Metabolic dysfunction has far-reaching negative effects on the body, which can manifest as cardiovascular and liver disease. Traditionally, these conditions have been treated in an organ-centered manner, resulting in isolated care. However, due to the systemic impact of metabolic dysfunction, a multidisciplinary approach is necessary to achieve optimal patient outcomes. This article highlights how cardiac treatments can have beneficial effects on the liver and vice versa, and emphasizes the need to address the disease processes rather than the organ-specific consequences of metabolic dysfunction.
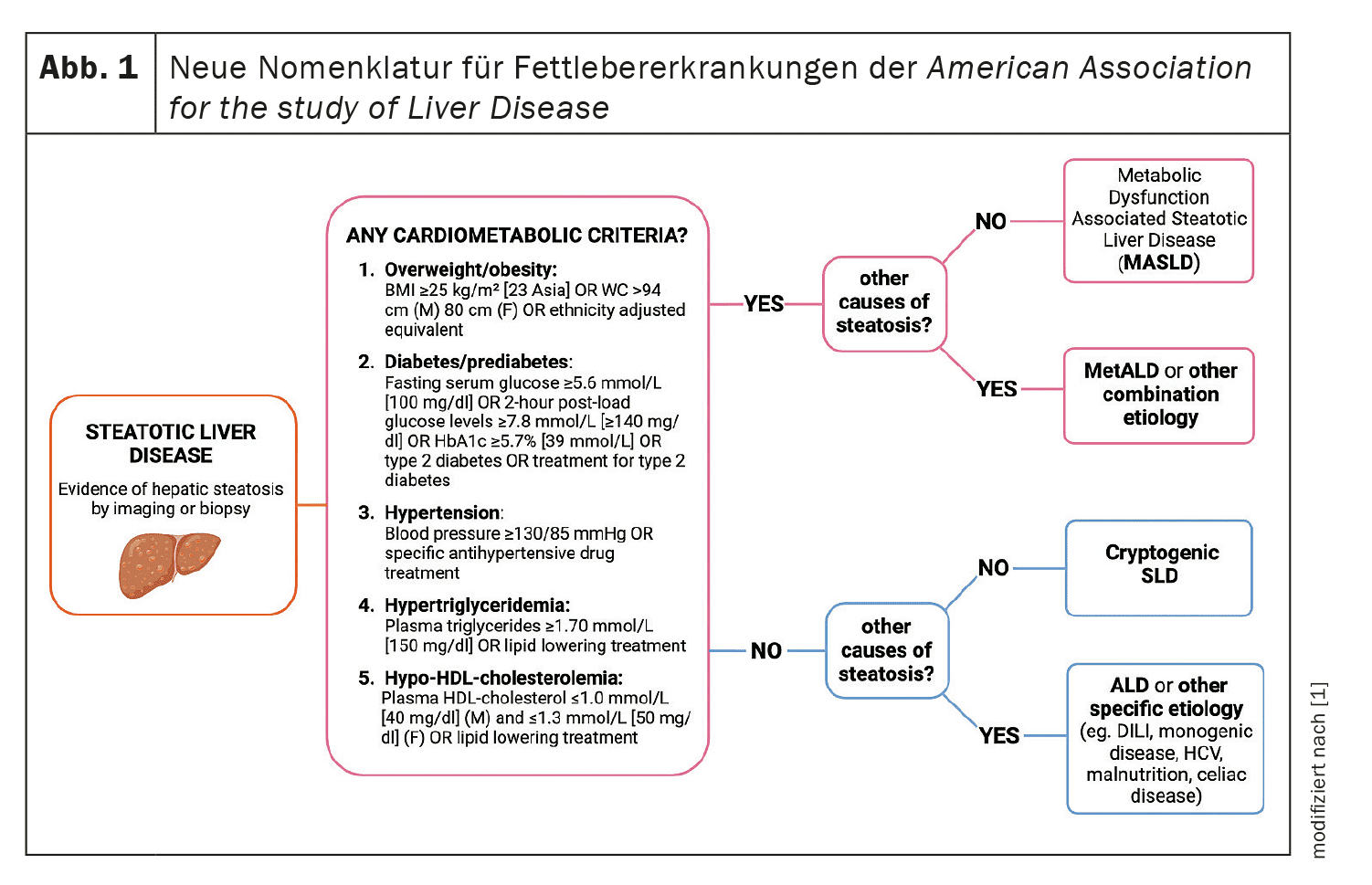
Cardiometabolic diseases provide an ideal basis for interdisciplinary collaboration between cardiology and hepatology. Advances in research have enabled a better understanding of the complex pathogenetic mechanisms underlying these diseases and their association with cardiovascular disease. The term “metabolic dysfunction-associated steatotic liver disease” (MASLD) was introduced to emphasize the dependence of hepatic steatosis on dysmetabolic conditions such as metabolic syndrome, diabetes mellitus and obesity.
New nomenclature and pathophysiology
The introduction of the new terminology MASLD and MetALD (metabolic and alcohol related/associated liver disease) emphasizes the need to treat the underlying metabolic disorders and not just the liver-related symptoms. This new classification avoids the stigmatization of terms such as “fatty liver” and has important implications for patient advocacy and public health. The pathophysiology of MASLD is closely linked to the interaction between lipid and glucose metabolism, which leads to a persistent systemic inflammatory state. This meta-inflammation plays a critical role in the development of both cardiovascular and hepatic disease. Effective treatment therefore requires approaches that go beyond the isolated consideration of individual organs.
Cardiological approaches to improving liver health
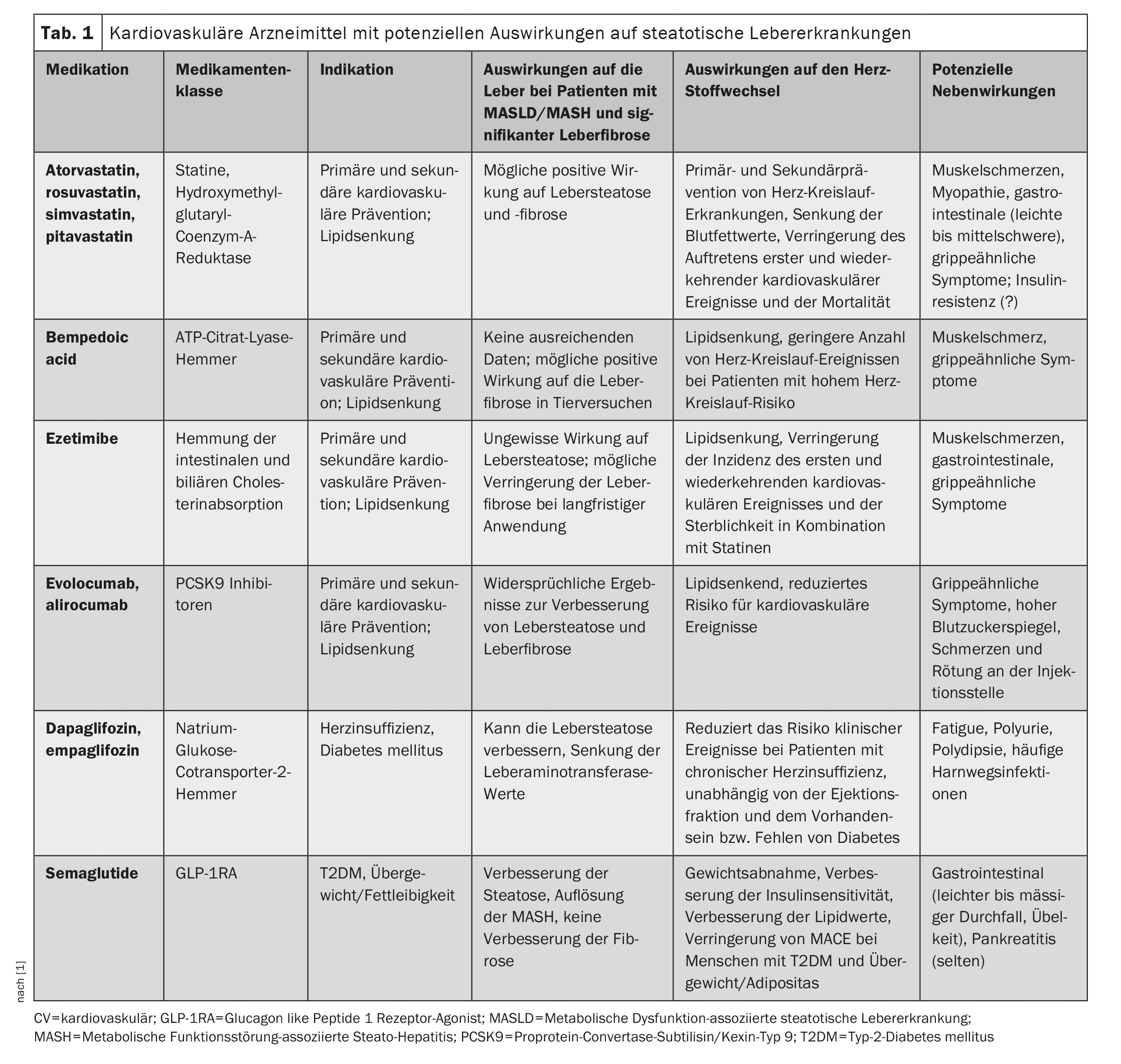
- Statins and bempedoic acid: Statins, such as atorvastatin and rosuvastatin, are key components of cardiovascular prevention. Studies show that statins may also have positive effects on hepatic steatosis and fibrosis. A randomized clinical trial of military personnel showed improvements in hepatic steatosis and fibrosis when treated with statins. Bempedoic acid, which works by inhibiting ATP citrate lyase, may also have beneficial effects on liver fibrosis, but further studies are needed.
- Ezetimibe: This drug reduces intestinal cholesterol absorption and has potentially positive effects on liver fibrosis with long-term use. Studies show that ezetimibe in combination with statins can reduce the risk of cardiovascular events in patients with high NAFLD fibrosis.
- PCSK9 inhibitors: These drugs, such as evolocumab and alirocumab, show conflicting results regarding their effect on hepatic steatosis and fibrosis, but may be beneficial due to their lipid-lowering properties. Studies indicate possible positive effects on liver health, but need further confirmation.
- SGLT2 inhibitors and GLP-1 receptor agonists: These drugs not only improve glycemic control and promote weight loss, but also have positive effects on liver health. SGLT2 inhibitors such as dapagliflozin and empagliflozin and GLP-1 receptor agonists such as semaglutide have shown significant improvements in hepatic steatosis and cardiovascular risk factors in clinical trials (Table 1).
Hepatological approaches to improving cardiovascular health
Lifestyle interventions: Improved metabolic health through lifestyle changes, including diet and physical activity, can prevent both liver and heart disease. These interventions are effective but often not sufficient to stop the rising morbidity and mortality from MASLD.
Pharmacologic approaches: Vitamin E and pioglitazone have been shown to be beneficial in the treatment of MASH, but with limited cardiovascular benefits. New drugs such as Lanifibranor and Resmetirom show promising results in simultaneously improving liver and heart health.
Specific medications and their effects
- Vitamin E: Vitamin E, a fat-soluble antioxidant, shows positive effects in the treatment of MASH, but without significant improvement in liver fibrosis. The cardiovascular effects of vitamin E are mixed, with some studies showing protective effects and others showing no significant benefits.
- Pioglitazone: A thiazolidinedione that activates PPARγ, improves insulin resistance, inflammation and lipid metabolism. Studies show positive effects on liver histology in MASH patients, but with side effects such as weight gain and heart failure.
- Lanifibranor: A pan-PPAR agonist that has shown promising results in clinical trials by simultaneously improving adipogenesis, inflammation and fibrosis. Lanifibranor has also shown positive effects on lipid profile and insulin sensitivity.
- Resmetirome: A selective THR-β agonist that has shown a reduction in liver fat and an improvement in MASH parameters in clinical studies. Resmetirome also shows positive effects on atherogenic lipid particles and could therefore offer cardiovascular benefits.
1. statins and bempedoic acid
Statins are a cornerstone of cardiovascular prevention and treatment. Studies have shown that they can also have positive effects on liver health. In a clinical trial with military personnel, statins showed improvements in liver steatosis and fibrosis. Animal studies also support these positive effects. However, further studies are needed to clarify the exact mechanisms and long-term effects.
Bempedoic acid, an ATP citrate lyase inhibitor, also shows promising results in animal models. It could reduce liver fibrosis and improve metabolic health. Initial clinical studies indicate a positive effect on cardiovascular health, but here too further studies are needed to confirm the long-term effects and safety.
2. ezetimibe
Ezetimibe reduces intestinal cholesterol absorption and, in combination with statins, has been shown to reduce the risk of cardiovascular events in patients with high NAFLD fibrosis. However, the effect of ezetimibe on liver fibrosis and steatosis needs further investigation before clear recommendations can be made.
3. PCSK9 inhibitors
PCSK9 inhibitors such as evolocumab and alirocumab are new and promising drugs for lowering LDL cholesterol. However, their effect on liver health is not yet fully understood. Some studies show positive effects on hepatic steatosis and fibrosis, while others report no significant improvements. Further research is needed to understand the role of these drugs in the treatment of MASLD.
4. SGLT2 inhibitors and GLP-1 receptor agonists
SGLT2 inhibitors and GLP-1 receptor agonists have been shown to be effective in both improving glycemic control and weight loss. These drugs also show positive effects on liver health, including reducing hepatic steatosis and improving liver function. This dual effect makes them promising candidates for the treatment of MASLD and cardiovascular disease.
5. other medications
Other drugs under investigation include:
- Metformin: Improves insulin sensitivity and has shown positive effects on liver health, although it is not specifically recommended for the treatment of MASH.
- Omega-3 fatty acids: Have shown positive effects in experimental studies, but clinical studies have not yet shown clear benefits for liver health.
- Fibrates: Reduce triglycerides and may have positive effects on liver health, but further studies are needed.
Collaboration and future research
Close collaboration between cardiologists and hepatologists is essential to achieve the best treatment outcomes for patients with MASLD. Future research should focus on the development of new therapies that address inflammatory pathways and multiple comorbidities. This could significantly improve the overall health and quality of life of patients. The implementation of lifestyle changes and multidisciplinary approaches in clinical practice will also be crucial to drive progress in the treatment of MASLD.
Source:
- Raggi P, Milic J, Manicardi M, et al: Metabolic dysfunction-associated steatotic liver disease: An opportunity for collaboration between cardiology and hepatology; Open AccessPublished: March 15, 2024. doi: https://doi.org/10.1016/j.atherosclerosis.2024.117523.
CARDIOVASC 2024; 23(2): 34–36