COPD is associated with high morbidity and mortality. It is currently the fourth leading cause of death worldwide, and according to a prediction by the Global Burden of Disease Study, it will be the third leading cause by 2020. There is a high prevalence and a high rate of admission and, as a result, a large loss of work days. So where do we currently stand in therapy as GOLD continues to bring forward new changes?
“These changes are generally justified. After all, they also lead to us improving the whole thing,” said Prof. Dr. Michael Dreher, Clinic for Pneumology and Internal Intensive Care Medicine, Medical Clinic V, University Hospital RWTH Aachen, at the 60th Congress of the DGP in Munich. However, the expert also admitted that when he first looked at GOLD 2019, he had thought that many things would now become complicated again, that many things would change, and that patients would have to be told anew what to do. “But actually, it’s not that hard and not that far away from the clinical routine and what we do anyway.” Prof. Dreher used the GOLD recommendations to classify the importance of inhaled corticosteroids (ICS) in the treatment of COPD – not without pointing out that none of this is set in stone, because it is always individual decisions that physicians have to make.
Basically, when a COPD patient presents for the first time and he has not yet had any therapy, he is still divided into risk groups: Group A and B the patients who are symptomatic, and Group C and D the patients who exacerbate frequently. From this, consideration is given to how best to adjust the therapy. In initial therapy, few patients are likely to benefit from inhaled steroids. They are only used in group D in the combination ICS/LABA. The IMPACT trial, one of the largest trials in COPD, compared triple therapy LAMA/LABA/ICS vs. In the rate of severe and moderate exacerbations, triple therapy performed significantly better compared with maximal bronchodilation. However, LABA/ICS was also better compared with maximal bronchodilation. One criticism in the past had been that this primarily included patients with a certain degree of reversibility. But then again, according to the expert, it is very likely these same patients in the initial presentation where you have to worry about the inhaled steroid. “If we’re not 100% sure if it’s asthma or COPD, if the patient has reversibility, then ICS certainly plays a role in COPD.”
Many roads lead to triple therapy
What should be avoided, however, is a patient receiving triple therapy in initial treatment. In 2016, the FLAME trial compared LAMA/LABA vs ICS/LABA and showed that LAMA/LABA was significantly less associated with exacerbations than the ICS/LABA combo. Therefore, dual bronchodilation is certainly warranted in the first serve in a patient in group D. The majority of patients in FLAME had fewer than two moderate or severe exacerbations in the past year, in which case patients likely benefited as well. IMPACT, on the other hand, had a patient population that was significantly sicker and had a higher rate of exacerbations, meaning ICS are certainly well indicated there. When FLAME and IMPACT are compared, it is found that there is no difference between maximal bronchodilation and the LABA/ICS combo, but there is a difference when there are two or more moderate exacerbations or one severe exacerbation. “So it’s always a very crucial question: what kind of patient are we talking about? If we then make the right indication, we can also help these people very well with an ICS.”
Prof. Dreher was not prepared to accept the accusation that too many ICS are prescribed in Germany. In making his case, he cited data from the DACCORD registry, which includes nearly 6000 patients. ICS are prescribed in over 30% of patients here, which is not that much according to the pulmonologist. Rather, he said, the problem is that the ICS is often applied in GOLD A or B as well. “And it really has relatively little to do in GOLD A.” The 30% mentioned are figures from Germany. When the three large triple trials, IMPACT, TRIBUTE, and KRONOS, are evaluated according to how many patients were on ICS before they were randomized, the numbers range from 60 (IMPACT, TRIBUTE) to 70% (KRONOS).
The KRONOS trial compared the fixed-dose triple vs LABA/ICS vs LAMA/LABA. Inclusion criteria here were moderate to very severe COPD, FEV1 at less than 80 and greater than 25%, patients had to be symptomatic but did not need a history of exacerbation. So the question here was: does triple therapy work in symptomatic patients who have no history of exacerbations? “Conversely, you can also say, does it work in all COPD patients?” the expert pointed out. This is because the DACCORD registry lists only 3% of the total 6000 patients as asymptomatic.
However, when indicated, the ICS works very well in KRONOS. Again, there were significantly fewer exacerbations than compared with the LAMA/LABA and LABA/ICS combos. However, not only the exacerbation history should be included in the question of when COPD patients benefit from inhaled steroids, but also the number of eosinophils. GOLD has defined 2 clear thresholds: Below 100 eosinophils it makes relatively little sense to think about an ICS, and above 300 EOS it is certainly justified.
Keeping an eye on the eosinophils
Thus, the patients who exacerbate frequently and have blood eosinophilia are most likely to benefit from an inhaled steroid. But could more patients possibly benefit from an ICS? In daily practice, the DACCORD data suggest, one is quite rarely confronted with exacerbating COPD patients. At least in this cohort, the exacerbation rate was only 0.38. This is very low and also lower than in the prospective studies. (For TRIBUTE 0.5-0.6, KRONOS 0.5-0.95, and IMPACT 0.9-1.2.) According to Prof. Dreher, it can certainly be assumed that exacerbations are lost to us in everyday clinical practice. The basic problem: If an exacerbating patient is given cortisone and notices that it makes him feel great, he may not even go to the doctor next time, but take the tablets himself.
Last but not least, the pulmonologist encouraged the principle that less is more: “If I have mild/moderate COPD and few exarcerbations, then I have to be fair enough to question the point of ICS as well.” Not only always escalating, but de-escalating can lead to success in some cases. The SUNSET study included exactly this patient population. FEV1 was 40-80% of target, there was no more than one moderate/severe exacerbation in the past year, and at least 6 months of triple therapy. In the study was randomized to triple therapy or indacaterol/glycopyrronium and placebo, the primary endpoint was non-inferiority of lung function. This was not shown. When ICS was taken out, the patient lost a mean of 26 ml FEV1, but there were no more exacerbations (secondary endpoint). And again, it became clear: More exacerbations without ICS are received by those patients who have a high blood eosinophilia, i.e. 300 or more.
What’s new in asthma?
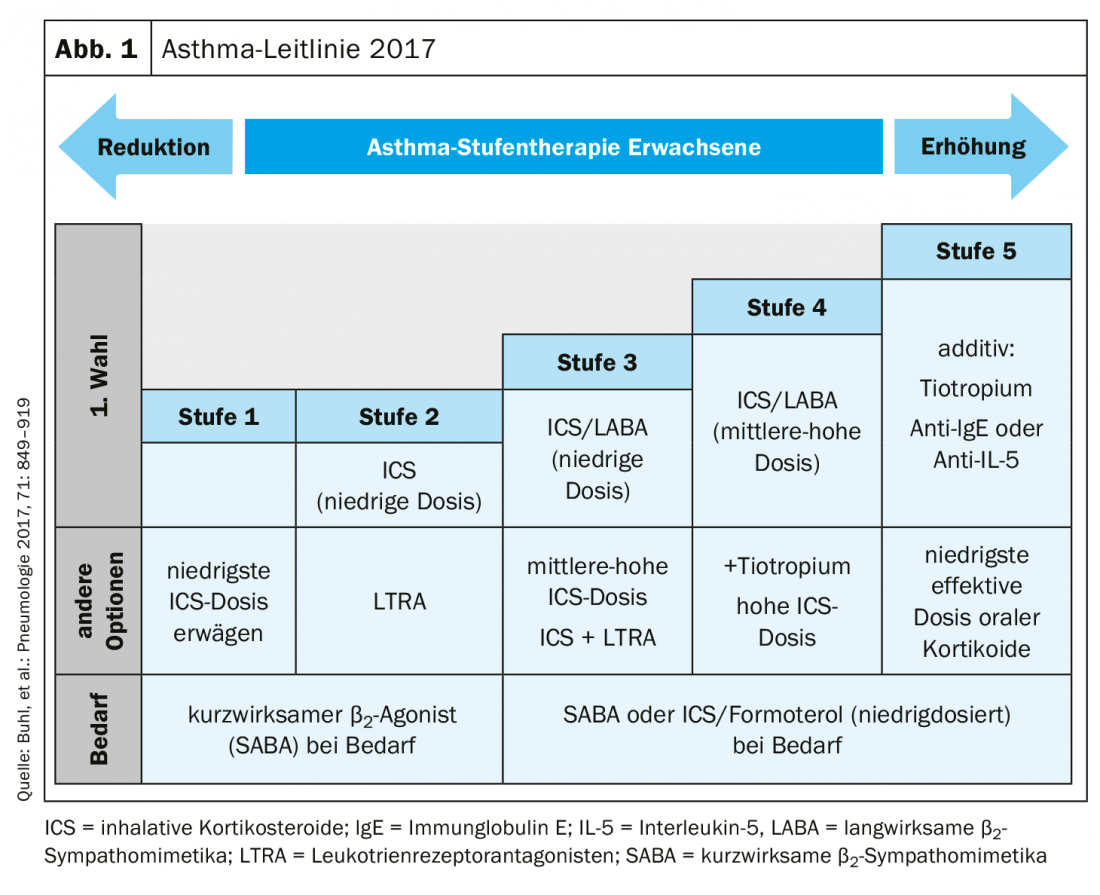
The usefulness of the use of inhaled corticosteroids was also the focus of the lecture by Prof. Dr. Andreas R. Koczulla, University Hospital Marburg, with a special focus on asthma. The expert first reminded the audience of the new National Health Care Guideline (NVL) on asthma, published in September 2018, which includes the well-known tiered regimen listing low, medium, and high dosing.
He defined the therapeutic goals of ICS use as follows: shut down proinflammatory cytokines and upregulate anti-inflammatory genes; reduce inflammatory cells and ultimately improve clinical symptoms in the patient; the epithelial relief, which can become dysregulated in the context of asthma, should also re-harmonize. However, the road to these goals can be rocky, especially considering the possible side effects.
Fluticasone propionate has an ICS dose recommendation for low of 100-250, medium 250-500 and high over 500 according to GINA. In the NVL, a maximum dose form is provided at ≥1000 µg. A recent paper took on the task of how much dose is needed to reach the maximum in FEV1. “You reach 80% of the maximum with 146 µg of fluticasone propionate. If you want to increase to 90%, increase the dose to 209 µg. However, the higher the dosage, the more severe the systemic side effects. These include adrenal insufficiency, cataracts, fractures and diabetes.”
The patient does what he wants – that’s good!
Patients often act more according to their symptoms, and if the symptoms are not particularly pronounced, they often take a little less of their medication, so they adjust their medication on their own. Prof. Koczulla expressed concern that only 3.3% of all asthma patients are included in the classic randomized controlled trials. “Do we really cover our everyday life with such studies?” The speaker therefore presented another real-life study, the so-called Salford study, which compared a standard therapy with an ICS/LABA combination. More responders were seen in the ICS/LABA (fluticasone furoate/vilanterol) combo (71%) than in standard therapy (56%). A responder was a patient with an improvement in the ACT either by three or more points or to a total of 20 or more points. “So that worked well here, and certainly worth noting is that there were no significant differences between FF/VI and standard therapy in terms of exacerbations and side effects,” the pulmonologist summarized.
In view of the results, colleague Dreher interjected that we are on the way to dividing patients into two groups first: those who are doing well and with whom individual therapy concepts can be developed to see whether something can also be saved. And the other group with the severe ones, where antibodies have to be considered and where the physician has to make sure that the patient is out of treatment before talking about alternatives. Prof. Koczulla agreed: “It’s clearly going in the direction of individualization. And maybe those who are doing well can really just be queried digitally, they’ll send a smiley and you won’t see them again for another six months.”
Summary
- ICS are rarely appropriate at initial diagnosis, but probably not at all uncommon later in the course of the disease. Namely, when a patient exacerbates frequently.
- If the eosinophils are also brought on board, good groups of substances are now available to reduce exacerbations.
- But one should not only escalate, but also always question: Possibly a de-escalation makes more sense.
- Increased ICS doses also increase the rate of side effects.
- Need-based therapy leads to savings effects.
- There is little data for the maximum dose range (data from randomized controlled trials show that as-needed therapy is possible, the real-life study has also shown that the ICS/LABA combo works relatively well).
Source: Industry Symposium “ICS in Asthma and COPD – Therapy in Changing Times”, as part of the 60th Congress of the DGP; Organizer: Berlin Chemie.
InFo PNEUMOLOGY & ALLERGOLOGY 2019, 1(1): 26-27.











