While a great many 60- to 80-year-olds have prostatic hyperplasia, only about 40% of them show symptoms that include obstructive and irritative micturition symptoms. The following article discusses which examinations are possible and useful in the general practitioner’s office and when a urologist should be consulted. Furthermore, he discusses the advantages and disadvantages of drug, interventional, and surgical therapeutic procedures. Here, especially holmium laser enucleation of the prostate shows good results for large organs.
Prostatic hyperplasia is an old problem. In ancient Greece, Hippocrates of Kos already distinguished between dysuria, stranguria and ischuria. First catheters, then made of bronze, are 1000 BC. been described in Egypt.
The Hippocratic oath not to perform surgical procedures, as well as the lack of access to anatomical studies through cadaver dissections, condition an anatomical first description of the prostate by Herophilos of Chalcedon only around 300 BC.
Urinalysis according to Galenos of Pergamon (c. 131 to 201 A.D.) by density, color, odor, taste and sediment in combination with symptoms and sex of the patient is known until the 17th century. Standard.
It was not until the founder of pathology Giovanni Morgagni (1683-1771) described anatomy and pathology of the urogenital tract and in this context prostatic hyperplasia in his five-volume work “Vom Sitz und den Ursachen der Krankenheiten” (De sedibus et causis morborum).
Demographic trends as well as an improved body awareness with a low willingness to suffer make prostatic hyperplasia a problem that affects 80% of 60 to 80 year old men. However, only about 40% of these patients are symptomatic.
Etiology and pathophysiology
Prostate carcinomas arise 70% in the prostate capsule, 10% in the central zone, and 20% in the transition zone between the two. Benign prostatic hyperplasia (BPH) also develops in this transition zone as well as in the periurethral glands. Macroscopically, a distinction is occasionally made between a bilobular (lateral lobes only) and trilobular (lateral lobes and middle lobes) configuration.
Histologically, glandular (adenoma) and fibromuscular (stroma) hyperplasia are distinguished. The term hyperplasia is only partially correct, as it is a true numerical proliferation of cells. The definitive genesis of BPH is not known to date. Hormonal changes in the estrogen/testosterone ratio with age are discussed.
There are ethnic and geographic differences in treatment frequency: for example, compared with white and black Americans, Asians have a significantly lower risk of needing surgery for BPH. Hyperalimentation (meat and fat consumption and physical inactivity), constipation as well as differences in sexual activity are discussed. Male siblings of patients with clinical BPH have a sixfold higher risk of also developing BPH.
Symptomatology
The clinical symptoms of BPH do not correlate with the pathoanatomical conditions. In general, a distinction must be made between obstructive and irritative bladder voiding disorders.
Obstructive micturition disorders include:
- weakened urine stream
- prolonged micturition time
- Drizzle
- Residual urinary sensation.
- Irritative micturition disorders include:
- Pollakiuria
- Nocturia
- Dsyurie
- Urge (urge incontinence symptomatology).
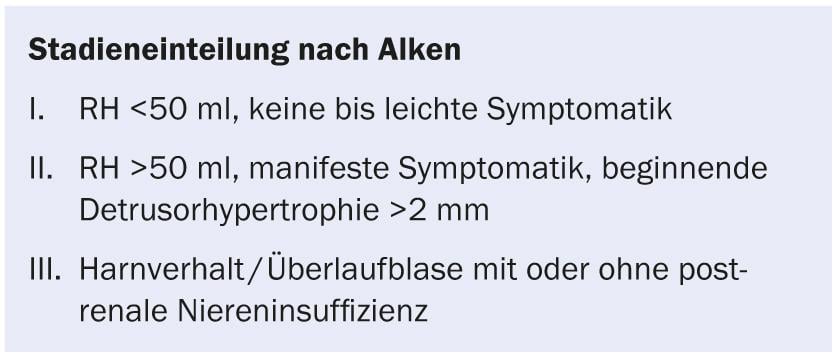
Bladder end-trusor hypertrophy due to high micturition pressures can lead to pollakiuria, as can increasing residual urine formation with a corresponding decrease in the effectively usable bladder volume. If the bladder muscles become exhausted, overflow incontinence (ischuria paradoxa) or urinary retention may develop. Sonographic investigations are indicated accordingly. The staging according to Alken is shown in the box.
Recurrent urinary tract infections, epididymitis, or hematuria should be referred for urologic evaluation because these may be symptoms of increased intravesical micturition pressure with consecutive residual urine formation, prostatic variceal bleeding, and ascending inflammation.
Similarly, it makes sense to refer patients for examination in good time if there is any suspicion, since irritative complaints in particular can persist stubbornly for a long time if diagnosis and therapy are delayed, even after surgery.
Examinations by the family doctor
Accurate micturition history: Should take place considering possible effects of diuretic administration or heart failure (cardiac-related nocturia) on micturition behavior. A drinking-micturition log can be kept over several days for accurate differentiation.
Digital rectal examination (DRU): This is the simplest diagnostic measure with good information about the size and condition (hardness, nodules, delimitability, symmetry) of the prostate. However, the DRU also provides good information on possible hemorrhoids or rectal tumors and gives an orienting assessment of a neurogenic bladder disorder, for example, via anal sphincter tone and the bulbocavernous reflex as well as perianal sensitivity.
Laboratory: urine stix and serum creatinine to exclude infection and postrenal insufficiency.
PSA: PSA is an integral part of routine diagnostics for BPH patients. As a protein, it is expressed by benign and malignant epithelial cells in the prostate and is thus not a tumor marker but a tissue marker. The weaknesses of PSA determination are well known, yet it is essential as an indicator of a necessary prostate biopsy to exclude a malignant genesis of the micturition symptoms. Therefore, patients with a PSA of 3.0 ng/ml and a PSA free/total ratio ≤12% should be referred for transrectal ultrasound to determine the size of the prostate and to correlate the PSA value with this. This is done with the help of a prostate risk calculation.
The Prostate Center Aarau, in cooperation with Mount Sinai Hospital Toronto, is conducting intensive investigations for new cancer-specific tumor markers.
Supplementary examinations by the urologist
Sonography: residual urine must not exceed 10-20% of the micturition volume. Sonography of the kidneys to exclude a dilated hollow system.
TRUS (transrectal ultrasound): In case of large prostate in DRU, because from an adenoma size of 60- 70 cc, the therapy of choice is no longer TUR-P, but holmium laser enucleation of the prostate (HoLEP).
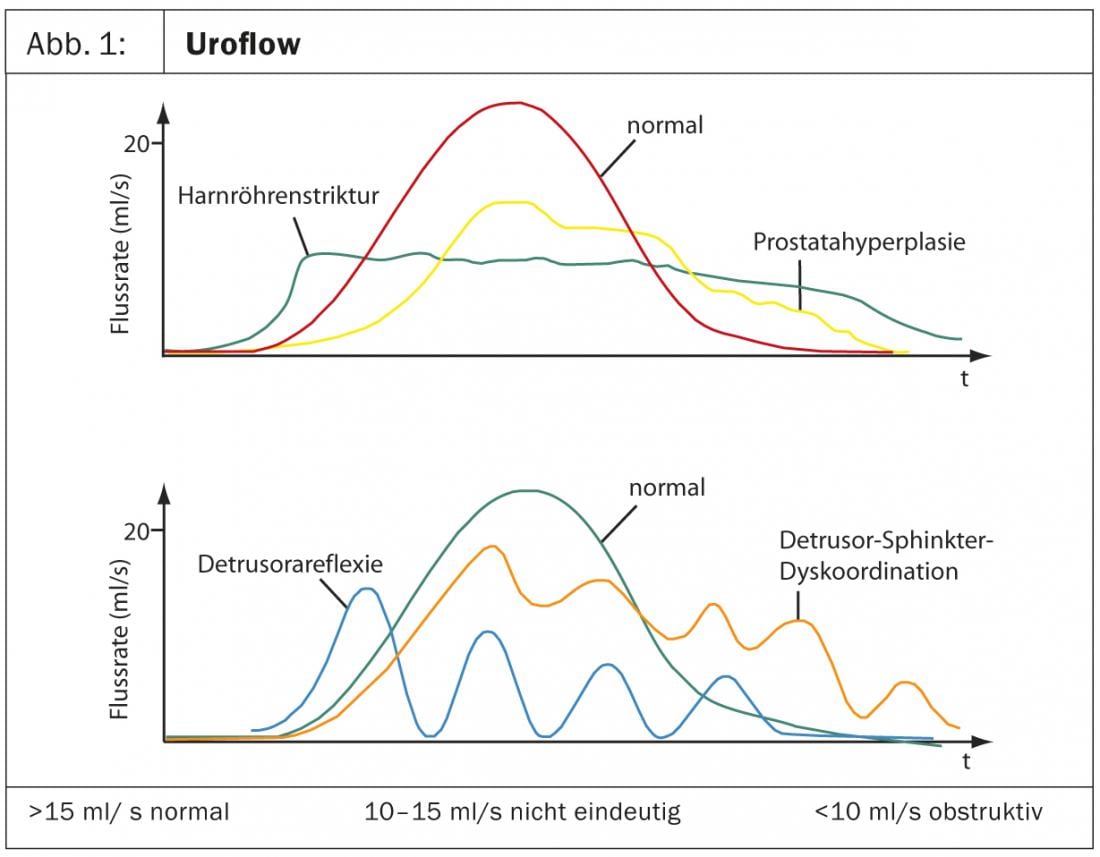
Uroflow: It is useful to ask patients to come to the urologist with a full bladder at the time of referral so that a uroflow can be obtained first. An important criterion is the maxflow, which should be above 15 ml/s. In addition to the suspicion of BPH, the graphical representation of the flow rate over time also permits differential diagnoses of bladder emptying disorders (Fig. 1) . If necessary, an abnormal uroflow should be followed by cystomanometry/videourodynamics in the presence of a neurogenic component/detrusor-sphincter dyssynergia.
Urethrocystoscopy: In addition to urethral strictures, bi- or trilobular prostatic hyperplasia, bladder neck sclerosis, bladder trabecularization, or diverticula may be diagnosed. Of great advantage is the technical possibility to show the patient directly the pathophysiological problem of his symptoms via a patient monitor and to illustrate the surgical and anatomical indication.
Drug therapy
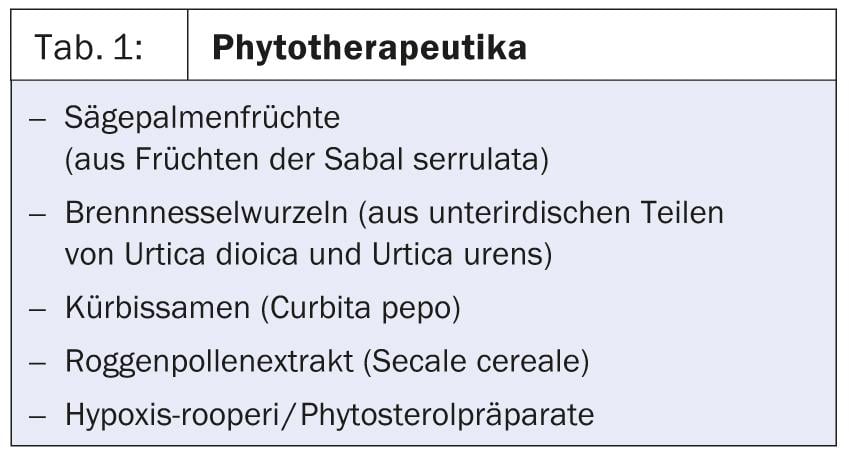
phytotherapeutics (Table 1): The ingredients of phytopharmaceuticals responsible for the therapeutic effects and their principles of action have not been clarified beyond doubt. The value of the plant extracts thus remains controversial. A substantial placebo effect is suspected, as micturition symptoms improved in some studies, but measurable parameters such as maximum flow and residual urine did not improve significantly. If symptoms are mild and there is no residual urine, it can’t hurt to try. Despite the lack of objective criteria, it is often true that he who heals is always right.
α-Receptor Blockers: α1-receptors and α1a-receptors are present in the bladder neck as well as the prostate, and their activation causes smooth muscle contraction. By blocking these receptors, the dynamic component of the obstruction can be relaxed. The medication is indicated at the onset of BPH and little pronounced, especially irritative symptoms. The duration of action varies, as do the side effects. The effectiveness of medication requires control of flow and residual urine. The agent tamsulosin has the highest α1a-receptor selectivity and thus the best clinical results, but a therapeutic trial with alfuzosin or terazusin is equally justified.
Side effects commonly reported include orthostasis, dizziness, and retrograde ejaculation, and occasionally loss of libido/potency.
Hormonal modulation: Testosterone is a prohormone in the prostate and is converted by 5α-reductase into the actual active form dihydrotestosterone, which binds to the androgen receptor. 5α-Reductase inhibitors inhibit the proliferative influence of DHT. For example, finasteride taken over a period of months resulted in a volume reduction of 20-30% (Höfner et al. 2000). Primarily, however, the obstructive BPH symptoms are also relieved, on the maximum urinary flow showed only an improvement of 1.4-1.9 ml/s compared to placebo. Combination preparations of tamsulosin and dutasteride in one capsule have been advertised more intensively in recent times, but the combination of active ingredients is nothing new in itself. More recent results (Combat study) justify a trial also with smaller prostate volumes (between 30-50 ml), but the effect is smaller here. 5α-Reductase inhibitors have erectile dysfunction as the most common side effect, also loss of libido in 5-15% and decreased ejaculation volume.
Full onset of action is expected after 6-12 months. Patients with advanced symptoms often cannot wait for such a time.
5α-Reductase inhibitors result in a PSA reduction of approximately 50%. A patient on 5α-reductase inhibitor therapy has a PSA threshold correspondingly not of 3 but of 1.5 ug/l, and thus needs earlier carcinoma screening.
Interventional procedures
Stent insert: insertion of platinum-coated metal alloys, titanium or polyethylene. Advantage is a possibility of use in multimorbidity. The disadvantage, apart from the need to change some preparations, is the frequency of infections and the feeling of constant need to urinate in a large proportion of patients.
Thermal procedures: With high-energy TUMT (transurethral microvellar-induced thermotherapy), symptoms are expected to reach the results of TUR-P within one year; this therapy is significantly inferior in urinary flow outcomes. TUNA (Transurethral Needle Ablation of the Prostate) involves the generation of interstitial heat (approximately 90°C) to produce thermonecrosis in the glandular body. This produces significant improvement in BPH symptoms, but has poor results in terms of urinary flow and requires repeated treatments in 42% of cases.
All of these are not standard procedures and are not recommended in national and international guidelines.
Operative procedures
TUR-P: The reference standard has long been transurethral resection of the prostate (TUR-P). Different manufacturers have good systems on the market. The modulations of the current in intensity or frequency as well as the distinction between monopolar (current return via adhesive electrode on the thigh) or bipolar system (current return in the transurethral device itself) do not make much difference in the functional end result. The advantage of bipolar resection is seen in the usability of physiological saline solutions as irrigation medium and results in less electrolyte shifts due to resorption of irrigation water. The average intraoperative blood loss is estimated to be approximately 500 ml, and transfusion rates are reported to be 0-20%, but de facto occur very rarely in our hospital. Marcoumar®, Xarelto® or Plavix® should be discontinued beforehand. be switched to low-molecular-weight heparin subcutaneously, ASA is not an obstacle.
KTP laser vaporization: The so-called KTP laser vaporization (greenlight laser) vaporizes excess prostate tissue with laser light in the visible range of 532 nm (green). The advantage is the almost bleeding-free operation even under anticoagulation, since blood vessels can be directly coagulated. With powerful 120 W laser, the effectiveness is comparable to TUR-P with >0.5 g/min. The disadvantage is that no histology is available due to vaporization and, accordingly, incidences of carcinoma are not detected. The reoperation rate due to obstructing detrital masses is 17%. In addition, delayed macrohematuria often occurs during the course of sloughing.
Holmium laser enucleation of the prostate (HoLEP): TUR-P should no longer be performed for large adenomas because of the volume load on the circulation due to irrigation fluid resorption. In many places, a transabdominal, transvesical adenoma enucleation (analogous to Freyer) or a transabdominal, extravesical adenoma enucleation (analogous to Milin) is the usual procedure for adenomas with a size of 100 g or more. A new laser procedure in the form of holmium laser enucleation of the prostate, or HoLEP, has been available for about eight years. It shows equally excellent results for all prostate sizes, but really plays out its advantages from an organ size >50-60 g. The obstructing lateral lobes ±middle lobes are completely removed transurethrally en bloc and pushed into the bladder. The resection base is directly coagulated with the holmium laser, so there is hardly any blood loss and also no significant resorption. The enucleated tissue blocks are then removed from the bladder by a morcellator and are available for the necessary histological examination.
With complete removal of the adenoma, the long-term functional outcomes are the same as with open surgery and, with a reoperation rate of <1% within seven years, are significantly better than with conventional TUR-P (approximately 15%).
The minimally invasive approach reduces hospitalization time by approximately five days, with significantly less blood loss and medication requirements, so that open adenoma enucleations have not been performed at the Prostate Center since 2011.
CONCLUSION FOR PRACTICE
- Up to 80% of 60- to 80-year-olds have BPH, but only 40% are symptomatic.
- Patients should receive early urological evaluation.
- Medications improve symptoms more than measurable parameters.
- TURP remains the reference standard.
- Holmium laser enucleation of the prostate is becoming the gold standard, especially for large organs.
Bibliography with the author
HAUSARZT PRAXIS 2013; 8(11): 12-16