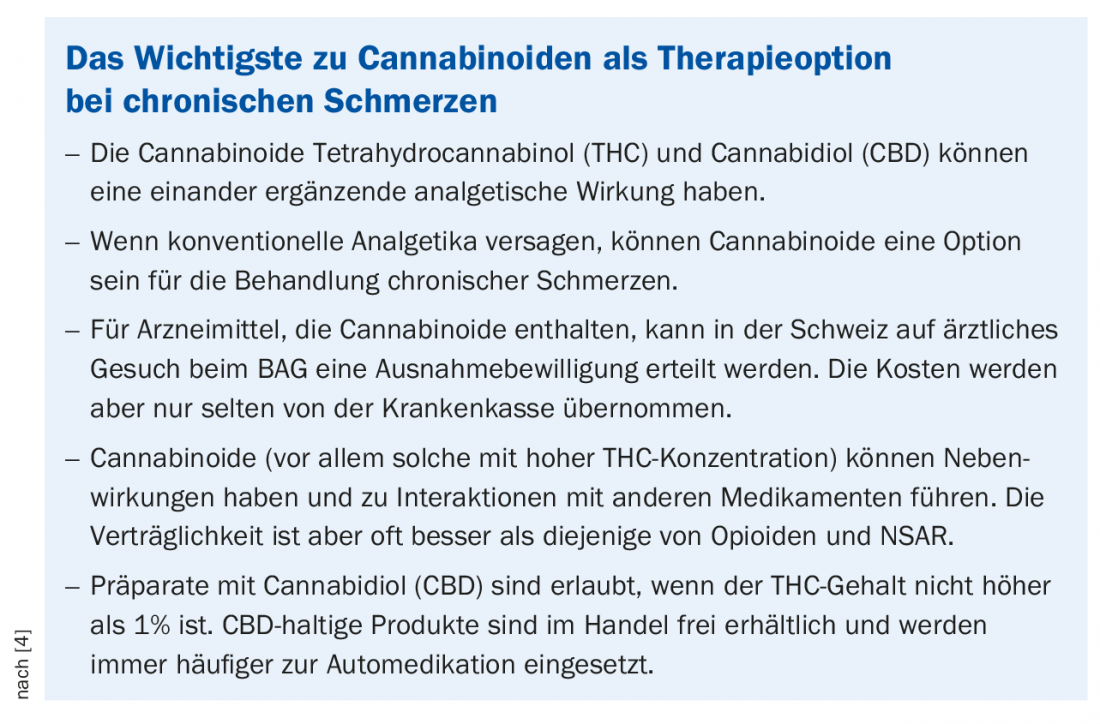
In individual cases, significant symptom-relieving efficacy of drugs containing cannabinoids was shown. Individual study results also support positive effects. However, the overall evidence base is not clear at the current time.
The use of cannabis for medical purposes is controversial. The conclusion of a meta-study published in 2015 and commissioned by the FOPH is that medical preparations containing cannabinoids have proven efficacy for the indication of chronic and neuropathic pain [1]. Statistically, however, the effect in this dataset is not very large – a finding that was replicated in 2017 [2]. On the other hand, there are reports of individual cases in which cannabis-containing drugs have significantly reduced subjective suffering, and the number of applications to the FOPH for exemptions is rising steadily.
Benefit-risk debate
In a meta-study published in 2018, statistical parameters were calculated for a benefit-risk balance regarding cannabis-containing drugs [3]. The number needed to treat (NNT) for at least 30% pain reduction was 24; in contrast, the number needed to treat until an adverse event occurs is only 6 [3]. According to PD Dr. med. Konrad Maurer, head of the interdisciplinary pain outpatient clinic at the University Hospital Zurich, this means an unbalanced relationship. On the other hand, it is also the case that the side effects of cannabis products (e.g., tachycardia, agitation) are relatively minor compared to those of other pain medications, and there is no risk of mortality even at high doses. With regard to undesirable effects of cannabis products, the debate on medical benefits should be distinguished from the socio-political discussion. The dependence potential of cannabis is lower than is generally assumed.
THC and CBD for medicinal purposes
Unlike THC (∆-9-tetrahydrocannabinol), CBD (cannabidiol) has no psychoactive effect. In Switzerland, the oral spray Sativex® (THC and CBD-containing muscle relaxant) is currently the only drug with cannabinoid active ingredients approved under the Therapeutic Products Act, but only as a second-line therapy for spasticity in the context of multiple sclerosis. Marinol®, a preparation containing THC in synthetic form (dronabinol), which is said to have analgesic and antispasmodic effects and to stimulate appetite, requires a medical application to the FOPH. Freely available in Switzerland are non-medical hemp products that have a TCH content of less than 1% or contain only the cannabinoid CBD. However, for medicinal products containing the active ingredient CBD for medical purposes, a medical application must be submitted to the FOPH and there is an obligation to report side effects to Swissmedics.
In the near future, the debate will increasingly revolve around CBD, Dr. Maurer said. Legalization of cannabis-containing products for medical purposes is planned in Switzerland, he said, but is not expected to take effect before 2022. Currently, costs for cannabis preparations are only covered by health insurance in individual cases. For self-payers, the price (about 400-800 CHF per month) can be a big hurdle, but compared to other medications that are covered by health insurance, it is a relatively small amount.
Source: VZI Symposium, January 31, 2019, Zurich
Literature:
- Whiting PF, et al: Cannabinoids for Medical Use. A Systematic Review and Meta-analysis. JAMA 2015; 313(24): 2456-2473.
- Meng H, et al: Selective Cannabinoids for Chronic Neuropathic Pain: A Systematic Review and Meta-analysis. Anaesth Analg 2017; 125(5): 1638-1652.
- Stockings E, et al: Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies. PAIN 2018; 159: 1932-1954.
- Baschoud A, Broers B: Cannabinoids and pain in the physician’s office. An option in the treatment of chronic pain? Prim Hosp Care Allg Inn Med 2018; 18(09): 156-159. DOI: https://doi.org/10.4414/phc-d.2018.01728
HAUSARZT PRAXIS 2019; 14(2): 36