Early detection of breast cancer still offers the best chance of cure. Mammography is the benchmark for screening, but is subject to technical, logistical, and diagnostic limitations. For this reason, research is being carried out at full speed on various test methods to detect the disease as early as possible.
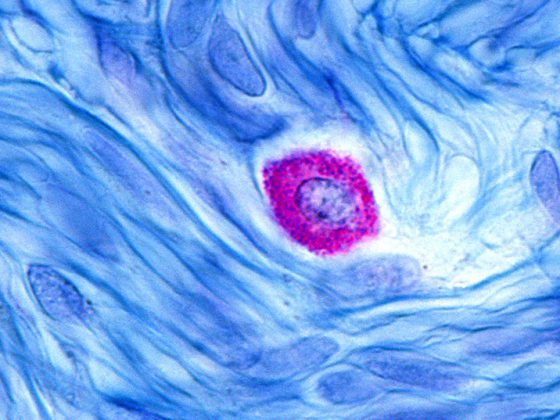
An effective and accurate blood test to detect early stages of disease should increase the early detection rate for breast cancer. Therefore, a series of lipid studies were performed in early breast cancer patients and the datasets were combined using machine learning-based analysis to test whether these profiles in plasma could detect breast cancer [1]. Blood samples were collected from women with stage 0-IV breast cancer (4 separate cohorts) and age- and BMI-matched breast cancer-free controls. Lipids from plasma-enriched extracellular vesicles were extracted and analyzed by high-resolution, precision mass LC-MS. Commercially available software was used to annotate and quantify >400 manually curated lipid species. After variable selection, a lipid signature was identified to distinguish breast cancer samples from control samples. Plasma samples from women with breast cancer were discriminated from controls with an average cross-validated accuracy of 0.81 and an average AUC of 0.84 across 4 cohorts. An optimized cross-cohort subset of early-stage IDC, DCIS, and ILC was distinguished from controls with a cross-validated AUC of 0.90, sensitivity of 0.88, and specificity of 0.82 (201 early-stage breast cancer, 199 controls). For this optimized cohort, our assay achieved a sensitivity of 0.71 with a prescribed specificity of 0.90 and a sensitivity of 0.89 with a prescribed specificity of 0.80, respectively. Accordingly, the study demonstrated high sensitivity and specificity of a lipid biomarker signature with potential for early detection of breast cancer.
When the use of bisphosphonates is indicated
Amplification of the transcription factor MAF gene has been associated with increased bone metastases in breast cancer. In addition, patients without MAF amplification in the primary tumor were shown to be more likely to benefit from adjuvant bisphosphonates. A genomic signature could identify patients who lack MAF amplification as candidates for adjuvant bisphosphonates. Therefore, genes that could predict MAF amplification status were investigated [2]. Because MAF amplification is associated with a high risk of bone metastases, a 70-gene signature for risk of distant recurrence (MammaPrint/MP) and an 80-gene signature for molecular subtyping (BluePrint/BP) were used to stratify patient groups. A total of 166 BC patients were enrolled in this pilot cohort. Fluorescence in situ hybridization was performed to detect MAF copy number. A signal-to-core ratio (SNR) of ≥2.5 was used as the threshold for MAF-amplified (MAF+). Differential gene expression analysis was performed with R limma using whole-genome microarray data. MAF+ and MAF- (SNR<2.5) were compared in all patients and in patients matched by MP/BP to balance high-risk groups. Differentially expressed genes (DEGs) were defined as absolute fold change ≥2 and adjusted p-value <0.05. Prediction of MAF amplification based on gene expression was performed using a correlation-based metric with a training set and 1179 stage I-III BC patients from the FLEX study (NCT03053193), which includes MP/BP assays and full transcriptome data.
Of the 166 patients, 12% were MAF+ and 88% were MAF-. Of the MAF+ patients, 95% were MP high-risk patients, as expected based on the association of MAF amplification and bone metastases, as opposed to 29% of MAF- patients. Of note, there was no significant correlation between amplification and MAF gene expression, underscoring the importance of using other genes to predict MAF amplification. When comparing the whole transcriptome of MAF+ and MAF- patients, 48 DEGs were found. From the MP/BP comparisons, genes with a ≥2-fold change were included in the final group of 57 genes, with enrichment of genes encoding C-X-C motif chemokine ligands and S100 calcium binding protein. The 57-gene classifier for MAF status achieved 92% accuracy, 94% specificity, and 75% sensitivity in the training group. Interestingly, when the classifier was applied to the FLEX cohort, 12% MAF+ cases were identified, similar to the training group.
Congress: ASCO Annual Meeting
Literature:
- Kehelpannala C, Pascovici D, Li D, et al: Detection of early-stage breast cancer in women by plasma lipidomic profiling. J Clin Oncol 40, 2022 (suppl 16; abstr 554).
- Nasrazadani A, Gomez Marti JL, Hyder T, et al: Investigation of a genomic signature for transcription factor MAF gene amplification and lack of bisphosphonate benefit in early breast cancer. J Clin Oncol 40, 2022 (suppl 16; abstr 559).
InFo ONCOLOGY & HEMATOLOGY 2022; 10(3): 20 (published 6/20/22, ahead of print).