Depending on its course, multiple sclerosis can lead to rapid losses in quality of life. Research is working at full speed to further detect the pathology of the disease and to provide targeted measures for diagnosis and therapy. In addition to new biomarkers that primarily facilitate differential diagnosis, effective compounds are also available to halt demyelination.
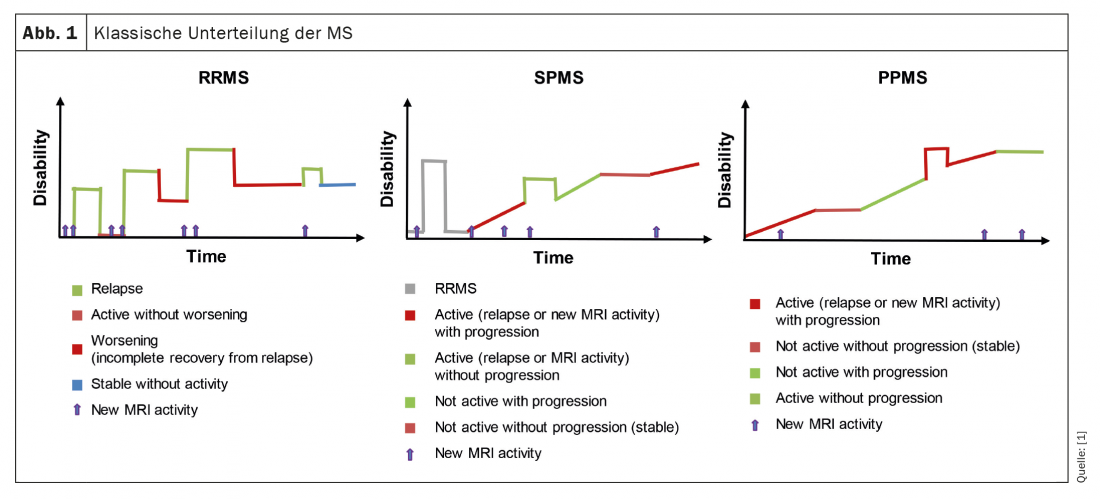
Multiple sclerosis (MS) is an autoimmune chronic inflammatory and degenerative disease of the central nervous system that affects more than 2.3 million people worldwide. It is characterized by both focal and diffuse damage. Physiopathologically, MS is due to circulating autoaggressive lymphocytes that penetrate the blood-brain barrier and attack the myelin layer of axons. This provokes demyelination and axonal damage, demonstrated Prof. Christina Granziera, MD, Basel. Traditionally, three manifestations of relapsing-remitting (RRMS), secondary progressive (SPMS) and primary progressive (PPMS) MS are distinguished ( Fig. 1). All are associated with different levels of inflammatory activity and clinical progression.
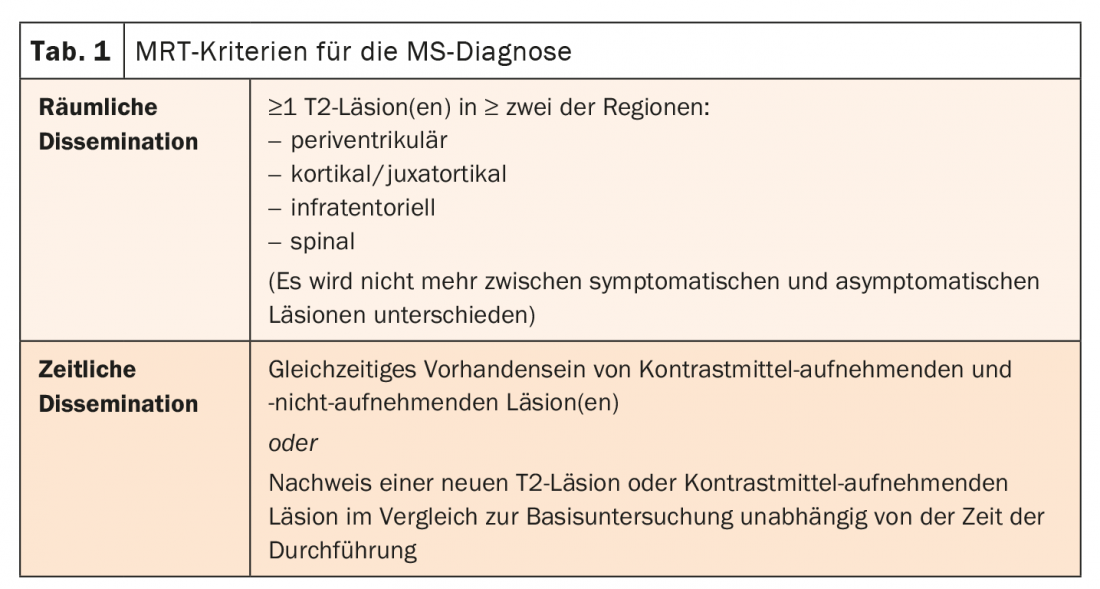
The diagnosis of relapsing-remitting MS is made on the basis of at least two clinically demonstrated relapses and at least two lesions. Lesions must be objectively demonstrated clinically. If only one relapse or lesion can be detected, additional requirements must be met with spatial and/or temporal dissemination (Tab. 1). PPMS is diagnosed when the patient has been in clinical disability progression without relapses for at least one year and at least two of the following factors are met:
- A T2 lesion on MRI and at least one periventricular, cortical/juxtacortical, or infratentorial lesion.
- at least two T2 lesions on spinal MRI
- intrathecal immunoglobulin synthesis
To date, there is no consensus for the diagnosis of SPMS. Different definitional options have been proposed. For example, the presence of continuous deterioration for at least one year, two consecutive sustained disabling events (independent of relapses), or steadily increasing neurologic dysfunction without clear improvement. According to the population-based MS-Base study, a clinical diagnosis of SPMS exists when at least three months of EDSS progression can be demonstrated in the absence of a relapse. In addition, the deterioration must amount to at least one EDSS level if the EDSS was below six before progression and 0.5 EDSS level if it was above six. Also, the EDSS after progression must be at least four with a pyramidal FS score greater than two.
Focus on differential diagnoses
When a patient presents with clinical deficits consistent with an MS relapse and the MRI scan demonstrates spatial dissemination, the following differential diagnoses should be considered:
- Infections/inflammations
- Neoplasia, NMOSD/MOGAD
- Cerebrovascular diseases
- Migraine
- Leukodystrophies, mitochondrial diseases
However, not only the characteristics of the lesions, but also their localizations can provide clues to possible other diseases. In recent years, several important radiological biomarkers have been developed to aid MS diagnosis. This includes, for example, the central vein. If at least 35% of CV lesions and two CVS lesions have a central vein, the presence of MS can be assumed with high specificity and sensitivity. Another biomarker are so-called paramagnetic rim lesions (PRL). It identifies activated, iron-containing cells and usually indicates chronic inflammatory lesions, the expert said. The differential diagnosis of other inflammatory demyelinating diseases of the CNS is particularly challenging. These include NMOSD, ADEM, MOG, or Baló disease, among others. In addition to clinical features, radiological and fluid biomarkers can also help distinguish MS from other diseases.
Effective therapy management
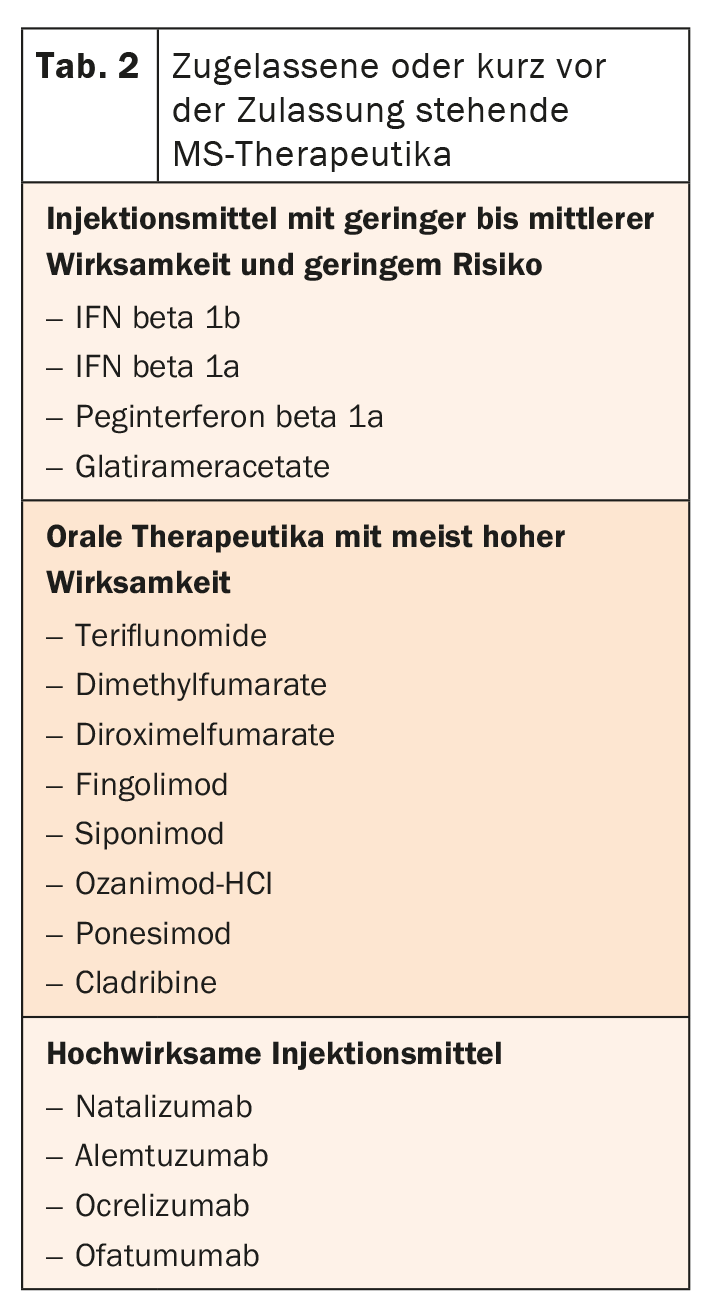
Most of the available MS therapies target B and T cells outside the CNS, but other options also act directly in the CNS (Table 2) . Most drugs are approved for RRMS. IFN beta 1a and siponimod can also be used for SPMS, and ocrelizumab can also be used for PPMS. Other preparations are currently undergoing clinical trials in this regard and have already demonstrated positive effects.
Congress: Forum for Continuing Medical Education
Source:
- Lublin FD, et al: Neurology. 2014; 83: 278-286; www.nationalmssociety.org/What-is-MS/Types-of-MS.
InFo NEUROLOGY & PSYCHIATRY 2021; 19(2): 24-26.