Visceral hyperalgesia plays an important role in the pathomechanism of functional gastrointestinal complaints. Symptom-oriented analgesic treatment can modulate the pain threshold. The analgesic effects of menthacarin have been demonstrated in several studies. Recent findings on visceral hypersensitivity shed light on the underlying mechanisms of action of the peppermint and caraway oil combination.
The pathogenesis of functional gastrointestinal disorders is not yet fully understood. According to current understanding, a multifactorial interaction structure is assumed, with psychosomatic factors playing a role in addition to somatic factors. That visceral hypersensitivity in the sense of increased pain perception is an important aspect has been empirically demonstrated several times [1–3] (box). It is therefore an important therapeutic starting point.
|
Perceptual and pain threshold to intestinal stimuli. The mechanism of visceral hypersensitivity refers to an increased vigilance to specific sensations in the gastrointestinal tract and has been described as an important pathogenetic factor for functional digestive complaints [13]. Deeper perceptual and pain thresholds to intestinal stimuli may result in central nervous sensitization. Visceral hypersensitivity plays an important role in both irritable bowel syndrome and functional dyspepsia [14]. Epigastric pain is a characteristic feature of functional dyspepsia, and in irritable bowel syndrome, a low pain threshold is involved in addition to altered gastrointestinal microflora when the intestinal wall expands. According to the ROM-IV consensus, symptom-oriented, individualized, and time-limited therapy should be implemented once the diagnosis of functional gastrointestinal symptoms has been established [4]. The primary therapeutic goal is to reduce symptoms and improve quality of life [15]. By modulating visceral hyperalgesia and the intestinal microbiota, as is possible through treatment with Carmenthin® , epigastric pain can be relieved and the microflora can be brought into better balance. |
Carmenthin® – symptom relief through synergistic mechanism of action
Currently, there is no causal treatment strategy for functional gastrointestinal symptoms, but the focus is on alleviating symptoms such as bloating, epigastric pain, cramping, bloating, diarrhea, or constipation. According to the ROM-IV consensus, symptom-oriented, individualized, and time-limited therapy should be performed for functional gastrointestinal complaints after organ pathological causes have been ruled out [4]. On the back of ample evidence from placebo-controlled trials, phytotherapeutics are now recommended by national and international guidelines as a symptomatic therapeutic option for functional gastrointestinal disorders [4,5].
Proven reduction of visceral hypersensitivity by combination (Carmenthin®).
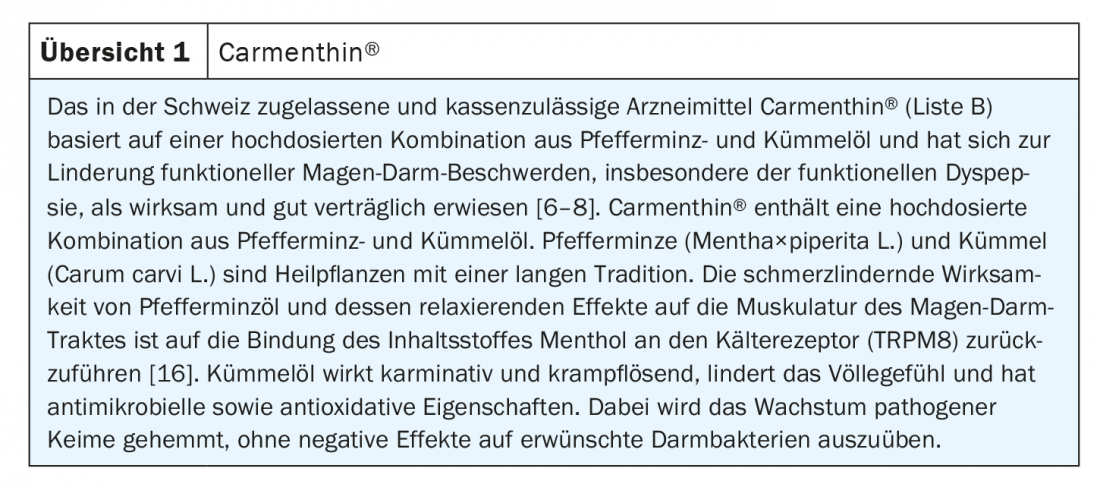
The preparation Carmenthin® (active ingredient: Menthacarin®) is based on a high-dose combination of peppermint and caraway oil and is approved for adults and adolescents aged 12 and over in Switzerland for the treatment of mild cramps, bloating, epigastric pain and flatulence [6,7].
Thanks to the synergistic effect of the high-dose combination of the two essential oils, Carmenthin® (review 1) reduces post-inflammatory visceral hyperalgesia by up to 50% in a placebo comparison [8]. Through antifungal and antibacterial properties, the phytopharmacological preparation counteracts a deep pain threshold often associated with visceral hyperalgesia. The symptom-relieving effects have been empirically proven several times. In patients with chronic or recurrent functional dyspepsia, evidence of efficacy includes that from a double-blind placebo-controlled randomized multicenter trial (n=114) [9]. At 2 and 4 weeks after baseline, the treatment arm with Carmenthin® (2×/d 1 capsule) showed a significantly greater reduction in symptoms compared to placebo (p<0.001). Pain relief proved to be a major effective factor.
Recent study data also indicate the pain-reducing effects of this phytopharmacological combination. Among other things, the underlying mechanism could be analyzed in more detail in the animal model. In a vivo study in rats, visceral sensitivity was operationalized by visceromotor responses when the intestinal wall was stretched [12]. The measured values were recorded before and 24 h respectively 7 days after a stress test in the conditions Carmenthin® vs. placebo. Changes in the microbiome and mycobiome were measured by various in vivo and in vitro parameters. The analyses revealed that the reversibility of hypersensitivity observed in the Carmenthin® condition was accompanied by a modification of the microbiome and mycobiome [12]. Since pain on stretching of the intestinal wall is a characteristic symptom in irritable bowel syndrome, these results suggest that Carmenthin® has beneficial effects for this indication.
Gut-brain axis (“Brain-Gut-Axis”)
There is quite a bit of human experimental efficacy evidence in the literature for peppermint oil in relieving symptoms of IBS, as shown in a meta-analysis with data from several randomized placebo-controlled trials [10].
The gastrointestinal tract is a highly innervated system, with a multitude of afferent nerve fibers generating information regarding intestinal contents, regulatory processes of digestion, and immune defense [17]. There is evidence that in functional gastrointestinal disorders, both the central processing of this information and the response to intestinal signals are impaired [18,19]. These mechanisms play out within the gut-brain axis (“brain-gut axis”), which is a concept for the interaction of the peripheral and central nervous systems [19]. It is a biopsychosocial explanatory model for describing the complex bidirectional interactions that occur within disorders of gastrointestinal function [20].
Visceral signals are switched via nerve fibers of the autonomic nervous system in the spinal cord. Reflex systems are activated there that regulate the functions of visceral organs in cooperation with the enteric nervous system. Although most of the signals are not transmitted to the cerebrum and thus escape conscious perception, some of these stimuli from the body periphery are registered in the brainstem. In this area and in the cerebrum, there are close connections back to the enteric nervous system via various pathways of the autonomic nervous system, the endocrine system as well as the immune system. It is therefore a complex psychobiological structure.
Literature:
- Agrawal A: Am J Gastroenterol 2009; 104: 1998.
- Dothel G, et al: Gastroenterology 2015; 148: 1002-1011.e4.
- Dorn SD: Gut 2007; 56: 1202
- Stanghellini V, et al: Rome IV – Gastroduodenal Disorders. Gastroenterology 2016 pii: S0016-5085(16)00177-3.
- Talley NJ, Walker MM, Holtmann G: Functional dyspepsia. Curr Opin Gastroenterol 2016; 32: 467-473.
- Specialized information: www.compendium.ch
- Madisch A, et al: Internist 2015; 56, (Suppl. 1): 28.
- Adam B, et al: Scandinavian Journal of Gastroenterology 2006; 41: 155-160.
- Rich G, et al: Neurogastroenterol Motil 2017; 29(11).
- Khanna R, MacDonald JK, Levesque BG: J Clin Gastroenterol 2014; 48: 505-512.
- Layer P, et al: AWMF registry number: 021/016. Z Gastroenterol 2011; 49: 237-293.
- Botschuijver S, et al: Neurogastroenterol Motil 2018; 30(6): e13299.
- Madisch A, et al: Dtsch Arztebl Int 2018; 115: 222-232.
- Madisch A, et al: Wiener Medizinische Wochenschrift 2019; 169: 149-155.
- Cremonini F: Neurogastroenterol Motil 2014; 26: 893-900.
- Deutsche Apothekerzeitung (DAZ): DAZ 2018 (9): 73, 01.03.2018.
- Brookes SJH, et al: Nat Rev Gastroenterol Hepatol 2013; 10(5): 286-296.
- Matricon J, et al: Aliment Pharmacol Ther 2012; 36(11-12): 1009-1031.
- Lee YJ, Park KS: World J Gastroenterol 2014; 20(10): 2456-2469.
- Elsenbruch S, Icenhour A, Enck P: Visceral pain – a biopsychological perspective. Neuroforum | Vol. 23: Issue 3. DOI: https://doi.org/10.1515/nf-2017-0029
HAUSARZT PRAXIS 2021; 16(1): 26-27