At the fourth congress of the Young Family Physicians of Switzerland (JHaS) at the Thun Congress Center, Prof. Dr. Thomas Rosemann, MD, Zurich, on the tasks of today’s family doctor. How has demand changed? What is the role of the primary care provider in the overall medical system? And how can collaboration within this network be improved?
(ag) According to Prof. Dr. med. Thomas Rosemann from the Institute of Family Medicine at the University Hospital Zurich, the complexity of care is increasing, especially in the outpatient sector. Thus, the often lamented increase in chronic diseases and chronically ill patients is not a failure of the health care system, but rather the consequence of highly developed care, which makes it possible to survive and survive with chronic diseases in the first place. This shifts the morbidity burden from acute to chronic and multimorbid conditions, consultation needs from singular events to structured, continuous follow-up or monitoring, and the approach to care changes from reactive to proactive. “So care is clearly becoming more complex, seemingly a Herculean task,” concluded Prof. Rosemann.
The challenge in family practice is not to fall into a “more-is-more”, i.e. a Goliath strategy, in view of multimorbidity and complexity, i.e. to prescribe as many different drugs as possible. Quite apart from the threat of interactions, studies [1] show that discontinuity of use of different drugs need not result in significant side effects or directly related deaths. On the contrary, 88% of elderly patients even reported an overall improvement in health after partial discontinuation of medication.
According to Prof. Rosemann, it is also interesting to note a study [2] that came to the conclusion that diabetes mellitus patients who were treated only by their general practitioner were less likely to receive absolutely guideline-compliant treatment than those who saw a specialist, but they also died less frequently. This association persisted even in patients without comorbidities. The question of what negative consequences a possible “Goliath” therapy can have in addition to the pure improvement of certain disease values is therefore justified.
Primary care as a team approach
In any case, for the primary care physician to be able to fulfill his or her demanding task, a team approach is required, which is achieved, for example, through the more active involvement of medical office staff. In particular, MPAs could take on the following tasks, which would also mean upgrading the profession:
- Regular monitoring, proactive calling of patients
- Early detection of changes, faster response
- More active involvement in diagnosis and therapy.
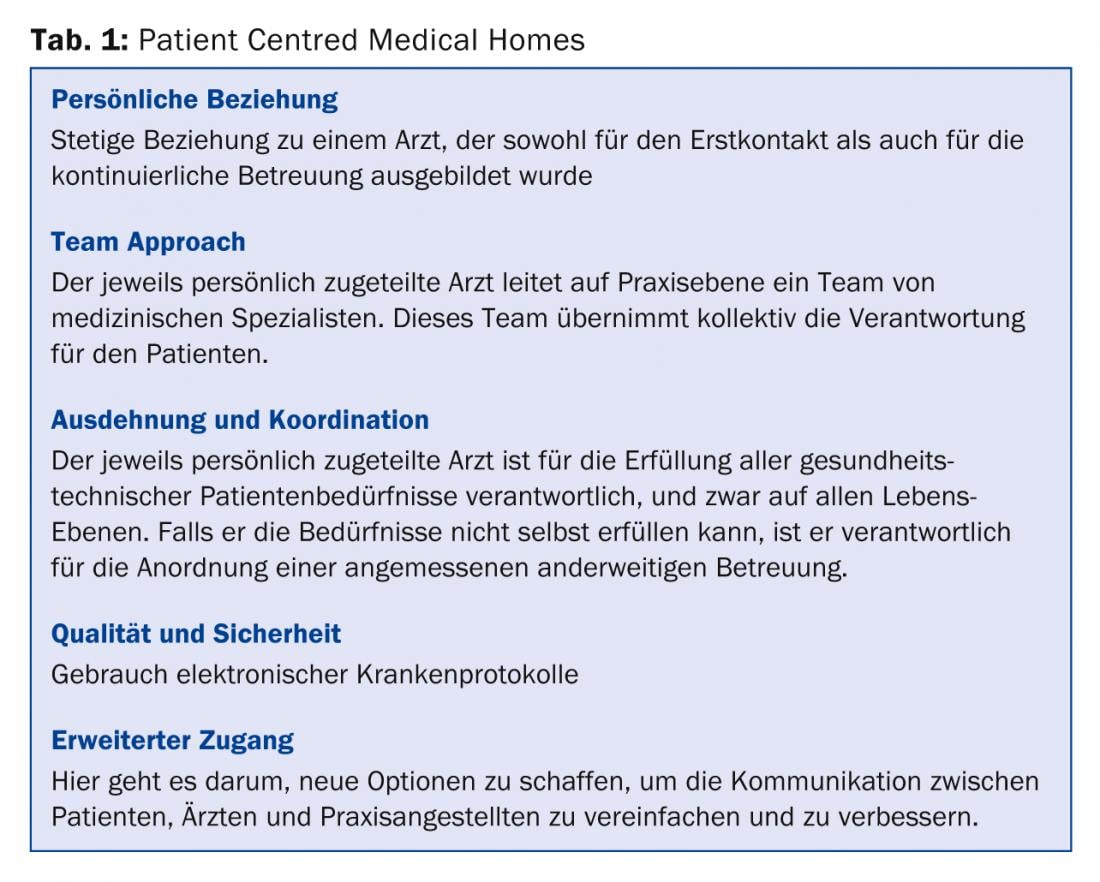
American models see so-called “Patient Centred Medical Homes” as the medical practices of the future. Table 1 shows the key points of this networked collaboration. In this context, the primary care physician is not only the caregiver, but also the coordinator of the network and the patient’s first point of contact. “This is a particularly important point for communication,” Prof. Rosemann explained. “Studies show that patients (e.g., with acute coronary syndrome) know little and only inaccurate information about their condition, i.e., their symptoms and possible treatment options, even after diagnosis and numerous interactions with physicians and other health care workers [3]. It is seemingly left to the primary care physician to gather all the information that the patient has already received, process it, and reproduce it in a way that is appropriate for the patient. A truly Herculean task, but one that is becoming increasingly important given the flood of information in the medical system. After all, surveys indicate that patients trust their family doctor the most when it comes to health issues, even ahead of specialists and clinicians.”
Growing into a Goliath at the Herculean task
In summary, according to Prof. Rosemann, demographics, medical progress and the commercialization of medicine are both a challenge and an opportunity for the family doctor. It thus increasingly fulfills the tasks that remain open elsewhere in the system:
- Advisor, companion and pilot in an increasingly fragmented and specialized health care system
- Coordinator of co-morbidity and multimorbidity and tightrope walker between “evidence” and individuality
- Manager/Player in an interdisciplinary team with defined tasks
- Landlord and confidant in the patient-centered “medical home.”
Source: “Family doctor – David, Goliath or Hercules”, lecture at the 4th JHaS Congress, April 5, 2014, Thun
Literature:
- Garfinkel D, Mangin D: Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med 2010 Oct 11; 170(18): 1648-1654. doi: 10.1001/archinternmed.2010.355.
- McAlister FA, et al: The effect of specialist care within the first year on subsequent outcomes in 24,232 adults with new-onset diabetes mellitus: population-based cohort study. Qual Saf Health Care 2007 Feb; 16(1): 6-11.
- Dracup K, et al: Acute coronary syndrome: what do patients know? Arch Intern Med2008 May 26; 168(10): 1049-1054. doi: 10.1001/archinte.168.10.1049.
HAUSARZT PRAXIS 2014; 9(5): 40-41











