Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated immune response to infection. Early detection is of key prognostic importance in childhood. It is crucial to recognize nonspecific but highly sensitive clinical warning signs in order to start supportive and antibiotic therapy as soon as possible, but follow-up after successful therapy is also of central importance.
The term sepsis describes a syndrome, i.e., co-occurring nonspecific symptoms that signal infectious-inflammatory dysfunction of multiple organ systems. Because the distinction from harmless systemic inflammatory reactions (SIRS) to, for example, intercurrent viral infections was imprecise under the previous sepsis definitions of 1991 and 2001 [1], and to reflect pathogenesis and threat, the most recent, third, international consensus conference, Sepsis-3, redefined sepsis as life-threatening organ dysfunction caused by a dysregulated immune response to infection.
The difficulty in everyday life, of course, is to recognize sepsis in its early stages. This is important because early detection and immediate therapy have a decisive impact on the prognosis. It is well known that every hour of delay until successful shock reversion doubles the mortality of sepsis. Consistent with this, a recent published work in 130 children with severe sepsis or septic shock showed a 3- to 4-fold increase in mortality when the latency from the onset of sepsis symptoms to the first antibiotic dose is more than 3 hours [2]. The background is that fulminant septicemias proceed exponentially, so that each preceding step of the ominous cascade potentiates subsequent events. Even today, most children who succumb to severe sepsis die within the first 24-48 hours after hospitalization.
The early detection of sepsis
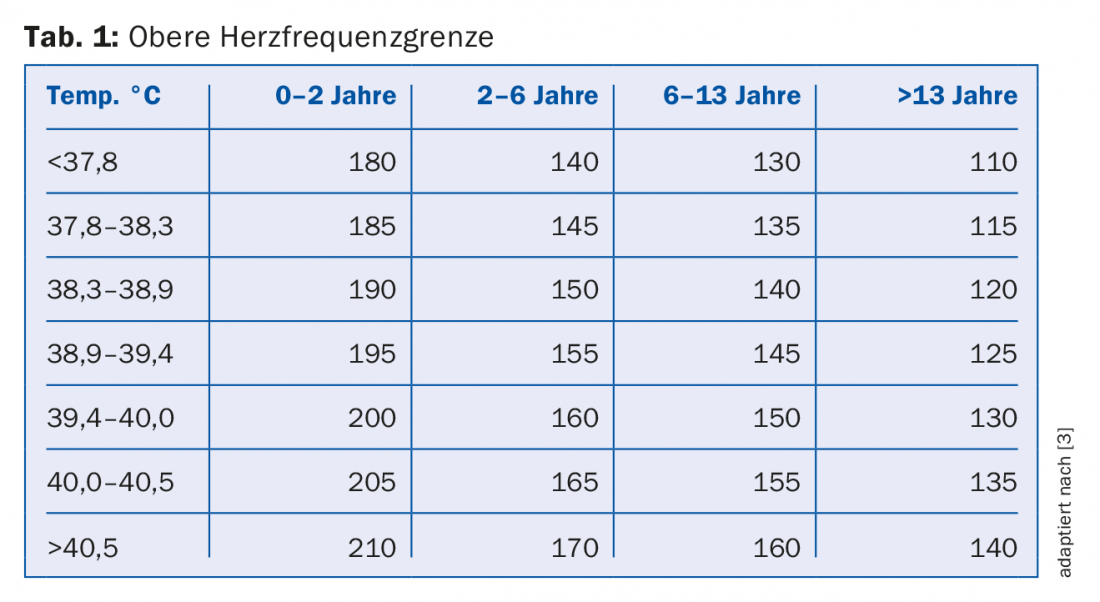
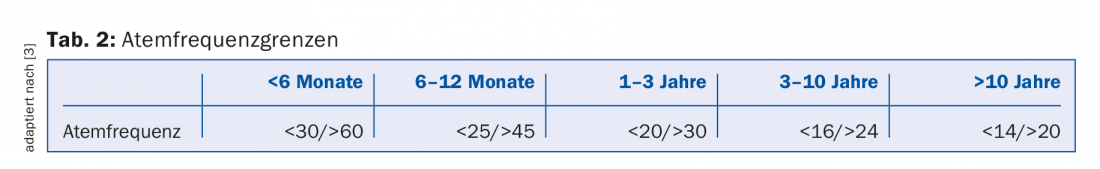
Late recognition of sepsis is common not only in practices and emergency departments, but also in hospitalized patients. Several recent studies have therefore focused on improving the early detection of sepsis. In this regard, positive experience has been reported with an early sepsis detection algorithm for hospitalized children based on temperature abnormality, defined as a body temperature of <36.0°C or >38.5°C, plus tachycardia and/or brady- or tachypnea as warning signals [3]. These warning signs proved to be very sensitive, although, as expected, not very specific. The age- and temperature-adapted limit values for heart rate and respiratory rate used for this purpose are shown in tables 1 and 2. The table shows that for every 0.5-0.6°C increase in temperature, the heart rate limit increases by 5/min each time. Limits apply provided additional factors such as pain, anemia, dehydration, etc. are excluded.
Another paper evaluated a systematic sepsis screening algorithm using nearly 20,000 children with temperature abnormality (<36.0°C or >38.5°C) versus conventional clinical assessment in a population typical of our everyday life with very low sepsis prevalence of only one case per 200 children [4]. This algorithm considered various vital signs along with recapillarization time, vigilance, and any baseline morbus and proved to be very sensitive with a negative predictive value of over 99.5%; however, only 2.5% of the positive children actually had sepsis. In contrast, clinical assessment was less sensitive but much more specific. Early detection algorithms thus have primarily a “red flag” function.
The message is that a good early detection rate necessarily also leads to the fact that the suspicion is not confirmed in the end in many children, which then must not be interpreted as an expression of a lack of clinical intuition.
Diagnosis of sepsis
Although the International Sepsis Definition Conference in 2001 was still speculating that the systemic inflammatory response would in the future be identified only biochemically and immunologically rather than clinically, biomarkers are not crucial for the diagnosis of sepsis even today because they cannot exclude early-stage sepsis nor would they be specific for it [5]. The diagnosis is primarily a clinical one; laboratory tests are part of the diagnostic workup. Blood gas analysis (acidosis) and lactate determination reflect the extent of cardiopulmonary limitation. Initial lactate elevation, which is commonly considered to reflect inadequate microcirculation in sepsis, also appears to be a marker of a more serious prognosis in children, although the data are less robust than in adults. Thus, mortality increased threefold in 1300 children with sepsis with an initial lactate of >4 mmol/L. However, lactate elevations in sepsis may also be contributory to increased adrenergic glycolysis or decreased hepatic clearance. Microbiological examinations, imaging techniques, and organ and inflammatory values are also part of the diagnostic workup, with the latter being useful as progression parameters. However, C-reactive protein and procalcitonin are not suitable to invalidate a suspicion of sepsis [6].
Initial care of the septic child
The mainstays of sepsis treatment in the emergency setting remain oxygen, crystalloid fluid substitution, empiric antibiotics, and respiratory support when appropriate. Liquid should be given generously, but according to effect. This remains true after the publication of the FEAST trial, which led to some uncertainty because in this study, initial bolus administrations were associated with higher mortality in over 3000 African children who presented to the emergency department with fever and compromised peripheral perfusion [7]. As early as the 1990s, however, a direct correlation between the amount of infused fluid and better survival was demonstrated, and more recent studies also suggest that circulatory insufficiency is prognostically decisive and that inadequate fluid supplementation is one of the preventable causes of lethal severe bacterial infections [8].
Continuous monitoring is a given, as respiratory and circulatory stability can change rapidly. Pulse oximetry and respiratory pattern, heart rate and peripheral blood flow, and vigilance and reactivity are the most important parameters.
What to do in practice (if available and feasible)?
- Monitoring and, if necessary, Basic Life Support (BLS)
- Oxygen, 1-2 (-4) L/min by nasal cannula
- Liquid, NaCl 0.9% or Ringer’s lactate, 20 ml/kg as bolus, repeat if necessary.
- Blood cultures, provided this does not result in a substantial delay in the first antibiotic administration [9].
- Broad-spectrum antibiotic
Current recommendations aim to administer the first fluid bolus within 30-60 min [5] and the first antibiotic administration within 60 min [9] after recognition of sepsis. Thus, the extent to which primary care should be provided in the practice depends not only on the child’s condition and local availability, but also on the expected delay before the emergency team arrives or at the hospital. The time windows mentioned can serve as decision-making aids.
Aftercare
Although an estimated one-third of all deaths in large pediatric intensive care units involve children with sepsis, over 70-80% of non-oncology children with severe sepsis or septic shock survive and return to the care of primary care physicians.
Repeated severe episodes of sepsis during the course are extremely rare in immunocompetent children, but the children remain at risk during the first months after hospital discharge. Nearly half of all patients require rehospitalization in the first few months after severe sepsis, an average of three times and mostly emergency [10]. This particularly affects children with comorbidities and very young children.
Approximately 1/3 of all survivors in the SPROUT study of 500 children with severe sepsis still showed a more or less pronounced loss of neuromotor skills at hospital discharge or after 90 days, as assessed by the Pediatric Overall Performance Category (POPC) score [11]. By analogy, a neuropsychological follow-up study examining children 3-6 months after severe illness with hospitalization in the intensive care unit found that teachers noted the following academic difficulties in these children compared with healthy controls [12]:
- A drop in academic performance in 29% vs. 4%, p=0.007.
- increased difficulty completing schoolwork in 33% vs. 8%, p=0.01
- A reduced capacity for divided attention in 44% vs. 11%, p=0.004
- a decrease in the ability to consider different options in 44% vs. 8%, p=0.001
Children who had meningoencephalitis fared the worst, followed by those with sepsis. Deficits in memory and attention were the main findings. Various factors are discussed as causes. On the one hand, 30% of children can be assumed to have post-traumatic stress disorder (PTSD), which can lead mainly to disorders in the area of attention and other executive functions. On the other hand, neuronal cell damage due to microabscession, systemic inflammation, and microcirculatory disturbances probably also play a role and may involve other cognitive domains in addition to the above-mentioned dysfunctions. The deficits are most pronounced in children who suffered seizures in sepsis, which on the one hand are a symptom of neuronal cell irritation, but on the other hand can be cell damaging if prolonged. Little is known about the long-term prognosis. Younger children seem to be more affected by permanent damage than older children due to increased vulnerability, contrary to the assumption of better cerebral plasticity.
Acute renal failure in the setting of sepsis is common and increases mortality and risk of cerebral sequelae, but little is known about the long-term prognosis of renal function. Many children are lost to follow-up. The literature suggests that at least 10% of children show longer-term pathologic renal function in terms of microalbuminuria, proteinuria, or arterial hypertension, and that up to half of those affected have a mildly impaired glomerular function rate (GFR) with unclear clinical value in terms of long-term prognosis. Regular analysis of urine sediment and blood pressure measurements at increasing intervals are therefore advisable in the longer term [13].
Cardiovascular function generally appears to recover well, and long-term pulmonary morbidity depends on the extent of pulmonary involvement or the presence of acute respiratory distress syndrome (ARDS).
Summary
Early detection of sepsis is essential in childhood. In the absence of specific markers, this is based on very nonspecific but highly sensitive warning signs such as temperature abnormality, tachycardia, deepened breathing, apathy, and vigilance reduction. Oxygen, BLS if necessary, an initial fluid bolus, and broad-spectrum antibiotics are the initial therapeutic steps. Follow-up is of great importance, especially with regard to neuropsychological deficits and possibly renal dysfunction.
Take-Home Messages
- Sepsis is redefined as life-threatening organ dysfunction caused by a dysregulated immune response to infection.
- Because fulminant courses are common, early detection is critical for prognosis. This is based on the nonspecific signs of temperature abnormality, tachycardia, brady- or tachypnea plus a clinical suspicion. Apathy and vigilance reduction are other important warning signs.
- Oxygen, crystalloid fluid substitution, empiric antibiotics, and respiratory support, if needed, are the cornerstones of primary care.
- In the first months after hospital discharge, children should be monitored closely. In the longer term, neuropsychological deficits and possibly nephrological sequelae are to be expected and justify appropriate follow-up.
Literature:
- Horeczko T, Green JP: Emergency department presentation of the pediatric systemic inflammatory response syndrome. Pediatr Emerg Care 2013; 29: 1153-1158.
- Weiss SL, et al: Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med 2014; 42: 2409-2417.
- Bradshaw C, et al: Implementation of an Inpatient Pediatric Sepsis Identification Pathway. Pediatrics 2016; 137: e20144082.
- Balamuth F, et al: Comparison of Two Sepsis Recognition Methods in a Pediatric Emergency Department. Acad Emerg Med 2015; 22: 1298-1306.
- Davis AL, et al: American College of Critical Care Medicine Clinical Practice Parameters for Hemodynamic Support of Pediatric and Neonatal Septic Shock. Crit Care Med 2017; 45: 1061-1093.
- Niehues T: C-reactive protein and other immunological biomarkers. Sense and nonsense in infection diagnostics. Monatsschr Kinderheilkd 2017; 165: 560-571.
- Maitland K, et al: Mortality after fluid bolus in African children with severe infection. N Engl J Med 2011; 364: 2483-2495.
- Launay E, et al: Suboptimal care in the initial management of children who died from severe bacterial infection: a population-based confidential inquiry. Pediatr Crit Care Med 2010; 11: 469-474.
- Rhodes A, et al: Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med 2017; 43: 304-377.
- Czaja AS, Zimmerman JJ, Nathens AB: Readmission and late mortality after pediatric severe sepsis. Pediatrics 2009; 123: 849-857.
- Fitzgerald JC, et al: Acute Kidney Injury in Pediatric Severe Sepsis: An Independent Risk Factor for Death and New Disability. Crit Care Med 2016; 44: 2241-2250.
- Als LC, et al: Neuropsychologic function three to six months following admission to the PICU with meningoencephalitis, sepsis, and other disorders: a prospective study of school-aged children. Crit Care Med 2013; 41: 1094-1103.
- Askenazi DJ: Do children with acute kidney injury require long-term evaluation for CKD? Am J Kidney Dis 2012; 59: 478-480.
HAUSARZT PRAXIS 2017; 12(11): 26-30











