In particular, older diabetics with a high BMI have an increased risk of a severe course and mortality rates are also higher compared to the general population. The interactions involved are extremely complex. Regular glucose control and maintenance of HbA1c target values are among the clinically relevant risk factors that can be influenced.
A study from China (n=1099) reported that 15% of hospitalized laboratory-confirmed age-mixed COVID-19 sufferers were diabetic [1,2]. Data from a health center in New York showed that the proportion of diabetic patients was higher in hospitalized corona patients than in nonhospitalized subgroups (31.8% vs. 5.4%) [3]. Across all of the COVID-19 patients included in this study, 15% were diabetes affected. A BMI >40 proved to be a major risk factor for hospitalization.
Risk of severe course is significantly increased
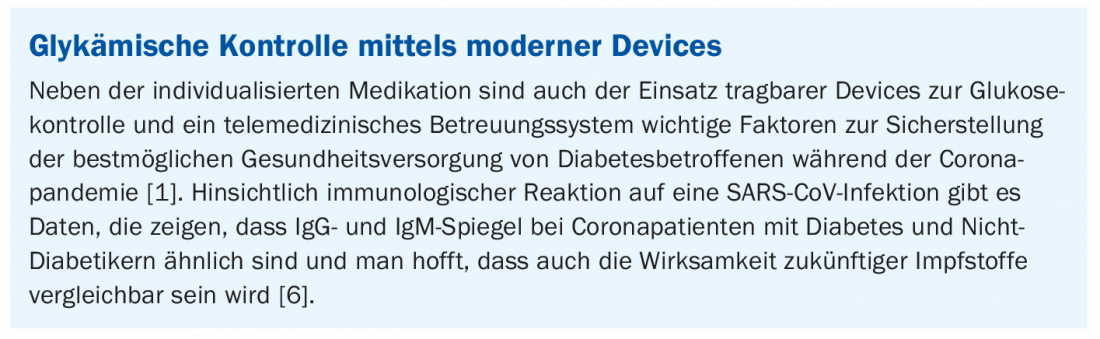
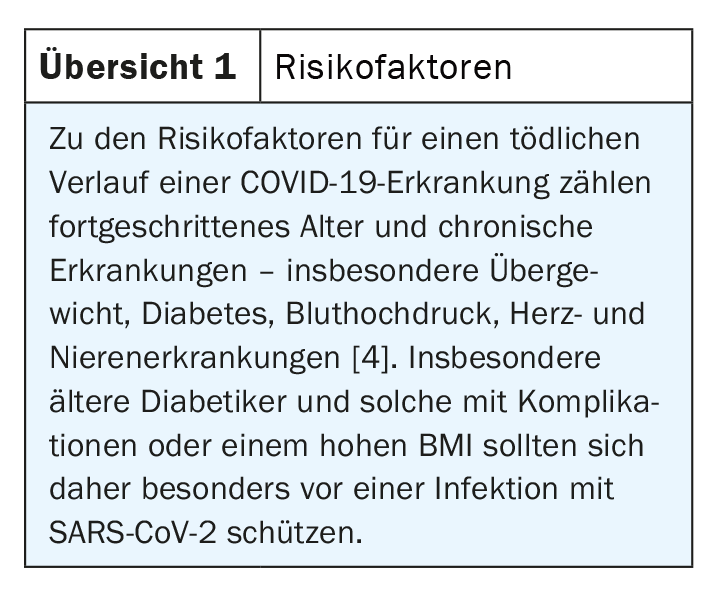
A search of PubMed shows that more than 2000 publications have appeared on COVID-19 and diabetes since the onset of the pandemic. Many of the articles report a correlation between high blood glucose levels and a severe course, including mechanical ventilation, ICU stay, and death, explains Prof. Juliana Chan, MD, of The Chinese University of Hong Kong and Prince of Wales Hospital, Shatin, Hong Kong [4]. According to a large British study (n=61,414,470), the prevalence of diabetes in the general population is 4.7%. The proportion of diabetes type 2 sufferers among 23 698 deaths of hospitalized COVID-19 patients was 31.4%, or nearly one-third [5]. The interaction structure involved is very complex. Glucose utilization in the organism depends on adequate oxygen availability and insulin, so that glucose is taken up by the cells and ensures vital functions. An acute stress such as COVID-19 disease can lead to destabilization of these interlocking processes resulting in uncontrolled glucose levels in the blood and multi-organ failure. It is well known that poorly adjusted glucose levels are associated with inflammatory processes and reduced resistance. As current data show. this is reflected in altered related parameters (e.g. IL6↑, lymphocytes↓, CRP↑) compared to COVID-19 patients without diabetes [8]. Older diabetics and those with microvascular and macrovascular complications or a high BMI are particularly at increased risk for a severe course with fatal consequences (review 1).
Gucose control as a modifiable risk factor.
Prof. Daniel J. Drucker, MD, of the Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, University of Toronto (Canada), emphasizes that glucose control is a modifiable risk factor. Good glycemic control reduces the risk for severe COVID-19 progression and is easier to influence than exemplary obesity, the speaker said. The pathophysiologic associations of the comorbidity of SARS-CoV-2 infection and diabetes are very complex, and there are numerous confounding variables. ACE2 (angiotensin-converting enzyme 2) and DPP4 (dipeptidyl peptidase-4) are two coronavirus receptor proteins that are also involved in metabolic signal transduction pathways and play important roles in glucose homeostasis. However, according to currently available data, there is no convincing evidence that drugs targeting ACE2- or DPP4-associated pathways lead to clinically relevant effects in SARS-CoV-2 infection [1,6]. What is certain is that glucose control is an important factor, even in this context. This is because hyperglycemia leads to reversible glycosylation of ACE2 receptors, which could facilitate coronavirus entry and thus lead to more severe infections. Whether DPP4 inhibitors have a relevant impact on clinical outcomes in diabetic patients with coronavirus infection cannot be assessed based on the current data [1]. In cases of diabetic patients with active SARS-CoV-2 infection and impaired renal function, it is suggested to possibly adjust the dosage of DPP4 inhibitors. Also with regard to other glucose-lowering substances, no evidence-based therapy recommendations can be made based on the current data situation, according to Prof. Drucker. The rapidly growing amount of data regarding SARS-CoV-2 requires continuous monitoring of emerging evidence to better understand the risks and benefits of glucose-lowering drugs in patients with COVID-19. This is also true for insulin-dependent cases, with decades of experience regarding the use of insulin in hospitalized diabetics in critical condition.
Type 1 diabetes: especially over 50-year-olds belong to the risk group
In a population-based UK study, hospitalized COVID-19 patients with type 2 diabetes were found to have a 3.5-fold increased risk of mortality compared with the general population, with a mean age of 72 years. With regard to type 1 diabetes, according to current data, only those over 50 years of age who have had diabetes for several years (80% for more than 15 years) and have an HbA1c >10% have an increased risk of a severe course, explains Prof. Catarina Limbert, MD, of the University Center of Central Lisbon & Hospital Dona Estefania, Lisbon, Portugal. [7]. Regarding possible correlations between the coronal pandemic and incidence figures, the speaker pointed out that previous multicenter studies did not show an increase in new diabetes type 1 cases during the coronal pandemic compared to the same period in previous years.
In terms of implications for treatment, the COVID-19 pandemic proved to be a booster for telemedicine, Prof. Limbert said. Although the digital revolution has been underway for some time with the use of insulin pumps, sensors, automated insulin administration, and virtual dosage recommendations, the coronary pandemic also highlighted the importance of remote care systems for assessing progress and making treatment decisions based on this information. Glycemic control was shown to improve with the use of advanced technologies, prompting healthcare providers to offer virtual diabetes clinics as a complement to conventional on-site visits. However, this would require multidisciplinary cooperation and it must be possible to guarantee the necessary technological know-how and practicable support. With regard to wearable diabetes devices, modern insulin pumps allow the selection of multiple basal rates and different bolus forms with different delivery delays.
Source: EASD 2020
Literature:
- Drucker DJ: Coronavirus Infections and Type 2 Diabetes – Shared Pathways with Therapeutic Implications. Endocrine Reviews 2020; 41(3): 457-470.
- Guan WJ, et al: New Eng J Med 2020. DOI: 10.1056/NEJMoa2002032.
- Petrilli CM, et al: Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. medRxiv 2020. doi:2020.2004.2008.20057794.
- Chan J: COVID-19 and diabetes: what is the evidence? Prof. Juliana Chan, Press conference, EASD, 22.09.2020.
- Barron E, et al: Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. The Lancet Diabetes & Endocrinology 2020; 8 (10): 813-822.
- Drucker DJ: COVID-19 and diabetes: what is the evidence? Prof. Daniel J. Drucker, Press conference, EASD, 22.09.2020.
- Limbert C: COVID-19 and diabetes: what is the evidence? Prof. Catarina Limbert, Press conference, EASD, 22.09.2020.
- Chan J: Overview on COVID-19 in persons with diabetes: What is the evidence? Prof. Juliana Chan, Press conference, EASD, 23.09.2020.
HAUSARZT PRAXIS 2020; 15(10): 50-51 (published 10/21/20, ahead of print).
CARDIOVASC 2020; 19(4): 32-33