Low physical fitness and muscle strength in early adulthood are risk factors for cardiovascular disease (CVD). However, it is unclear how these factors relate to subclinical atherosclerosis because of the lack of longitudinal studies. A recently published study has now investigated whether physical performance and muscle strength in early adulthood are related to subclinical atherosclerosis in later adulthood.
Both physical fitness [2,3] and muscle strength [2,4] are predictors of future CVD risk and mortality. Sarcopenia, which includes muscle strength, and CVD have been shown to share common pathogenic pathways, with atherosclerosis playing a central role [5]. Nevertheless, the relationship between physical performance and muscle strength and subclinical atherosclerosis is less clear. A recent study showed that higher exercise capacity was associated with a lower risk of subclinical atherosclerosis after adjusting for confounding factors [6]. In addition, muscle strength has been shown to be associated with subclinical atherosclerosis in various populations, [7,8] independent of other CVD risk factors [8]. Further studies have also shown that middle-aged athletes have a higher prevalence of coronary atherosclerosis than their less active peers [9]. However, these studies are cross-sectional and limited by the risk of reverse causality. There is a clear lack of longitudinal studies with sufficient follow-up that have examined the association between physical performance and muscle strength in early adulthood and subclinical atherosclerosis in later adulthood. Therefore, the aim of a recently published study was to determine, first, the associations between maximal exercise capacity and muscle strength in early adulthood and the presence of plaques and carotid intima-media thickness (cIMT) in later adulthood and, second, whether these associations are mediated by CVD risk factors in early or later adulthood in Swedish men [1].
The study included Swedish men (n=797) eligible for conscription (~18 years) who participated in the baseline assessment of the Visualization of Asymptomatic Atherosclerotic Disease for Optimal Cardiovascular Prevention (VIPVIZA) trial between 2013 and 2016 (60 years). VIPVIZA is a pragmatic, open-label, randomized controlled trial comparing the effect of traditional communication based on individual CVD risk factors plus pictorial information about an individual’s subclinical atherosclerosis on CVD prevention [10]. At enlistment (~18 years), isometric muscle strength (dynamometer) and maximal exercise capacity (maximal load-cycle ergometer test) were measured. In later adulthood (60 years), the presence of carotid plaque and intima-media thickness were determined using high-resolution ultrasound.
Statistical analysis
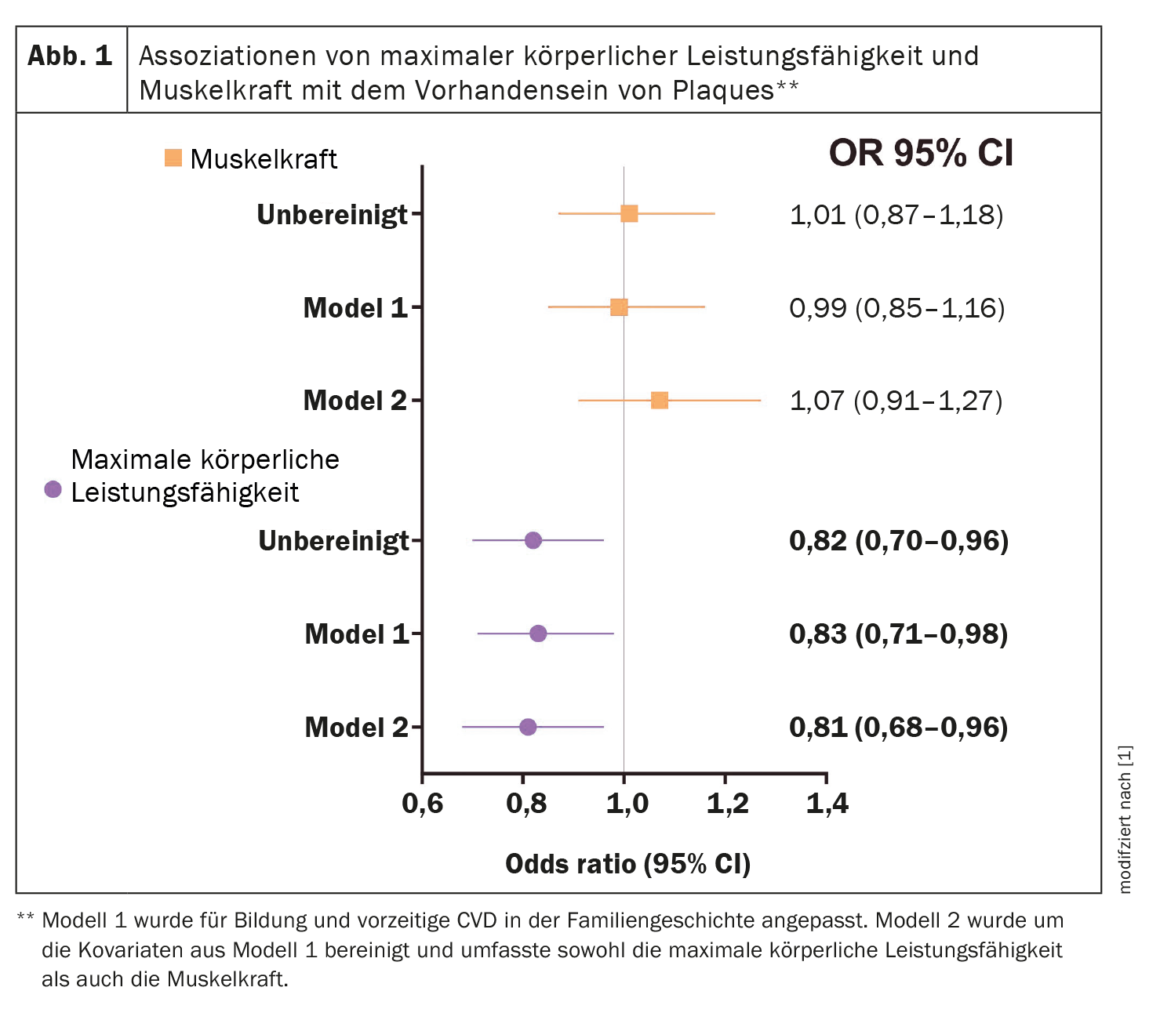
Logistic regression models were used in the main analysis to determine whether physical performance and muscle strength were associated with the presence of plaques. The associations of physical performance and muscle strength with cIMT were assessed using two approaches: (i) linear regression with continuous cIMT and (ii) Logistic regression with dichotomized cIMT, using ≥ the 75th percentile as the presence of subclinical atherosclerosis; this corresponds to a value of 0.91 mm. Model 1 was adjusted for education and premature CVD in family history. Model 2 included both physical fitness and muscle strength in addition to the covariates of model 1 to determine the independent association of these predictors with subclinical atherosclerosis.
Further analyses included a secondary analysis examining the relationship between each muscle strength variable (handgrip, knee extension, and elbow flexion) and the presence of plaques as well as cIMT. In the main analysis, maximum physical capacity and muscle strength were assumed to be a precursor of BMI. However, BMI, body weight, or height may also confound the association of muscle strength and maximal exercise capacity with subclinical atherosclerosis. Therefore, the following sensitivity analyses were performed: (a) inclusion of either BMI in early adulthood or (b) body weight in early adulthood; or (c) of weight and height in early adulthood into all models.
Descriptive features
At follow-up, 62% (n=493) of participants had plaques and had a median cIMT of 0.78 mm [interquartile range (IQR) 0.23]. In early adulthood, 82% (n=654) of men were of normal weight (BMI ≥18.5 and <25 kg/m2) and only 6% (n=48) were overweight or suffered from obesity (BMI ≥25 kg/m2). Strikingly, men with high physical fitness and high muscle strength were taller and had higher BMIs than men with lower physical fitness and lower muscle strength, a difference that persisted into later adulthood. In addition, men with high physical fitness had higher HDL cholesterol and lower triglycerides in early adulthood and were more likely to meet physical activity recommendations in later adulthood than men with lower physical fitness. In addition, men with high exercise capacity were also more likely to have no plaques (41.4%, n=171) than men with low exercise capacity (34.6%, n=133, p=0.049).
Connection between plaques
Higher physical fitness was associated with a 17% lower odds (OR** 0.83 [95% CI# 0.71-0.98, p=0.024]) of having plaques in later adulthood (model 1), adjusted for education and family history of premature CVD. This relationship remained after adjustment for muscle strength, p=0.017 (Model 2). In none of the models was a significant relationship found between muscle strength and the presence of plaques (Fig. 1) [1].
** OR=Odds Ratio
# CI=confidence interval
Intima Media Thickness Associations
There was a significant nonlinear relationship between physical performance and continuous cIMT, independent of muscle strength (nonlinear p-value=0.027), but no significant relationship with dichotomized cIMT. No significant relationship was found between muscle strength and continuous or dichotomized cIMT.
Mediation and secondary analysis
In the multi-mediator analysis, the association between exercise capacity and the presence of plaques was not mediated by BMI and systolic blood pressure in early adulthood, the 95% confidence intervals of the total indirect effect were equal to zero, and the direct effect remained significant (OR 0.80, p=0.011). Interestingly, the association between exercise capacity and the presence of plaques was mediated by the combination of BMI, systolic blood pressure, non-HDL cholesterol, triglycerides, and glucose tolerance status in later adulthood (the overall indirect effect was significant, whereas the direct effect was not [OR 0.85, p=0.080)], but this association was not mediated by a single factor. In addition, no significant association was found between handgrip strength, knee extension, and elbow flexion and the presence of plaques or cIMT.
Sensitivity analysis
In the multiple imputation analysis, the significant association between exercise capacity and the presence of plaques remained, and the nonlinear association with cIMT was no longer significant. The nonsignificant associations between muscle strength and subclinical atherosclerosis persisted after imputation of missing values, except for the associations of dichotomized cIMT. Muscle strength was associated with a 21% increased likelihood of having a cIMT using > the 75th percentile (OR 1.21, 95% CI 1.03-1.42, p=0.018), independent of physical fitness.
Inclusion of BMI in early adulthood as a potential confounder in all models did not change the association between physical performance and the presence of plaques, compared with the main analysis of complete cases. In contrast, adjustment for weight in early adulthood alone (OR 0.84, p=0.058, model 2) or together with height in early adulthood (OR 0.85, p=0.072, model 2) attenuated the estimates. The association between muscle strength and the presence of plaques remained nonsignificant regardless of adjustment for BMI or weight in early adulthood alone or together with height. After adjusting for BMI in early adulthood, the nonlinear relationship between physical performance and cIMT was attenuated (nonlinear p=0.051 in model 2). After including weight in early adulthood alone or with height, the nonlinear association in model 2 predominated. The nonsignificant association with physical performance and cIMT ≥ the 75th percentile remained unchanged after including BMI in early adulthood, weight alone, or height. Adjustment for BMI in early adulthood, weight alone, or height did not change the nonsignificant association between muscle strength and cIMT.
Lower prevalence of plaques
Higher physical performance in early adulthood, but not higher muscle strength, might protect against the development of carotid plaque in adulthood. The underlying mechanism could be due to the combination of body mass index, systolic blood pressure, glucose tolerance status, non-HDL cholesterol, and triglycerides rather than a single CVD risk factor.
Literature:
- De Winter MA, et al: Recurrent venous thromboembolism and bleeding with extended anticoagulation: the VTE-PREDICT risk score. EurHeartJ 2023.
https://doi.org/10.1093/eurheartj/ehac776 - Åberg ND, Kuhn HG, Nyberg J, et al: Influence of cardiovascular fitness and muscle strength in early adulthood on long-term risk of stroke in Swedish men. Stroke 2015;46: 1769-1776.
- Högström G, Nordström A, Nordström P: High aerobic fitness in late adolescence is associated with a reduced risk of myocardial infarction later in life: a nationwide cohort study in men. Eur Heart J 2014;35:3133-3140.
- Timpka S, Petersson IF, Zhou C, Englund M: Muscle strength in adolescent men and risk of cardiovascular disease events and mortality in middle age: a prospective cohort study. BMC Med 2014;12: 1-8.
- He N, Zhang Y, Zhang L, et al: Relationship between sarcopenia and cardiovascular diseases in the elderly: an overview. Front Cardiovasc Med 2021;8: 1-12.
- Jae SY, Lee KH, Kim HJ, et al: Separate and joint associations of cardiorespiratory fitness and healthy vascular aging with subclinical atherosclerosis in men. Hypertension 2022;79: 1445-1454.
- Karabinus JA, Deblois JP, Keller A, et al: The inverse association of muscular strength with carotid intima-media and extra-media thickness in women. Int J Sports Med 2021;42: 419-424.
- 8 Albin EE, Brellenthin AG, Lang JA, et al: Cardiorespiratory fitness and muscular strength on arterial stiffness in older adults. Med Sci Sports Exerc 2020;52: 1737-1744.
- Aengevaeren VL, Mosterd A, Sharma S, et al: Exercise and coronary atherosclerosis: observations, explanations, relevance, and clinical management. Circulation 2020;141: 1338-1350.
- Näslund U, Ng N, Lundgren A, et al: Visualization of asymptomatic atherosclerotic disease for optimal cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomized controlled trial. Lancet 2019;393: 133-142.
CARDIOVASC 2023; 22(1): 30–31











