Women with obesity show an increased risk of poor contraception and unplanned pregnancies, as well as complications with hormonal contraceptives. Data regarding efficacy, effects on coagulation parameters and metabolism are inconsistent. Mild to moderate obesity without concomitant pathology (hypertension, diabetes mellitus, lipid metabolic disorder) is not per se a contraindication to combined hormonal contraception, but it leads to a significant increase in the risk of thromboembolism. For BMI of 35 kg/m2 and above, the risks usually outweigh the benefits. The following article goes into more detail about these risks and a possible influence of obesity on contraceptive effectiveness.
At first glance, it may seem surprising that obese women are at a higher risk for unwanted pregnancies, since a lower pregnancy rate would be expected as a result of the frequently associated PCO syndrome. However, various studies have shown that obese women, especially adolescents, are not only more likely than normal-weight women to have unwanted pregnancies, but also more likely to have abortions.
This is due to a variety of reasons, but the studies clearly show a lack of physician consultation and poorer compliance. Obviously, the need for contraception in obese women is underestimated. On the one hand, physicians are less likely to refer obese women to sexuality and contraception, presumably because sexual activity is less likely to be assumed.
On the other hand, many obese women suffer from a lack of self-confidence and are less confident to approach the doctor about such an intimate topic. The lack of self-confidence is also blamed for the poorer compliance of obese women as well as the overall higher risk behavior, also regarding condom use. The association of self-esteem, negative body image, and lack of contraception is well known from adolescent gynecology – even in underweight girls. It is therefore advisable to assume sexual activity when counseling obese women, to inquire about contraception as a matter of course, and to counsel carefully accordingly. The risks of contraception tend to be overestimated, whereas the risks of pregnancy tend to be underestimated [1]. Any contraception for obesity is better than none [2].
Risks of combined hormonal contraception
One possible reason for the lack of contraception is fear of its risks, among physicians as well as patients. Unfortunately, the data are insufficient because most studies exclude overweight patients. In the USA, adults of normal weight are already in the minority.
Thromboembolism is one of the feared complications of combined hormonal contraceptives. Various studies show an increase in risk with increase in BMI or body weight in kg. The following relationship can be derived from the MEGA study [3]: Compared to normal weight individuals, mild obesity without hormonal contraception increases the risk of TE by 1.7, and obesity by 2.4. When obesity (BMI >30) and combined pill are combined, the risk increases 24-fold. According to Abdollahi [4], obese OC users face a tenfold increased risk compared to normal weight women.
One possible explanation for the increased risk of thrombosis is an increase in inflammatory parameters (fibrinogen, CRP, plasminogen activator inhibitor-I) in obese compared with normal-weight patients [5].
Cardiovascular complications: Less clear is an influence of BMI on arterial thigh, as study results are contradictory. According to the MMWR, obese OC users are not thought to be at increased risk compared with normal weight users. Interestingly, with regard to cardiac risks, the third-generation progestogens (desogestrel and gestodene) appear to be more favorable than the second generation [6].
In contrast, combined contraceptives are clearly contraindicated (level 4) in ischemic or complex valvular heart disease and in the presence of multiple cardiac risk factors. Here, regardless of BMI, progestin-only contraception (estrogen-free pill, Implanon®, Mirena®) or hormone-free contraception (copper IUD, mechanical contraception) are recommended, depending on the condition.
Influence of overweight on effectiveness
The idea that increased body weight affects the distribution and thus the concentration and effect of a hormonal contraceptive is obvious. Unfortunately, however, the data are poor because most studies exclude overweight women and the available data were predominantly collected retrospectively. In summary, the main results:
- For implants, older studies show contradictory data, but according to two recent studies Implanon® can be recommended without restriction also in obese patients [7].
- For the subcutaneously administered depot MPA (Sayana®), increased follicle maturation was demonstrated in obese women, but no evidence for ovulation was found. It thus appears to have the same contraceptive safety as the intramuscularly applied preparation (Depot-Provera®). However, the data situation is still very limited. In the case of i.m. application in obese women, care must be taken to ensure sufficient depth of application.
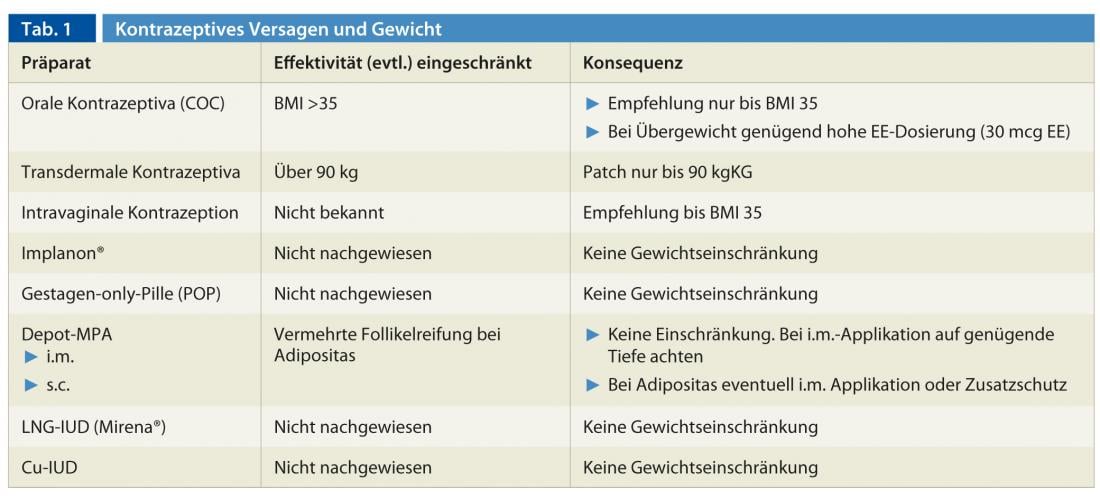
- In the case of combined hormonal contraceptives, the form of application also plays a role. For transdermal contraception (Evra-patch®), safety is reduced in women weighing more than 90 kg; BMI was not studied. For oral contraceptives, Dinger [8] shows a risk increase for contraceptive failure by a factor of 1.5 for a BMI >35. However, other studies show no correlation of BMI and contraceptive failure. Holt [9], in a retrospective analysis, found an increase in contraceptive failure in women over 70 kgKG and an association with hormone dosage: for low-dose preparations, the OR was 2.6; for very-low-dose preparations, the OR was 4.5. In summary, obese women must be assumed to have weaker ovarian suppression, although ovulation usually does not occur thanks to potent progestogens. Low-dose preparations should rather be avoided ( Table 1).
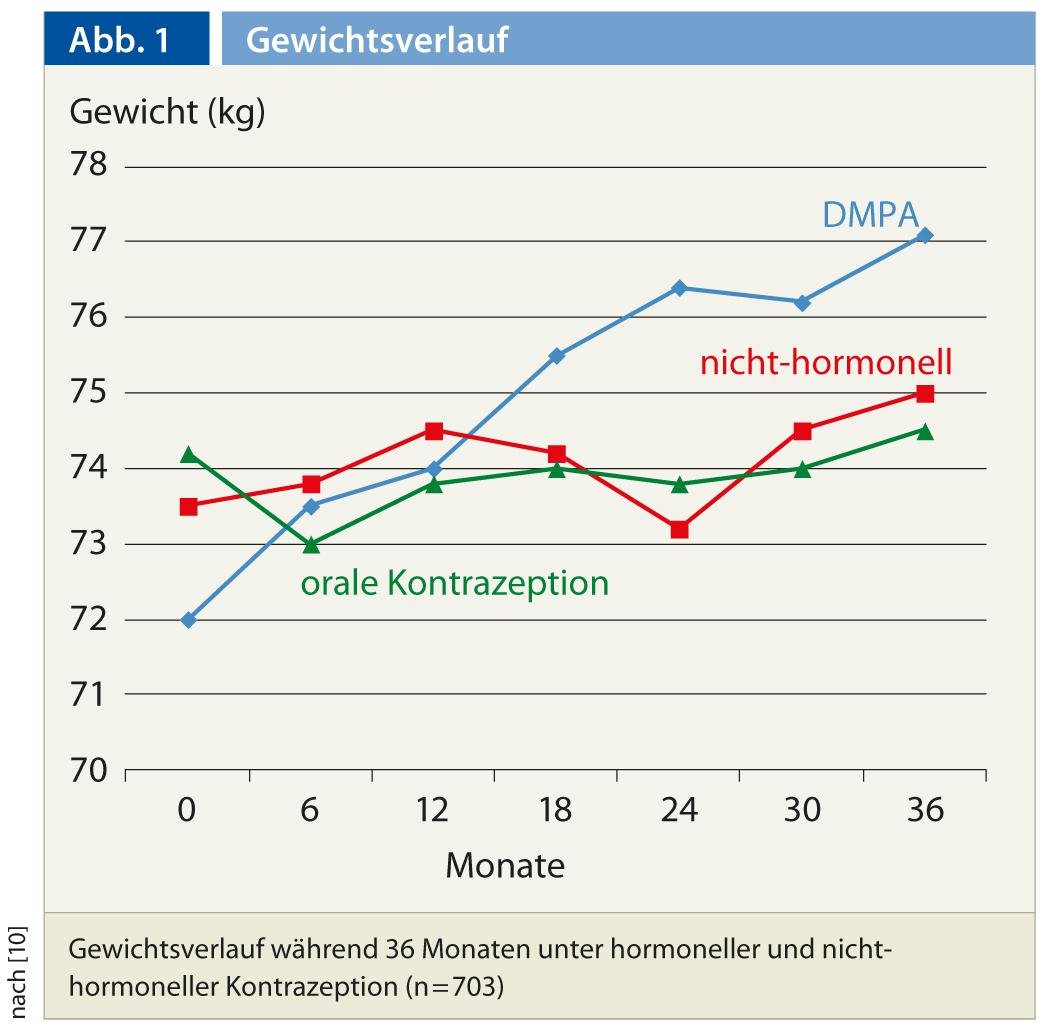
Effects of contraceptives on body weight
Many women who are overweight fear gaining more weight by using a contraceptive method. This fear should be actively addressed and taken seriously, as it can negatively impact compliance. Unfortunately, data on the course of weight under contraceptives are usually only available from normal-weight patients. One small study compared weight outcomes under oral and intravaginal contraception in different BMI groups, with obese women showing no greater effect than normal-weight women. Evidence of an above-average influence on weight is only available under the three-month injection (depot MPA) (Fig. 1) [10].
Conclusion for practice
- Obese patients are at higher risk for unplanned pregnancy, are less likely to receive medical advice, and have poorer compliance, even though pregnancy risks are greater.
- In cases of mild to moderate obesity without additional risks, all contraceptive methods can be chosen.
- For combined hormonal methods, the risks generally exceed the benefits above BMI 35.
- The contraceptive patch (Evra®) is recommended only up to 90 kg.
- Increased weight gain is only expected with the three-month injection (Depot-Provera®).
- In counseling obese women, long-term contraceptives can be offered as the first choice: The subdermal implant (Implanon®), the progestin-releasing intrauterine system (Mirena®), and the copper IUD.
Helpful websites for recommending contraceptives for medical problems:
www.who.int/reproductivehealth/publications/family_planning
Medical eligibility criteria for contraceptive use 2010
www.fsrh.org/pdfs/UKMEC2009.pdf
UK Medical Eligibility Criteria for Contraceptive Use 2009
Ruth Draths, MD
Literature:
- Rodriguez MI: Rev Endocr Metab Disord 2011; 12: 85-91.
- Shaw KA, Edelman AB: Best Pract Res Clin Endocrinol Metab 2013; 27: 55-65.
- Pomp et al: Br J Haematol 2007; 139: 289-96.
- Abdollahi M, et al: Thromb Haemost 2003; 89: 493-8.
- Sonnevi K, et al: Blood Coagul Fibrinolysis 2013; 24: 547-53.
- Lidegaard Ø, et al: N Engl J Med 2012; 366: 2257-66.
- Xu H: Obstet Gynecol 2012; 120: 21-6.
- Dinger J, et al: Obstet Gynecol 2011; 117: 33-40.
- Holt VL, et al: Obstet Gynecol 2005; 105: 46-52.
- Berenson AB: Am J Obstet Gynecol 2009; 200: 329.e1-8.