Bridging therapy with glucocorticoids (GC) as a temporary part of initial treatment for rheumatoid arthritis (RA) helps to rapidly suppress disease activity. However, it is suspected that patients who have received bridging take more GC in the further course than non-bridgers. Dutch researchers now wanted to find out whether this is fact or myth.
Glucocorticoids (GC) and GC bridging have been the subject of discussion for decades. Even the international guidelines on this topic are currently not uniform, stated Lotte van Ouwerkerk, Department of Rheumatology, Leiden University Medical Center, Netherlands [1]: The 2022 EULAR recommendations recommend the use of csDMARDs (preferably MTX) for the treatment of RA patients at the outset. Bridging with GC (oral or parenteral) could be considered. However, tapering and discontinuation of GC bridging is recommended as soon as clinically possible (preferably within three months). The focus is on the rapid suppression of disease activity. In contrast, the 2021 ACR guideline does not recommend GC bridging as an initial therapy due to the risk of adverse events and concerns regarding long-term use. However, this is a conditional recommendation based on expert opinion.
To gain more clarity, van Ouwerkerk and her research group first conducted a systematic literature review and meta-analysis to determine what is known about the long-term use of glucocorticoids after GC bridging. They found that no observational studies with sufficient information on GC bridging were available. There were ten clinical trials with GC bridging in at least one study arm, which showed that 10% of patients were still taking or returning to GC after 24 months.
Contradictory results
In a second step, the scientists then initiated an IPD meta-analysis (box) . They used data from seven clinical trials previously identified through the systematic literature search: Patients who started GC bridging (35 weeks on average) were less likely to still be taking a GC after bridging (0.18) and decreased over time after two years (0.07). However, other research suggests that after bridgers stop bridging, they continue to use more GC than non-bridgers.
| Individual Patient Data IPD stands for Individual Patient Data. An IPD meta-analysis is a special type of meta-analysis in which the raw data are used, i.e. the individual patient data, and not the aggregated data as in a normal meta-analysis. Mixed-effects regression analysis with the study arm as a random effect is used to correct for the obvious differences between the study designs. |
To find out what is really true, van Ouwerkerk et al. the use of GC after a bridging phase between RA patients in randomized clinical trials that either started with initial GC bridging or not.
The primary endpoint of their IPD meta-analysis was oral GC use at 12, 18 and 24 months from baseline. Secondary endpoints were
- the mean oral cumulative GC dose (with and without bridging) up to month 24,
- the continuous (≥3 months) use of GC (yes/no) at any time between the end of the bridging plan and month 24,the number of relapses (DAS28 increase >1.2 or ∆DAS28 >0.6 and ≥3.2 at the last visit),
- of the DAS28 over time and
- the number of DMARD changes (adding a DMARD or switching between DMARDs).
The last point was of particular interest to the scientists because the DMARD changes can be a burden for the patients and it probably also saves costs if the DMARD does not have to be changed so often.
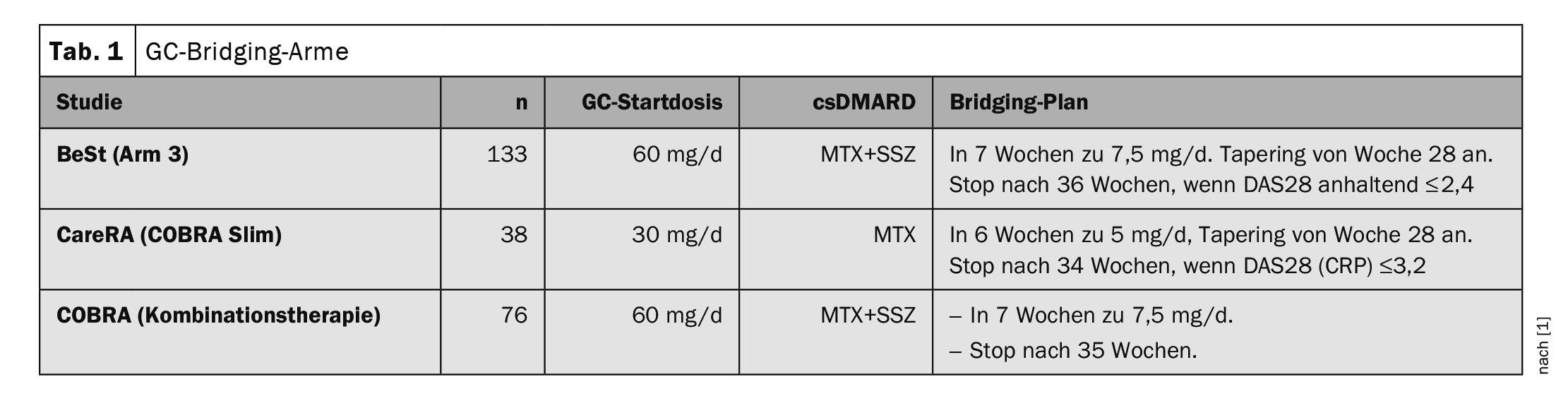
Significant difference – but only in the first year
Three of the seven studies (BeSt, CareRA and COBRA) included at least one study arm with GC bridging plus csDMARD and one study arm with csDMARD but without GC bridging. A total of 625 patients were included, of whom 40% (n=252) were randomized to GC bridging. All 3 studies started with GC bridging treatment at a high dose of 60 mg/day or 30 mg/day, but this was quickly reduced to a lower maintenance dose (Table 1). The non-bridging arms of the studies each used MTX or sulfasalazine (SSZ) as monotherapy.
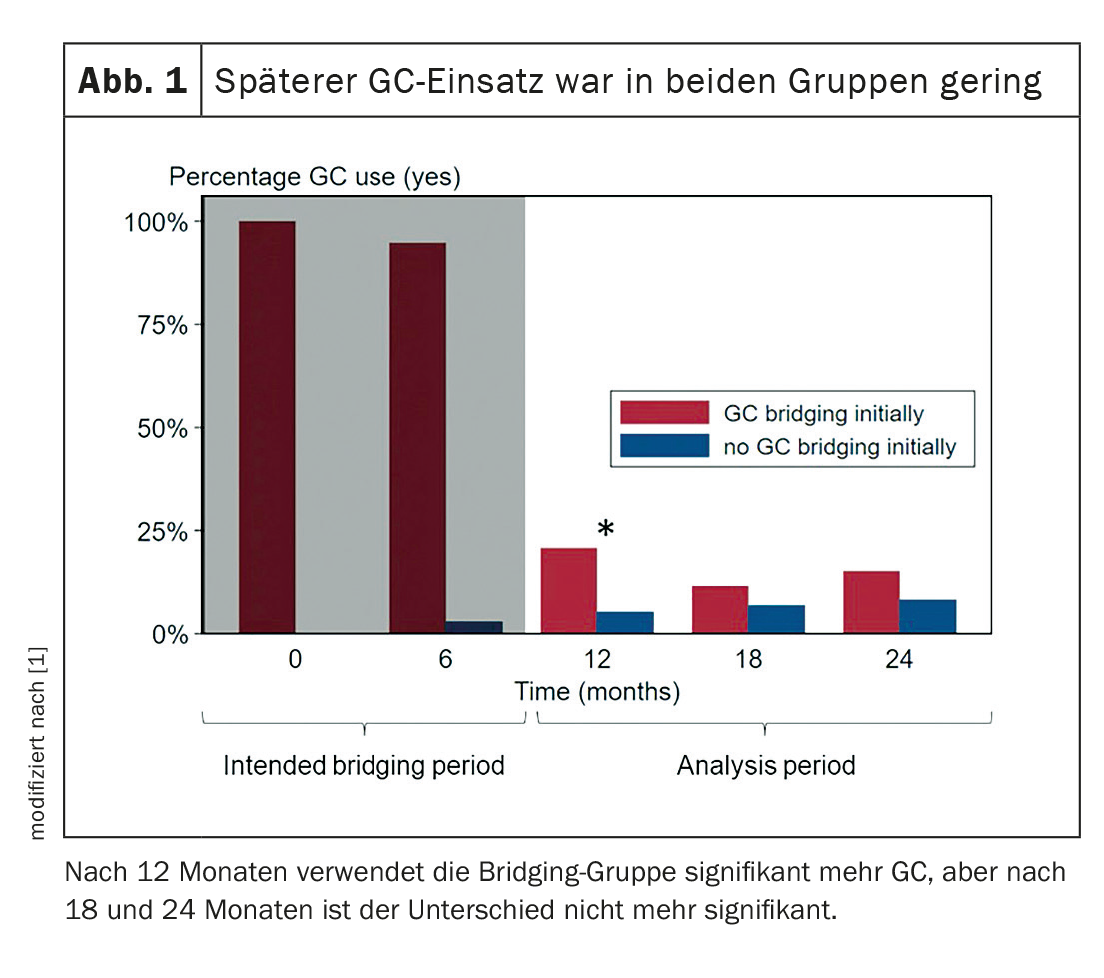
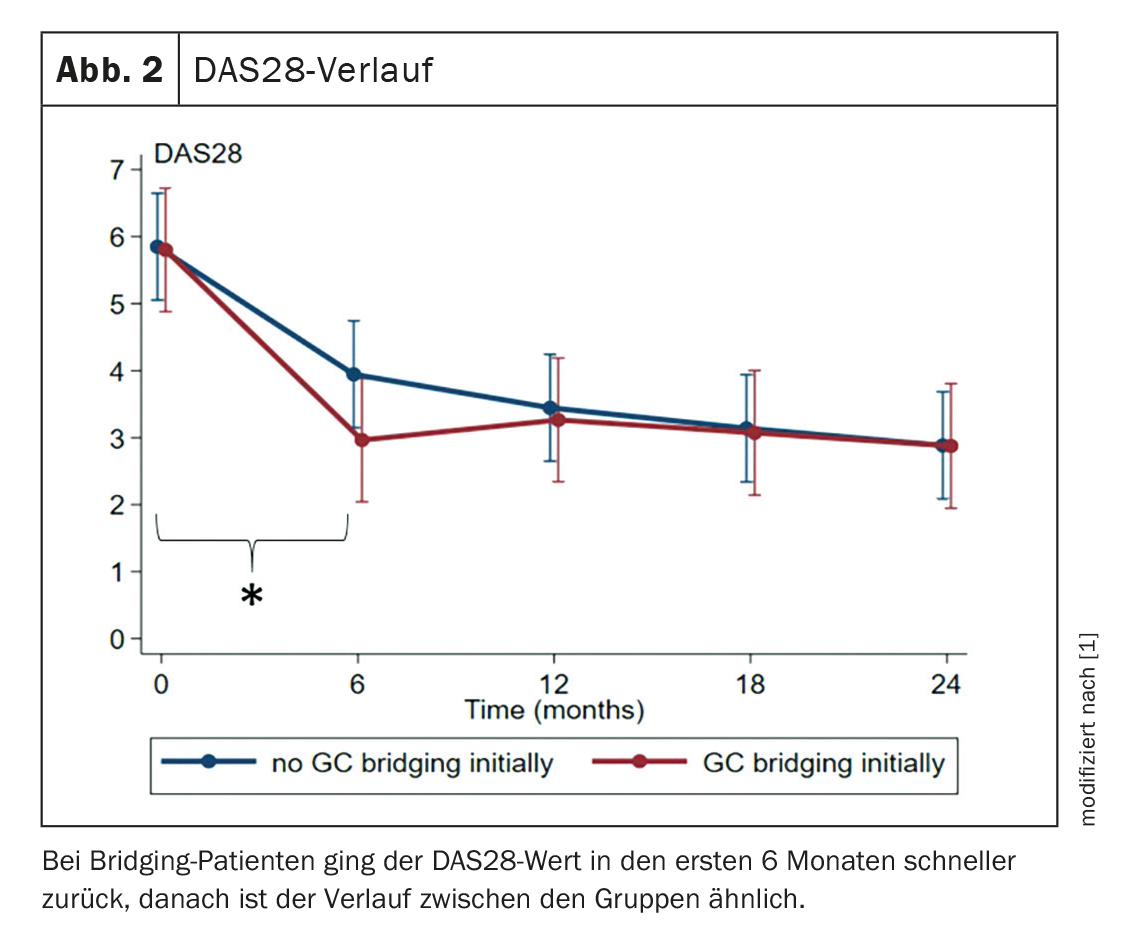
The results showed that the bridging patients used significantly more GC after 12 months compared to the non-bridgers (OR 3.3). Although there was still a difference after 18 and 24 months, it was no longer significant (Fig. 1). The DAS28 value decreased significantly faster in the GC bridging group in the first six months. Thereafter, however, the groups converged (Fig. 2). The mean cumulative GC dose after 24 months without consideration of the initial bridging regimens did not differ significantly between the groups (365 mg; 95% CI -62; 793). However, if the bridging period is included, there is a significant difference in the mean cumulative GC dose between the groups, with the bridgers using more GC (2889 mg; 95% CI 1812; 3967; this corresponds to a difference of 4 mg per day over two years). The bridgers also took the GC for longer after the bridging phase, but required fewer DMARD changes (IRR 0.59; 95% CI 0.38; 0.94).
The rheumatologists also performed a sensitivity analysis that included only patients from the CareRa study with a high risk of poor prognosis and was based on ACPA, rheumatoid factor and DAS28. The sensitivity analysis showed similar results to those of the main analysis, only the DMARD changes are no longer significantly different.
“We see the benefits of glucocorticoid bridging with faster clinical improvement in the first six months and fewer DMARD changes over time,” concludes van Ouwerkerk. However, discontinuation can sometimes be delayed. After the initial GC intake, there were no further effects of the glucocorticoids from year 1. At the end of the bridging periods, there were no differences in mean DAS28 score, number of disease relapses (by study definition) or cumulative glucocorticoid dose after the bridging phase, but the bridgers had a faster decline in DAS28 score in the first six months (during the bridging phase).
Source:
- van Ouwerkerk L: Vortrag «Initial glucocorticoid bridging in rheumatoid arthritis: does it affect glucocorticoid use over time?»; EULAR 2023, Mailand, 2.6.2023 (online).
InFo RHEUMATOLOGIE 2023; 5(2): 28-30