Level 1 evidence is available for the benefit of additional BT in endometrial, cervical, and breast carcinoma. For example, it is an integral part of the therapy concept for endometrial carcinoma of the intermediate to high risk group as well as for definitive radio/chemotherapy of cervical carcinoma. However, it can also be used in many other indications for the purpose of organ preservation in the recurrence situation or for palliation.
Randomized data on the benefit of brachytherapy (BT) are available for numerous tumor localizations. However, in terms of frequency of use, three important indications can be highlighted in Switzerland for which level 1 evidence is available not only in terms of improvement of local control, but also overall survival and quality of life (Table 1). After providing the basics of brachytherapy in the first part of the review article, this second part will focus on the clinical use of the most common forms of BT. Numerous positive randomized studies are also available in prostate cancer, e.g., as a dose escalator in intermediate and high risk profiles, supporting its regular use internationally. In many other entities (such as ENT tumors, esophageal, anal, and rectal cancer), BT can be used especially with the goal of organ preservation or for palliation mostly based on small prospective, but majority retrospective studies.
Endometrial Cancer
Indication and Data: Surgery as hysterectomy with adnexectomy with or without surgical lymph node staging is the treatment of choice for endometrial carcinoma (EC). The use of adjuvant therapy options is based on the postoperative risk profile and consists of vaginal BT using a vaginal cylinder (VZ) with or without percutaneous pelvic radiotherapy (external-beam radi otherapy, EBRT) and adjuvant chemotherapy. The classical, purely clinical-histopathological risk stratification of EC, based on tumor infiltration depth into the myometrium (pT stage), tumor differentiation grade (G1-G3) and histological subtype (endometroid vs. non-endometroid) has been extended by molecular classification, which is now also integrated in the current guidelines [1,2]. The molecular classification results in a shift to a lower or higher risk profile compared to the classical classification, especially in the presence of a POLE (“DNA polymerase epsilon”) mutation (excellent prognosis) or a p53 mutation (worst prognosis). However, the predictive role of molecular stratification for radiotherapy remains largely unresolved. Adjuvant therapies reduce the risk of recurrence in EC and in certain situations also overall survival; the individual contribution of radiotherapy or chemotherapy cannot be clearly stated despite several large randomized trials (especially since the definitions of the risk categories differ slightly in each case). There is consensus regarding the indication of adjuvant BT for EC with an intermediate- or high-risk profile. Thus, more concretely and somewhat simplified, treatment by VZ should be recommended in an early stage patient with pT1b and/or deep differentiation (G3), from any stage ≥pT2 or in the presence of a p53 mutation [1,2].
In the rare situation of medically inoperable patients with EC, primary radiotherapy consisting of pelvic percutaneous radiation followed by intrauterine BT is a treatment option with long-lasting complete remission. In locoregional recurrences, interstitial BT can often still be used curatively even in preirradiated patients. In the following, however, only the practical implementation of the adjuvant setting, which is by far the most common, will be discussed.
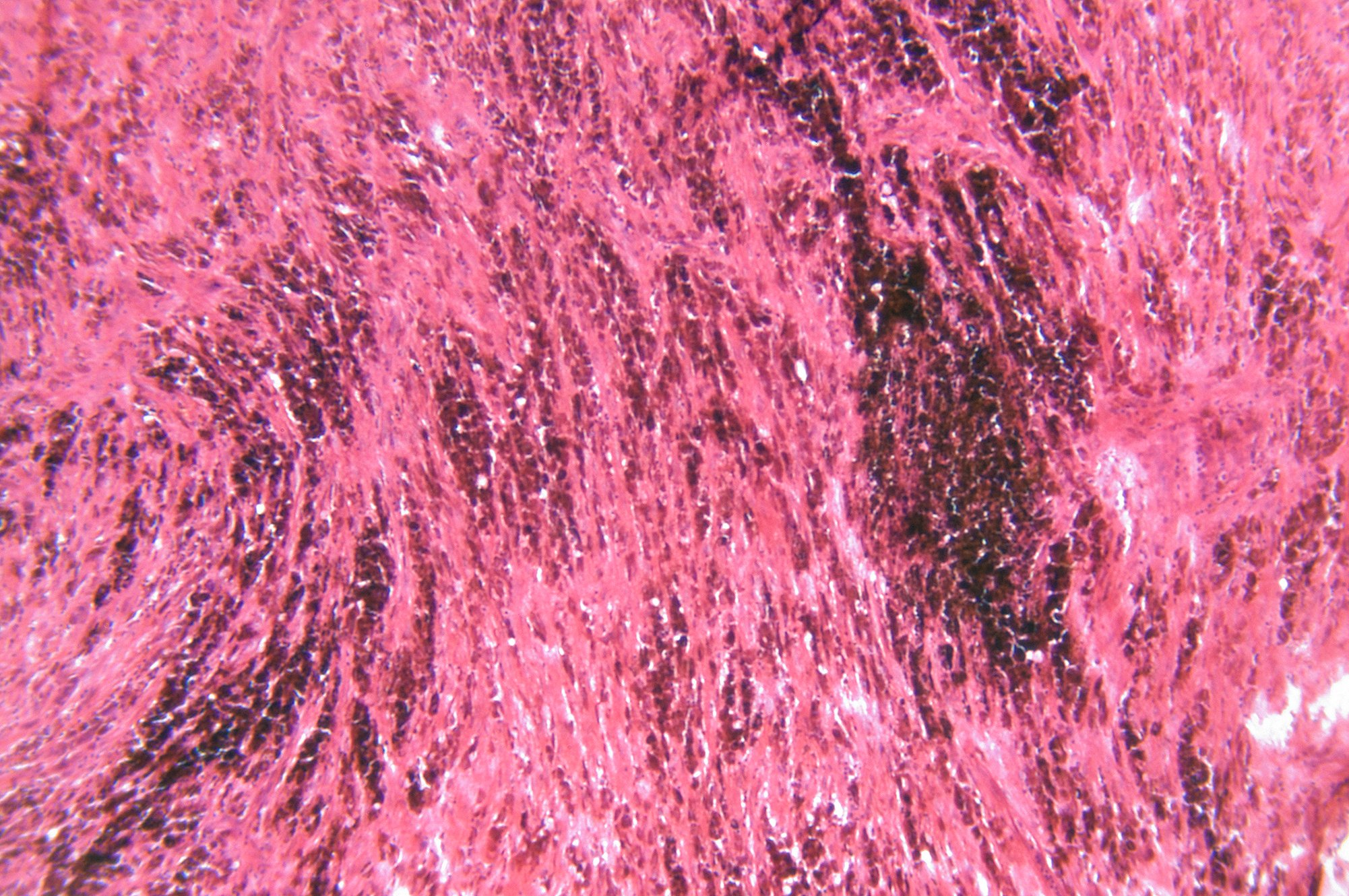
Practical implementation: Adjuvant intravaginal BT using VZ is offered in many centers throughout Switzerland. The main postoperative risk area for local recurrence, in addition to the settling scar, is the upper vaginal area, so treatment of the proximal third or half of the vagina (typically 3-5 cm) is recommended. The applicator insertion is performed in lithotomy position and is comparable to the insertion of an examination speculum for the patient. The diameter of the VZ is selected according to the individual anatomy. Based on the thickness of the vaginal wall, the dose is usually dosed to 5 mm tissue depth and the irradiation length is adjusted to the respective vaginal length (Fig. 1). After each radiation fraction, which takes only a few minutes thanks to the HDR (high-dose rate) afterloading technique, the VZ is removed. The total course of treatment lasts half an hour. Depending on whether imaging-guided radiation planning is performed during the initial insertion, the total treatment time may be extended by 1-2 hours. The dose fractionation (number of sessions and amount of single dose) depends on whether vaginal BT is performed alone or in combination with prior pelvic EBRT, but the technical procedure is the same (Table 1).
The side effect profile is favorable with only very rarely clinically relevant acute or late side effects. The most significant long-term major side effect of vaginal shortening and constriction can be reduced or largely avoided by regular use of vaginal dilators and topical measures.
Cervical Cancer
Indication and data: definitive combined radio/chemotherapy (RCT) is the international standard for any advanced cervical cancer. It consists of a min. 5 weeks of pelvic irradiation with concomitant chemotherapy (platinum-based) followed by BT as a dose boost [3,4]. Specifically, in cervical cancer, tumor stages are considered “advanced” if they are locally extensive or if there is lymph node involvement. Locally advanced cervical carcinomas have tumor size >4 cm (cT1b3), extensive vaginal involvement, or infiltrated parametria (≥cT2b). Borderline treatment decisions are made in early advanced stages cT1b2 (smaller tumors, 2-4 cm) and cT2a (limited vaginal involvement). Here, surgery can be a good alternative to definitive RCT with experienced surgeons and in center hospitals [3,4]. The combination of radical surgery and postoperative radiotherapy should be avoided whenever possible because it significantly increases morbidity and provides no advantage in overall survival. This underlines the importance of initial diagnostics to best assess whether an early stage is present and surgery alone is indicated, or whether the tumor is advanced and should be treated by definitive RCT. BT is rarely used in the context of postoperative radiotherapy.
Practical implementation: BT of cervical carcinoma requires more expertise and a well-coordinated overall treatment team, which is why patients are often assigned to center hospitals for this purpose. Several implantation techniques are available, with commercial applicators used in Switzerland. These consist of two components; an intrauterine pin which is inserted via the cervical canal and thus placed intrauterine, and an endovaginal component (a ring or two ovoid) which rests against the portio (see Figure 2, Part 1 of this review article). In case of extensive parametranal and/or vaginal residual after percutaneous RCT of several weeks, additional interstitial applicators are recommended for ideal tumor coverage. These interstitial catheters can be inserted from the outside using a hole arrangement on the inserted ring to target a predefined angle and distance. They enter the parametric tissue at the level of the vaginal fornix, thus increasing the lateral dose distribution by about 2 cm, which allows co-treatment of the parametria. If interstitial applicators are used, it is called combined intrauterine and interstitial brachytherapy. The total treatment time (calculated from the start of the first percutaneous radiotherapy) should be <50 days [5]. A common treatment regimen provides for 4 fractions of 7 Gy each (Table 1), although the period over which these are applied also depends on logistical resources of the clinic.
Only applicator insertion is performed under anesthesia (intubation anesthesia or spinal anesthesia). For the subsequent imaging, radiation planning and radiotherapy, the patient lies in bed with applicator. This is usually removed immediately following treatment, for which basic analgesia is often sufficient. In total, a fraction lasts an outpatient half-day.
Breast Cancer
Indication and Data: The role of adjuvant RT in breast carcinoma has increased in importance due to the widespread use of breast-conserving surgery. Interstitial BT is offered in breast carcinoma (1) as partial breast irradiation alone postoperatively, (2) as local dose saturation of the tumor bed together with percutaneous radiotherapy, or (3) in the recurrence of preirradiated patients.
Partial breast irradiation (PBI) alone, as an alternative to whole breast re-irradiation, is an established de-escalation strategy for early breast carcinoma with low risk of recurrence after complete tumor excision. Here, the irradiation volume is reduced to the extended tumor bed, resulting in a more favorable toxicity profile with better quality of life and non-inferiority related to local control or overall survival [6]. Prospective data are now available for other PBI techniques (e.g., also intraoperative single radiation treatment or percutaneous PBI), some with good results, but the best evidence with the longest follow-up is seen with interstitial BT described here [6,7].
The irradiation volume and technique used in interstitial BT boost is usually the same as that used in partial breast irradiation. In contrast, however, BT boost is used in combination with percutaneous whole-breast irradiation, so it is usually a form of desired therapy escalation in high-risk situations. The oncologic advantage of BT boost over other forms of dose repletion was not clearly demonstrated in a prospective head-to-head comparison [8]. Regardless of radiotherapy technique, boost in breast carcinoma achieves a reduction in local recurrence (especially in younger patients) without impacting overall survival.
In the recurrence situation, interstitial BT may be offered as an adjunct to the again breast-conserving approach. Larger retrospective evaluations achieved oncological results at least equivalent to salvage mastectomy with good tolerability.
Practical implementation: The steps of implantation technique and radiation planning are detailed in guidelines for the purpose of standardization [9,10]. The applicators for multicatheter BT can be placed already during or even after surgery (under general or local anesthesia). Guide needles are inserted into the tumor bed of the operated mamma via so-called templates (plastic templates with prefabricated hole arrangement) at regular, parallel intervals in 2-4 planes, guided by the image. After this, plastic catheters are pulled through the hollow guide needles and the rigid needles are removed. Knobs at the respective skin exit points guarantee that the applicators do not move during the treatment time. The target volume to be irradiated is defined as a 2 cm margin around the direct tumor bed, which is localized taking into account preoperative imaging, surgical scar, and surgical clips. The chest wall and skin are left out of the target volume. The subsequent irradiation takes place over a few days with classically two irradiation fractions per day.
Periinterventional side effects rarely include infection, bleeding, or pain. In the acute phase, PBI with BT results in fewer skin reactions compared with percutaneous whole-breast irradiation, and even in the longer follow-up after >10 years, the tolerability of BT is favorable, with reduction in the incidence of severe breast fibrosis [6].
For each of the listed RT indications, there are noninvasive treatment alternatives in breast carcinoma. The dosimetric advantage of BT with sparing of surrounding tissues (skin, heart, and lungs) is clear and has been shown to correlate with a lower late side effect rate and better cosmesis in many patients. In addition, the higher radiation dose per fraction, which is made possible by the steep dose gradient, allows a logistically favorable total treatment time of less than one week (Fig. 1) . The minimally invasive nature of BT must be balanced against these advantages and should be discussed with the patient given her risk profile.
Take-Home Messages
- Level 1 evidence is available for the benefit of additional BT in endometrial, cervical, and breast carcinoma.
- Partial breast irradiation with interstitial BT should be offered to low-risk patients after breast-conserving surgery because it reduces radiogenic side effects on the skin, lungs, and heart.
- BT is an integral part of the therapeutic concept for endometrial carcinoma of the intermediate to high risk group as well as for definitive radio/chemotherapy of cervical carcinoma.
- In many other indications, BT can be used for the purpose of organ preservation in the recurrence situation or for palliation.
Literature:
- Concin N, Matias-Guiu X, Vergote I, et al.: ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int J Gynecol Cancer 2021; 31(1): 12–39.
- Harkenrider MM, Abu-Rustum N, Albuquerque K, et al.: Radiation Therapy for Endometrial Cancer: An American Society for Radiation Oncology Clinical Practice Guideline. Pract Radiat Oncol 2023; 13(1): 41–66.
- Cibula D, Pötter R, Planchamp F, et al.: The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients With Cervical Cancer. Int J Gynecol Cancer 2018; 28(4): 641–655.
- Chino J, Annunziata CM, Beriwal S, et al.: Radiation Therapy for Cervical Cancer: Executive Summary of an ASTRO Clinical Practice Guideline. Pract Radiat Oncol 2020; 10(4): 220–234.
- Pötter R, Tanderup K, Schmid MP, et al.: MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. Lancet Oncol 2021; 22(4): 538–547.
- Strnad V, Polgár C, Ott OJ, et al.: Accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy compared with whole-breast irradiation with boost for early breast cancer: 10-year results of a GEC-ESTRO randomised, phase 3, non-inferiority trial. Lancet Oncol 2023; 24(3): 262–272.
- Offersen BV, Alsner J, Nielsen HM, et al.: Partial Breast Irradiation Versus Whole Breast Irradiation for Early Breast Cancer Patients in a Randomized Phase III Trial: The Danish Breast Cancer Group Partial Breast Irradiation Trial J Clin Oncol. 2022; 40(36): 4189–4197.
- Poortmans P, Bartelink H, Horiot JC, et al.: The influence of the boost technique on local control in breast conserving treatment in the EORTC “boost versus no boost” randomised trial. Radiother Oncol 2004; 72(1): 25–33.
- Strnad V, Hannoun-Levi J-M, Guinot J-L, et al.: Recommendations from GEC ESTRO Breast Cancer Working Group (I): Target definition and target delineation for accelerated or boost Partial Breast Irradiation using multicatheter interstitial brachytherapy after breast conserving closed cavity surgery. Radiother Oncol 2015; 115(3): 342–348.
- Strnad V, Major T, Polgar C, et al.: ESTRO-ACROP guideline: Interstitial multi-catheter breast brachytherapy as Accelerated Partial Breast Irradiation alone or as boost – GEC-ESTRO Breast Cancer Working Group practical recommendations. Radiother Oncol 2018; 128(3): 411–420.
InFo ONKOLOGIE & HÄMATOLOGIE 2023; 11(3): 6–9