It would be a dream: to identify patients in the early stages of rheumatoid arthritis (pre-RA) and to prevent the manifestation of the disease through efficient countermeasures. Is this also realistic? At a symposium during the European League Against Rheumatism (EULAR) Congress in Madrid in June 2017, opportunities in different risk groups were discussed.
“Accurate prediction of disease development is considered the holy grail of risk factor research,” said Dr. Diane van der Woude of Leiden University Rheumatology Hospital in the Netherlands. In a comparatively rare disease such as rheumatoid arthritis (RA), with a prevalence of around 1%, prediction becomes a feat that can hardly be achieved, at least in the general population. In participants of the Nurses’ Health Study, attempts have been made to estimate RA risk based on genetic and environmental factors and autoantibodies in the blood, van der Woude reported, but with limited success. “If you have a very low risk of disease, you need an incredibly good biomarker,” the rheumatologist emphasized. Therefore, prevention strategies are currently focused on groups of people with signs and symptoms of rheumatologic disease.
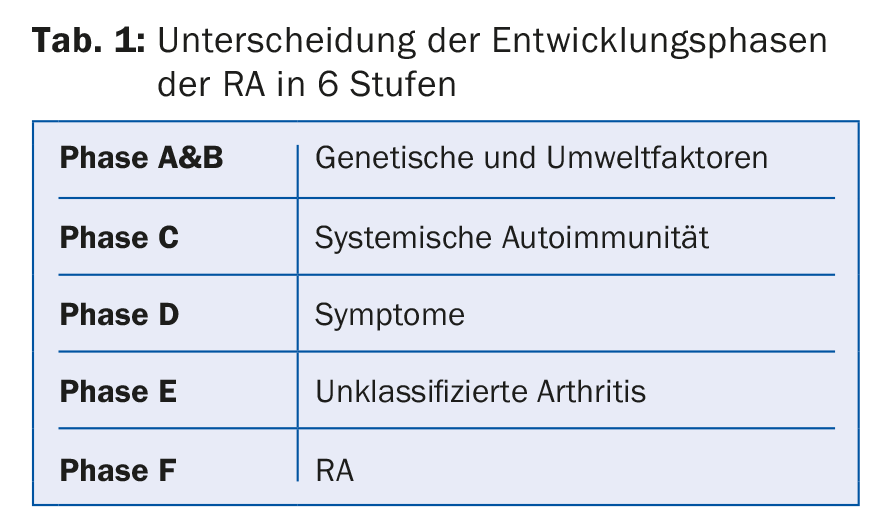
Six phases are distinguished by EULAR in the development of RA [1] (Table 1) . Phases A and B indicate an increased risk due to genetic and environmental factors. More than 100 genetic risk factors for RA have been identified to date, primarily variants in the HLA (human leucocyte antigen) system, reported Dr. René Toes, also based in Leiden. The genetic contribution to the onset of RA is estimated to be about 40%, according to van der Woude. According to them, not only risks of certain gene variants have to be taken into account, but also protective effects. Among environmental factors, smoking has the highest significance, especially in seropositive patients. The impact of smoking relative to overall risk is estimated to be %-35%. Other factors that may increase the risk of RA are low education level, high birth weight, obesity, environmental pollution, hormonal factors and periodontitis. Moderate alcohol consumption and breastfeeding may have a protective effect [2].
In particular, a publication on the possible association between periodontitis and RA last year caused quite a stir [3]. It was suspected that the bacterium Aggregatibacter actinomycetemcomitans, which secretes leukotoxin A (LtxA) and is frequently detected in the oral cavity of periodontitis patients, could trigger autoimmune processes, van der Woude reported. In fact, anti-LtxA antibodies have already been detected in RA patients; however, according to recent studies, it is again unclear whether LtxA actually play a role in the development of autoimmunity.
Systemic autoimmunity characterizes phase C of RA development. Autoantibodies such as ACPA (anti-citrullinated protein antibodies) can often be detected years before RA symptoms develop, Toes reported, but are also too nonspecific to predict RA. There are probably two steps associated with autoantibodies in RA development. In the first phase, ACPA formation possibly occurs via environmental factors. Only in the second phase, which is triggered by an interaction with HLA molecules, is further progression to RA then initiated. It should be noted that autoantibodies including rheumatoid factor are detected in only %–70% of RA patients.
Prevention efforts appear promising in patients who already have rheumatologic symptoms (phase D) or who have developed arthritis that is not yet classifiable (stage E) is present and who often develop manifest RA in the further course (phase F).
When arthralgia is clinically suspected, the following criteria indicate a high risk of progression, according to EULAR, van der Woude said:
- Symptoms in the metacarpophalangeal joints of the fingers
- (MCP joints) or pressure sensitivity.
- Morning stiffness >60 minutes
- Strongest symptoms in the morning
- Difficulty making a fist
- First-degree relatives with RA.
A prediction model of RA developed in the Netherlands based on 9 biomarkers, including mainly clinical criteria (symptom onset <12 months, symptoms in upper and lower extremities, pain intensity VAS >50 mm, swollen joints) and laboratory parameters (rheumatoid factor-, ACPA-positive), has also proven useful. Patients with high scores had a very high risk of developing manifest RA in the next one to five years, reported Kevin Deane, M.D., of the University of California at Aurora. He recommended early intervention in such patients to prevent or at least delay the development of RA.
First on the list are lifestyle interventions such as smoking cessation, and possibly omega-3 fatty acid intake would also have a beneficial effect, Deane said. Studies are also already investigating the use of classic RA drugs such as methotrexate (MTX) and hydroxychloroquine, and even biologics, in patients with a significantly increased risk of RA. A meta-analysis of data from 7 randomized controlled trials in a total of 800 patients with undifferentiated arthritis or ACPA-positive arthralgias documented the benefit of 1 year of therapy with MTX, methylprednisone, with a TNF blocker, abatacept, or rituximab. The risk of RA at the end of the study after one year was reduced by a mean of 28% in the verum groups compared to placebo [4].
In the U.S., the StopRA trial is currently ongoing in patients with at least twofold elevated APCA levels and an estimated 50% risk of developing RA in the next three years. Patients in the verum group will be treated with hydroxychloroquine for one year, after which the risk of RA will be monitored for an additional two years compared to the control group. The hope is to achieve a reset of the immune system through transient immunotherapy, Deane said. The initial data are hopeful, but further studies and more knowledge of the pathophysiology of RA are needed, he said.
Source: EULAR 2017, Madrid; Session “From pre-RA to established RA”, June 16, 2017.
Literature:
- Gerlag DM et al: EULAR recommendations for terminology and research in individuals at risk of rheumatoid arthritis: report from the Study Group for Risk Factors for Rheumatoid Arthritis. Ann Rheum Dis 2012; 71: 638-641.
- Karlsson EW et al: Strategies to predict rheumatoid arthritis development in at-risk populations. Rheumatology 2016; 55(1): 6-15.
- Konig MF et al: Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci Transl Med 2016; 8(369): 369ra176.
- Hilliquin S et al: Early therapeutic intervention for pre-rheumatoid arthritis (pre-ra) patients significantly reduces risk of ra. EULAR 2017; Abstract OP0011.
HAUSARZT PRAXIS 2017; 12(7): 40-41











