A 55-year-old patient complains of reflux symptomatology, but it is mainly manifested by atypical postprandial dyspnea with retrosternal pain accompanied by nausea.
Background: A 55-year-old male patient complains of reflux symptomatology, but mainly manifested by atypical postprandial dyspnea with retrosternal pain accompanied by nausea.
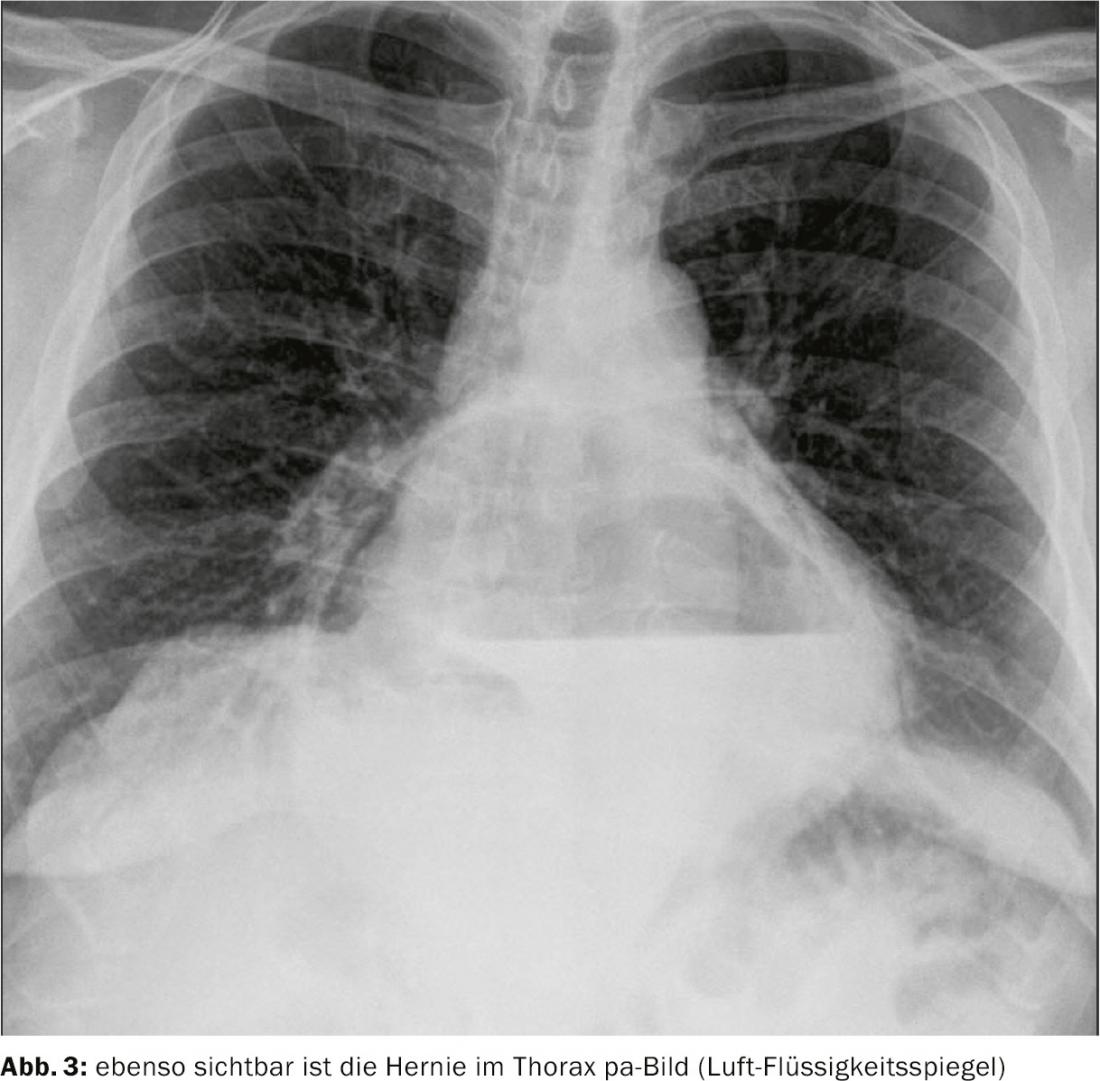
History and diagnosis: The patient presented to the gastroenterologist due to reflux symptoms with retrosternal pain. He stated that the complaints occurred mainly after meals. The further medical history also revealed a nicotine dependence and diabetes mellitus type 2. Further to be mentioned is a performed Lichtenstein operation inguinal right several years ago. The patient was already treated conservatively with Pantozol 40mg twice daily. Endoscopy and esophageal manometry and CT (thoracic) were performed to establish the diagnosis. These revealed a complete upside-down stomach with volvulus and acceptable esophageal motility.
Therapy: After conservative therapy failed to produce desired results, transhiatal mobilization of the stomach and esophagus and post- and anterior crurorrhaphy with Nissen fundoplication were performed. As a result, the symptoms improved rapidly and it was subsequently possible to switch to treatment with an alginate as needed.
 Comment by Yves Borbély, MD: The case impressively shows the presentation or symptomatology. Thus, postprandial dyspnea as an expression of gastric distension is not a classic reflux symptom. Further conservative therapy would not have been useful, since the main problem is structural and thus must also be treated surgically. If there is not a high burden of comorbidities, the indication for surgery in such a situation is given. Possible complications with further conservative therapy include dysphagia/aphagia with progressive volvulus, pain, or entrapment with necrosis.
Comment by Yves Borbély, MD: The case impressively shows the presentation or symptomatology. Thus, postprandial dyspnea as an expression of gastric distension is not a classic reflux symptom. Further conservative therapy would not have been useful, since the main problem is structural and thus must also be treated surgically. If there is not a high burden of comorbidities, the indication for surgery in such a situation is given. Possible complications with further conservative therapy include dysphagia/aphagia with progressive volvulus, pain, or entrapment with necrosis.
For the patient, this means that some risk of recurrence remains. In addition, a history of inguinal hernia surgery is suggestive of generalized connective tissue weakness. Fundoplication may temporarily cause some gastroparesis. In connection with an improved food intake, both quantitatively and qualitatively, reflux symptoms are still possible intermittently with fatty foods. These can be relieved by PPI or an alginate.