthetic indications in the upper third of the face, and the third (DP 04/2017) to the lower third of the face. In this fourth part of the series, we discuss the use of botulinum for focal hyperhidrosis. You are now holding the last part of the Botulinum training series in your hands. Search out the previous articles on this topic in your article archive so that you have in your hands the most comprehensive overview of the possible applications of botulinum in dermatology. If one or the other article is missing from your archive, consult the Physicians’ Continuing Education Portal www.medizinonline.ch, where all articles are available online and at any time (also as PDF).
The Aesthetic Dermatology training series will continue in the same way (basics, simple practical applications, expert applications) in the future. The next series will be dedicated to the topic of “fillers”. A “laser” series is also planned. Science comes from creating knowledge: Let’s go!
Once upon a time, long, long ago …
In 1817, Dr. Justinus Christian Kerner (1786-1862) published in the “Thübinger Blättern für Naturwissenschaften und Arzneykunde” an exact description of symptoms of patients suffering from botulism and concluded already at that time “that the fatty acid could be used for various ailments such as excessive sweating, possible increased secretion of mucus, purulent ulcerations, chronic bleeding […], similar to arsenic or chlorine!”. In the late 1960s, ophthalmologist Dr. Alan Scott sought a conservative alternative to the strabismus surgeries commonly performed at the time. In 1973, the first primate was successfully treated with the toxin for strabismus. Subsequently, it was increasingly used in other indications besides strabismus: “Ubi musculus, ibi botulinum!” In 1994, the neurologist Bushara recognized that patients treated with BTX for blepharospasm sweated less on the treated side of the face, and in 1996 he published a possible extension of the indications for BTX treatment: hyperhidrosis. In 1997, the author founded the first hyperhidrosis consultation in Switzerland at the Dermatology Clinic of the University Hospital Zurich. It can be argued that the triumph of the drug Botox® in aesthetic dermatology would not have happened without the indication of focal hyperhidrosis. Plastic surgery colleagues at the time were extremely skeptical about the drug that could replace their lifting surgeries. However, due to the indication of hyperhidrosis, the drug quickly found widespread use and the next step to use Botox® also in the face to attenuate the mimic muscles was short.
The Minor’s welding test
Minor’s welding test is a semi-quantitative measurement method for objectifying the amount of welding. The principle of the test goes back to the oxidation of potato starch and was first described by Victor Minor in 1928. The axilla is stained with Lugol’s solution (iodine-potassium-iodide solution). Then the marked area is finely dusted with potato starch. Depending on the severity of the hyperhidrosis, the area discolors to varying degrees of purple. Lugol’s solution and potato starch can be easily prepared by the local pharmacist. Alternatively, Betadine® and Maizena (corn starch) can be used, although it should be noted that the reaction with this combination is much less pronounced and it can therefore sometimes lead to false negative results. This semi-quantitative test allows the treating physician to precisely delineate the area to be treated. It is often argued that the hairy axilla area corresponds to the injection field. Unfortunately, this “rule” is only true in about two-thirds of cases. Anyone who regularly performs the Minor’s sweat test will notice that it exhibits strong interindividual variability (Fig. 1). In addition, the test also allows prognostic conclusions to be drawn. Depending on the intensity, the duration of effect of the injected botulinum can be estimated prognostically. It can be assumed that in case of a strong, dripping staining (grade IV) the effect of the botulinum treatment lasts less long than in case of a weak, hardly visible staining (grade I). However, it should be noted that the intensity of individual hyperhidrosis is physiologically variable. Thus, a low-grade minor’s sweat test by no means excludes veritable axillary hyperhidrosis. In addition, Minor’s sweat test provides essential information in the patient’s treatment process. Thus, any residual hyperhidrosis can be easily determined after therapy has been completed and followed up to the complete satisfaction of the patient. The test is cheap, easy to perform and delegable. It also helps to convey competence in your medical practice (“My doctor tested the amount of sweat!”). Minor’s sweat test is therefore indispensable in the treatment of axillary hyperhidrosis. Make it!

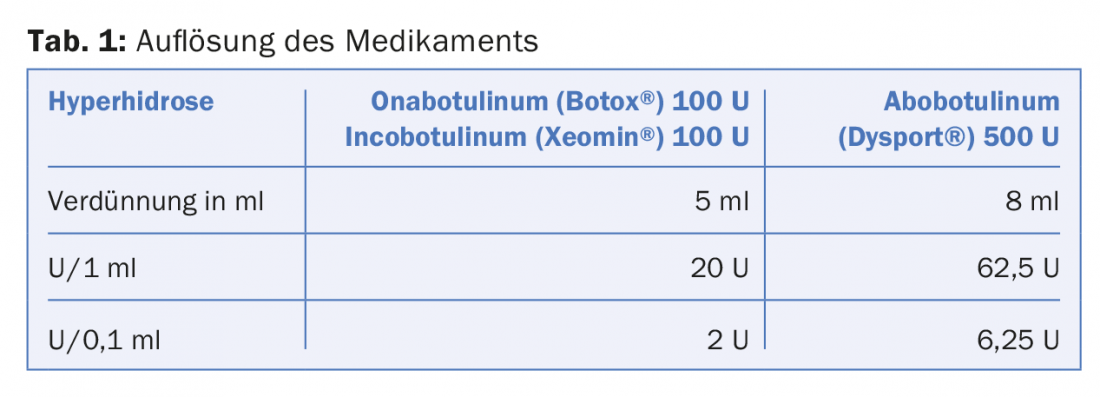
Dissolution of the drug
While a dilution of the drug with 2.5 ml NaCl has been established for the aesthetic treatment of the face, a dilution of 5 ml NaCl is recommended for the treatment of hyperhidrosis. This recommendation applies to the dissolution of 100 units ampoules of Botox® (Allergan) resp. Xeomin® (Merz Aesthetics), while 8 ml NaCl is required to dissolve 500 units ampoules of Dysport® (Ipsen). The units of Botox® and Xeomin® are bioequivalent. One unit of Botox®/Xeomin®, however, is equivalent to 2.5-3 units of Dysport®. For this reason, it is essential to adjust the dilution accordingly in the case of dysport treatment (Tab. 1) . With this conversion, it is possible to achieve the same bioequivalence per injection point (0.1 ml), regardless of which preparation is selected for treatment (ratio 1:3 = Botox®/Xeomin®:Dysport®). For less experienced users, it is recommended to stick with a botulinum preparation to avoid risky conversions.
It has been proven to use attachable hypodermic needles with a size of 30-32 gauches. This choice has the advantage that after reconstitution of the botulinum, the drawing needle (pink 18 Gauches) can be left in the ampoule and the respective 1 ml insulin syringes can be easily drawn up. Some users prefer insulin syringes with a welded-on needle. This method has the advantage that, because the needle does not have an attachment, no substance is lost during the aspiration and injection process. However, the disadvantage of this method is that the gray plastic cap of the ampoule must be removed with relative difficulty, the fine 32G needle makes it more difficult to draw up the solution, and the needle becomes blunt more quickly when it touches the wall of the ampoule. In addition, hygienic concerns must be expressed when the mounting needle is also the injection needle. Another advantage of the attached needle technique is that excess solution can be easily returned to the ampoule and storage of the drug is easier. This procedure is also harmless from a hygienic point of view, as no aspiration takes place during the injection itself.
Injection technique for the treatment of axillary hyperhidrosis
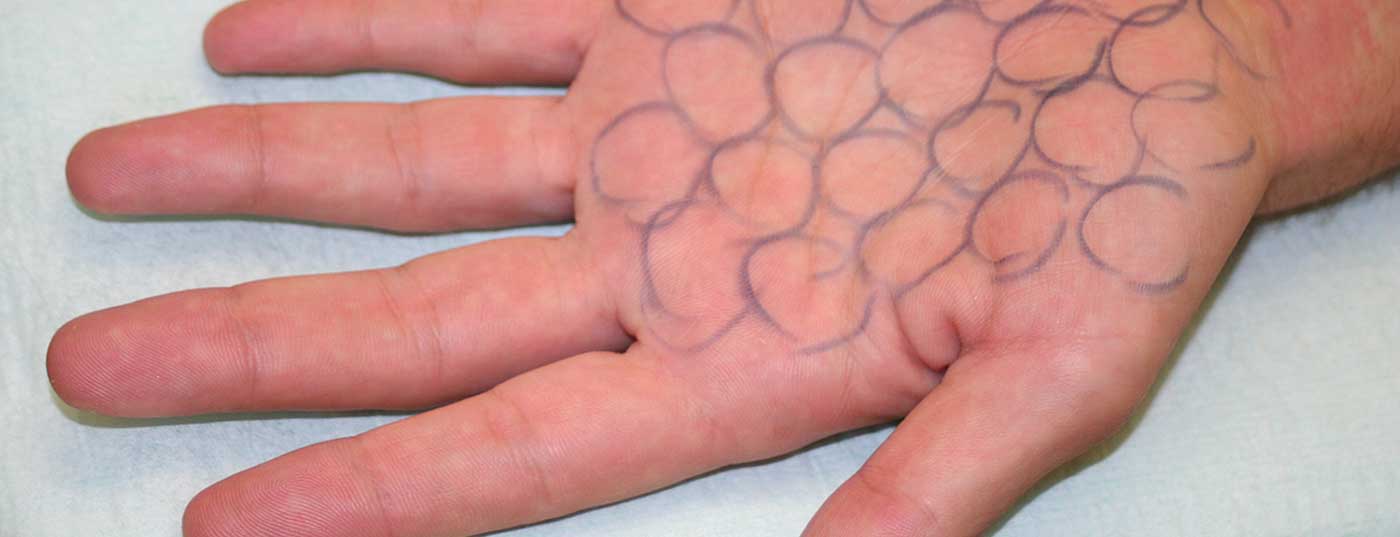
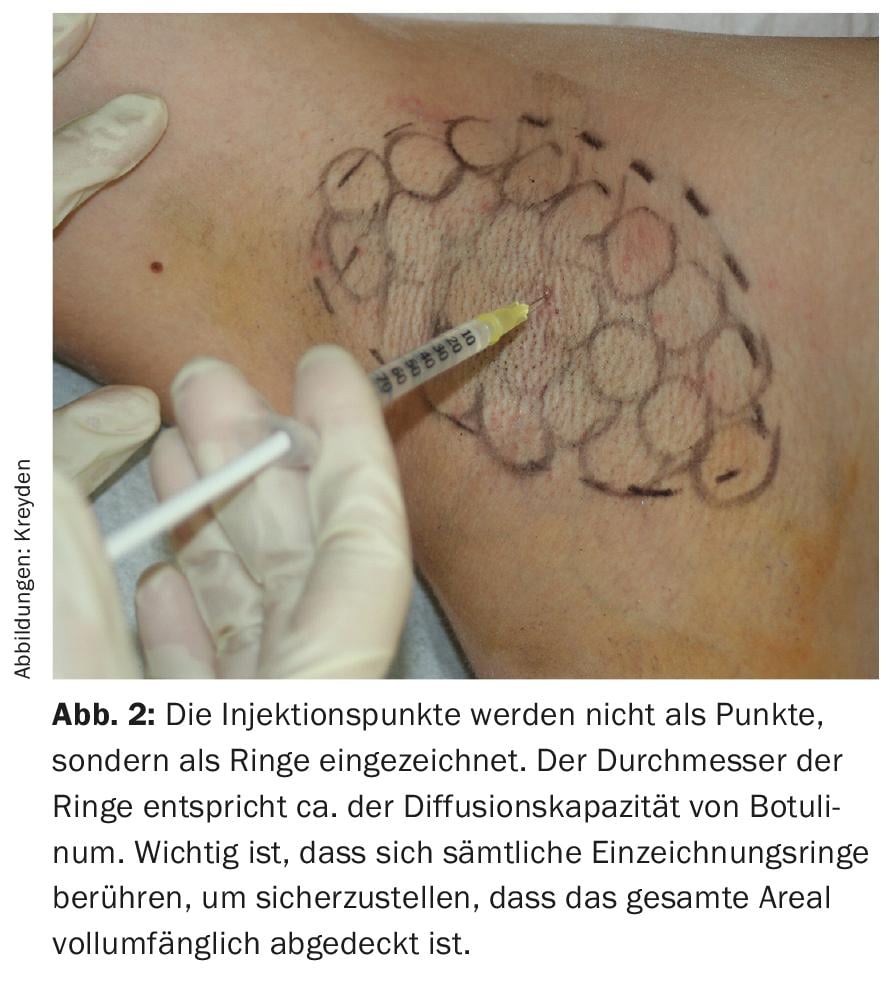
After marking the hyperhidrosis zone using Minor’s sweat test, the area to be injected is marked with a pen. Soft eyeliner pencils have proven successful for this purpose, as they withstand disinfection and can be easily and completely removed after treatment. Conventional surgical pins have the disadvantage that the markings sometimes remain visible for days after the treatment, which is not very appreciated by patients, especially in the summer months (strappy dress). It is known that the drug in the above dilution spreads about 1-1.5 cm three-dimensionally. To achieve the most comprehensive, gap-free injection possible, circular injection marks with a diameter of approx. 1 cm, paying strict attention to the fact that the marking circles touch each other respectively (Fig. 2). If only the injection points are drawn in, as recommended by other authors, the diffusion capacity of the botulinum may leave untreated streak-like residual hyperhidrosis zones – the second most common cause of an inadequate result after lack of minor’s sweat test. Regardless of which preparation is used for treatment, 0.1 ml of solution is injected per injection point, provided that reconstitution has been performed using the above scheme. This corresponds to two units of Botox®/Xeomin® resp. 6.25 Units Dysport®. Kreyden et al. were able to show as early as 2001 that two units of Botox®/Xeomin® or 6 units of Dysport® for the treatment of axillary hyperhidrosis achieve a maximum effect. The injection itself is placed subdermally. An injection angle of about 45° with a needle penetration depth of 1-2 mm is recommended.
Effective anesthesia for the treatment of palmoplantar hyperhidrosis.
The treatment of palmar or plantar hyperhidrosis is performed using the same technique as for axillary hyperhidrosis. Per injection point, 2 U Botox®/Xeomin® resp. 6 U Dysport® applied. The injection sites are also marked using the ring technique (Fig. 3). However, due to the painful palmoplantar injections, specific attention must be paid to the anesthetic technique.
In axillary treatment, no local anesthesia is actually needed because the injections are very well tolerated. In each case, about one third of the injections are hardly felt, one third are perceived as fine punctures, and only just the last third burns like a bee sting. That is why some authors recommend an occlusive EMLA® pretreatment. This can be performed without further ado, if desired by the patient.
However, treatment of palmar or even plantar hyperhidrosis is very painful. And compared to axillary hyperhidrosis, it requires about three times the amount of punctures. Thus, the therapy time (suffering time for the patient) is also correspondingly longer. Appropriate anesthesia for painful injections remains a perennially debated problem. In the literature, it is mainly the hand- or Foot block established as a standard. In some countries, intubation anesthesia is still recommended as the first choice form of anesthesia. However, this recommendation must be questioned for several reasons.
The hand block is associated with numerous undesirable effects:
- The nerve block needs training and is often incomplete
- Needle effect time can be long and often poses a logistical problem not only for the treating physician but also for the patient
- Vasovagal syncope due to anesthesia setting is common
- Due to the motor involvement, the nerve block represents a considerable discomfort for the patient for hours after application (e.g., impossibility to drive a car after the treatment).
- The risk of nerve injury, prolonged anesthesia or hypesthesia, or systemic effects (anaphylaxis, cardiac complications) must not be underestimated
- Due to the limiting duration of action of BTX, the nerve block must be repeated at regular intervals.
Thus, various alternative local anesthetic methods were tried by the author.
EMLA® under glove occlusion: The one-hour preceding occlusive glove application of EMLA® shows sufficient anesthesia for the puncture itself. For burning injection pain, this form of anesthesia is insufficient. In addition, glove occlusion causes the hands or feet to swell considerably (maceration), which can lead to imprecise injection depth of the botulinum to be applied and, in turn, to varying results. For this reason, this form of anesthesia can only be recommended to a limited extent.
Cold treatment by ethylene spray: this form of anesthesia has become widely used for the treatment of thrombosed hemorrhoidal nodes in anal surgery. Commercially available ethylene spray is used to superficially freeze the area to be treated prior to incision. In the treatment of palmoplantar hyperhidrosis, liquid ethylene has been shown to tend to freeze the entire hand of the patient. Thus, this form of anesthesia is not recommended due to its imprecision.
Precise cold anesthesia by means of cryotherapy (according to Kreyden): Known from classical dermatology, highly precise cold treatment by means of cryotherapy succeeds (e.g. actinic skin damage, verrucae vulgares). After less successful ethylene treatment trials, this anesthetic treatment actually seemed obvious. Directly before the injection, the marked injection site is anesthetized very precisely with superficial cold anesthesia (Fig. 4). With this form of pain control, both pain sensations (puncture and burning injection pain) can be effectively addressed. In an observational study, treated patients reported a pain score of 3-4 (minor pain) on a pain scale of 1-10 (maximum pain 10 points). However, it became apparent that this form of anesthesia also has disadvantages. On the one hand, the treatment itself is not painless (pain sensation of 3-4) and on the other hand, therapy-typical post-interventional blistering with prolonged punctate erythema may occur. Patients complained of explanatory distress about their palms being stippled in this way. To avoid this undesirable side effect, the choice of cryotherapy nozzle is critical. In order to achieve the most superficial treatment possible, this should have the smallest possible diameter (CryoPro® nozzle D). Additionally, a 10-hole nozzle is commercially available, designed primarily to enhance laser applications by spraying a cold mist to mitigate heat sensations. This special 10-hole nozzle succeeds in setting a superficial frost in the area of the puncture site instead of spot freezing of the skin, thus effectively preventing blister formation. To minimize the pain sensation of the cryotherapy itself, it is recommended that iontophoresis therapy with 2% lidocaine solution be applied directly beforehand. With transdermal iontophoretic application of 2% lidocaine, satisfactory anesthesia was achieved in children before the placement of an intravenous catheter. Combining both forms of anesthesia and using a very superficial cryotherapy (10-hole nozzle), a virtually painless treatment with few side effects can be performed.
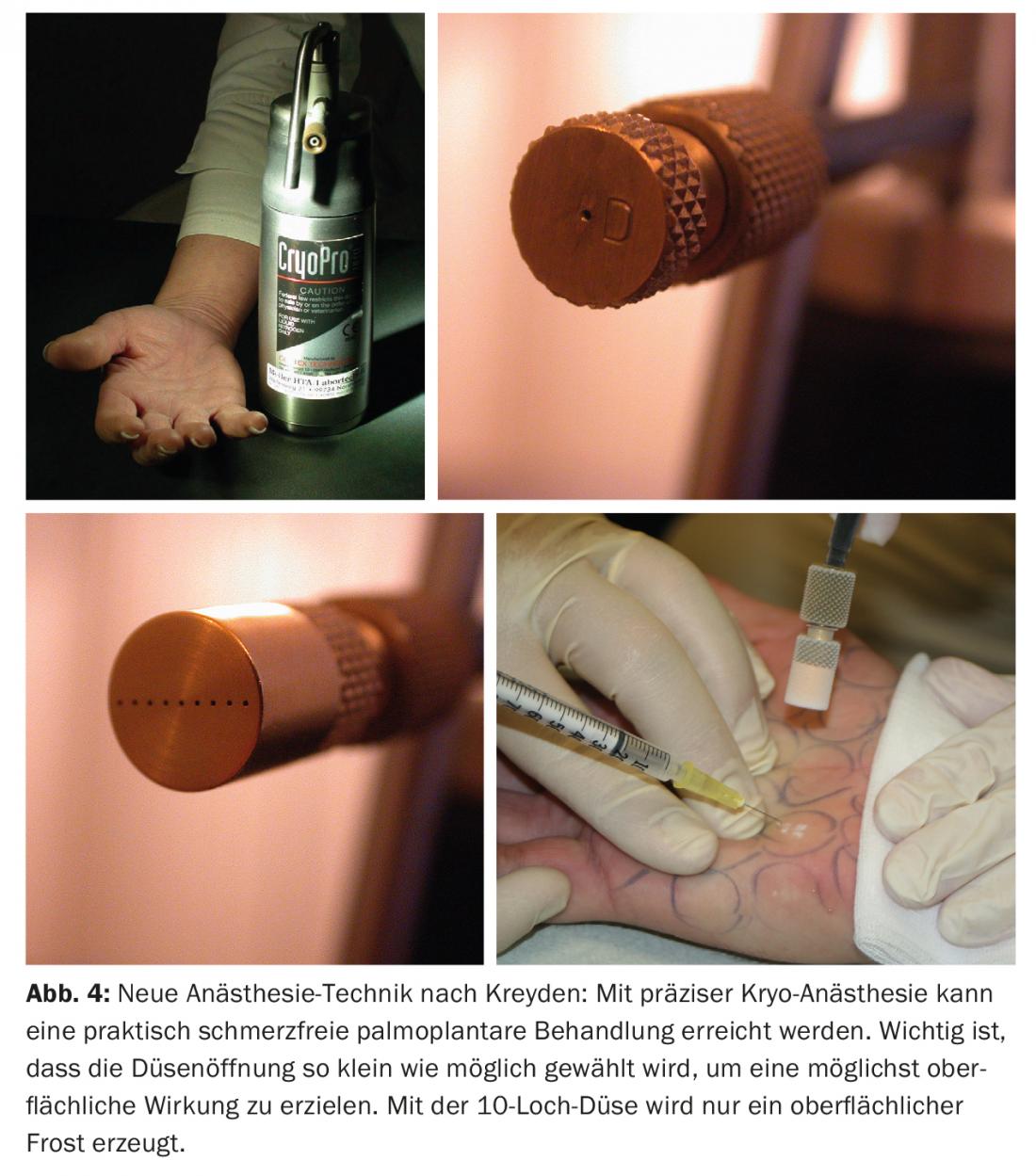
At most, the need for assistance can be mentioned as a disadvantage of this anesthetic technique. In practiced hands, however, palmar treatments are possible within a few minutes, and further time-consuming treatment steps with side effects are unnecessary. It is this technique that allows the unhesitating extension of botulinum treatment beyond the axillary indication to the otherwise somewhat more difficultly classified palmar and even plantar treatment.
Rarer indication of focal hyperhidrosis.
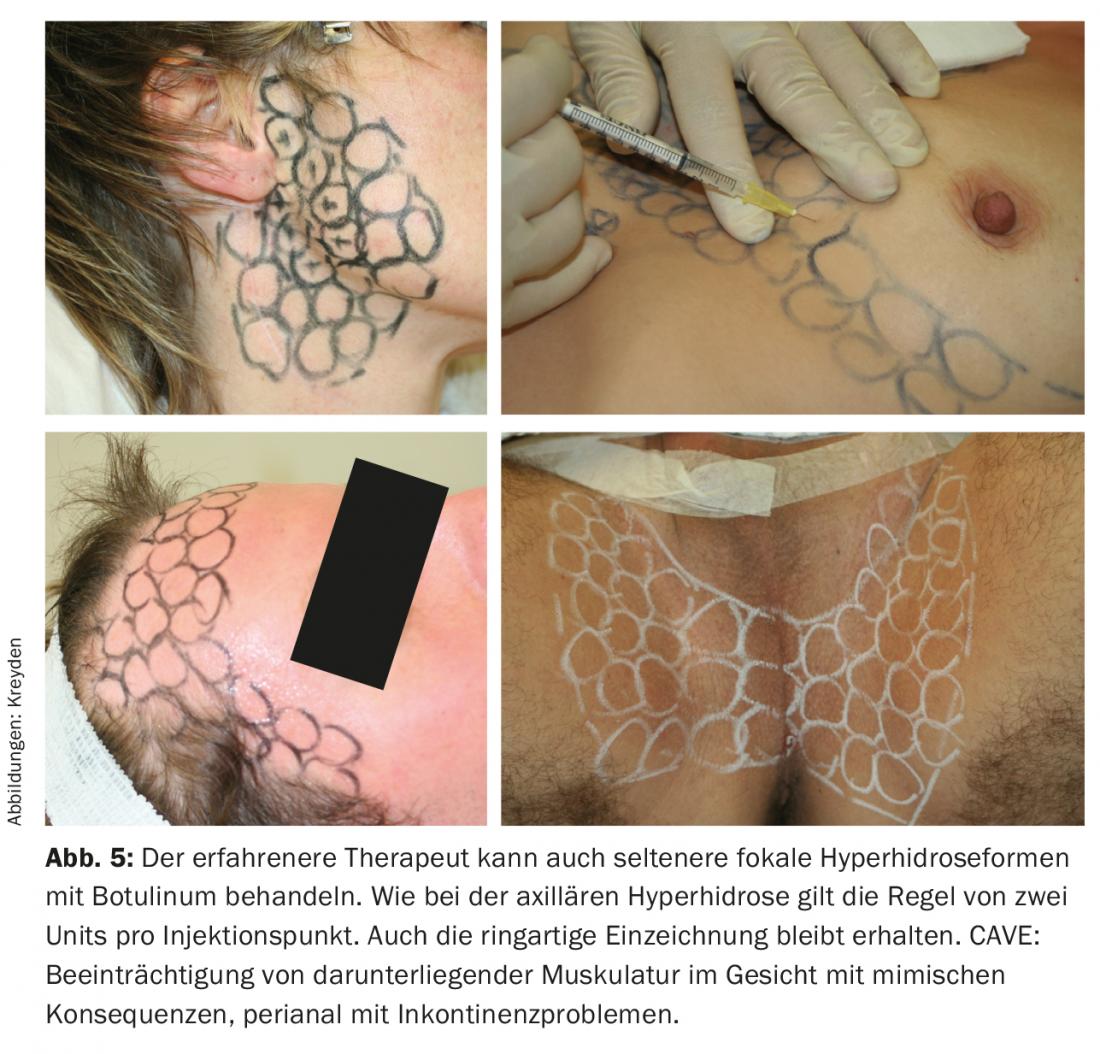
By far the most frequent indication for botulinum treatment is certainly axillary hyperhidrosis, followed by hand sweating. The only indication approved by Swissmedic is axillary hyperhidrosis. In other words, all treatment areas outside of axillary hyperhidrosis are so-called “off-label” applications and represent a treatment attempt in purely legal terms. Other areas of sweating include frontal and/or nuchal hyperhidrosis, submammary and/or intermammary hyperhidrosis, or inguinal, less commonly perineal resp. perineo-anal hyperhidrosis. The so-called Frey syndrome (gustatory sweating, syndrome of the auriculotemporal nerve) is a rare entity usually after surgical intervention of the parotid gland (less frequently after inflammation) and is characterized by increased sweating during eating, due to misdirection of salivomotor parasympathetic fibers after trauma.
All rarer forms of focal hyperhidrosis (Fig. 5) can also be treated with botulinum, whereby, analogous to the axillary and palmoplantar therapy regimen, two units per injection point are sufficient. Depending on the localization of the injection points, impairment of mimic function may occur as a side effect. This is particularly important to consider in the treatment of Frey’s syndrome, but also in the treatment of frontal hyperhidrosis. For this reason, such treatments should be reserved for physicians with extensive experience in the use of the drug botulinum.
Take-Home Messages
- The triumph of Botox® in aesthetic dermatology would probably not have happened without the indication of focal hyperhidrosis.
- Minor’s welding test is a semi-quantitative measurement method for objectifying the amount of welding. The principle of the test goes back to the oxidation of potato starch. It is indispensable in the treatment of axillary hyperhidrosis.
- In order to achieve an injection with as few gaps as possible, circular injection markings (diameter 1 cm) are recommended, with the marking circles touching each other in each case.
- Per injection point, 2 U Botox®/Xeomin® resp. 6 U Dysport® applied.
- With directly preceding iontophoresis therapy with 2% lidocaine solution and a very superficial cryotherapy (10-hole nozzle), botulinum treatment can be extended beyond the axillary indication to the otherwise somewhat more difficultly classified palmar and even plantar treatment.
DERMATOLOGIE PRAXIS 2017; 27(6): 29-33