Rhinosinusitis is a common health problem in primary care and is usually due to mucosal inflammation of the nose and sinuses. Less than 2% of cases are related to bacterial infections. Intranasal corticosteroids and saline are often indicated.
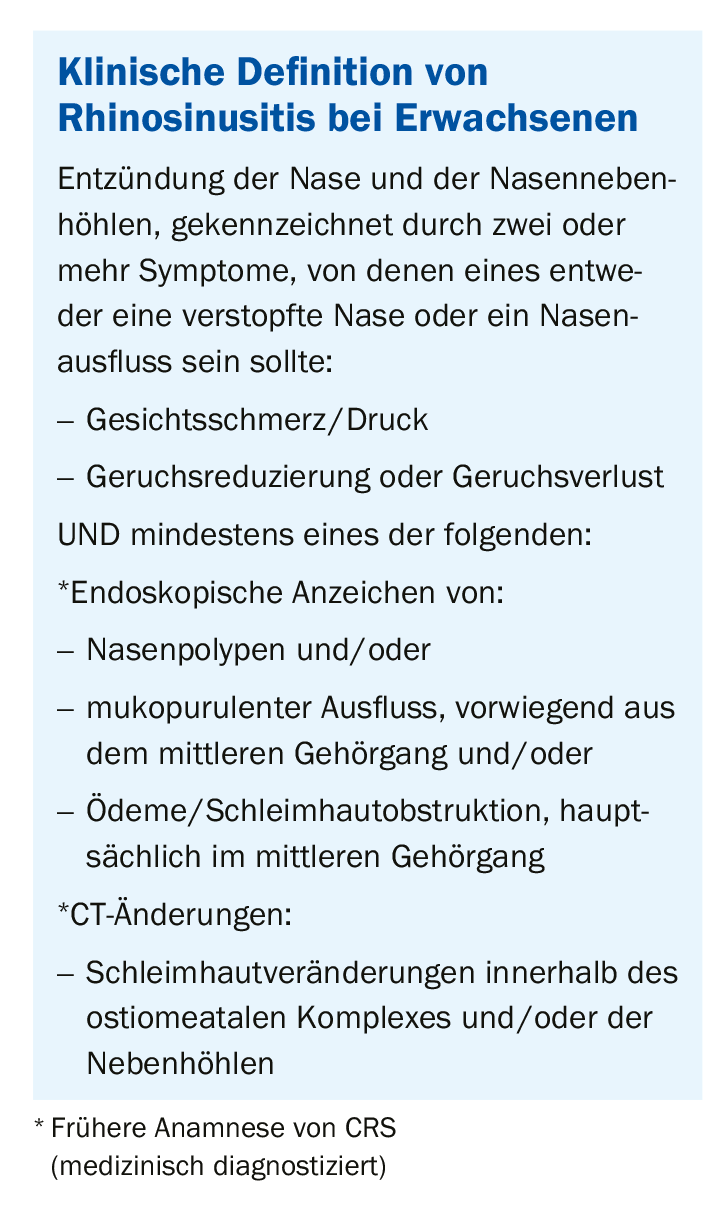
The diagnosis of RS is usually based on clinical symptoms supported by diagnostic imaging or nasal endoscopy.
Acute or chronic?
Acute rhinosinusitis (ARS) is defined as worsening of symptoms after five days or symptoms persisting after 10 days but less than 12 weeks. If the symptom duration is less than five days, it is acute viral rhinosinusitis, which is a cold. Chronic rhinosinusitis is defined by the duration of symptoms lasting longer than 12 weeks.
Viral or bacterial?
The majority of ARS cases are viral in origin, with only a few cases complicated by bacterial infection. In clinical practice, it is difficult to distinguish between bacterial and viral rhinosinusitis. This can lead to unnecessary use of antibiotics for patients and increase the incidence of antibiotic resistance. Symptoms such as fever, facial pain, purulent nasal discharge, and duration of symptoms were used to distinguish bacterial from viral rhinosinusitis.
Acute bacterial rhinosinusitis (ABRS) is present when at least three symptoms apply:
- discolored discharge (with unilateral predominance) and purulent secretion in the nasal cavity
- severe local pain (with unilateral dominance)
- Fever (>38° C)
- increased erythrocyte sedimentation rate/ C-reactive protein
- Worsening of symptoms and signs
Risk factors
Patients at increased risk for ARS are characterized by the following features:
- active smoker
- allergic rhinitis (AR)
For CRS, these are the following risk factors:
- Smoker
- positive family history
- Asthma, especially in the presence of CRS with nasal polyps.
- Allergies, chronic bronchitis and emphysema
- ARS
- chronic rhinitis
- gastroesophageal reflux disease
- Sleep apnea
- Adenotonsillitis
Clinic
Anterior rhinoscopy should be performed as part of the clinical evaluation of suspected ARS in a primary care setting. Findings such as mucosal edema, nasal inflammation, purulent nasal discharge, polyps, and/or anatomic abnormalities may be present. Anterior rhinoscopy has limited value in the diagnosis of CRS. Diagnosis of CRS requires nasal endoscopy by an otolaryngology (ORL) surgeon, which allows better visualization of nasal pathology including anatomic variations, mucosal inflammation, polyps, and nasal discharge.
Laboratory
An endoscopically directed culture by otolaryngologists can obtain a sample for culture and susceptibility testing in unresolved ABRS (no response to antibiotics after 72 hours).
The organisms most commonly associated with ABRS are:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis (more common in children)
- Anaerobic organisms are predominant in ARS of dental origin.
In CRS, the organisms most commonly involved are:
- Staphylococcus aureus
- Enterobacteriaceae spp
- Pseudomonas spp
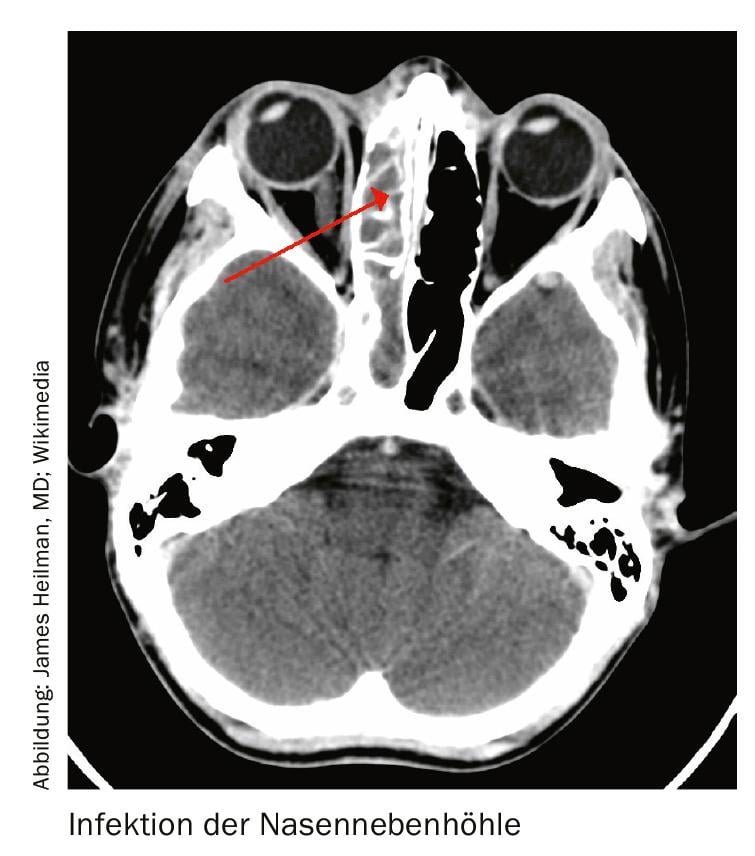
Radiology
Simple radiography is not recommended. Computed tomography (CT) is the gold standard for radiologic evaluation of the paranasal sinuses. A CT scan of the paranasal sinuses should be considered in the ORL setting if:
- the medical therapy is not effective
- an operation is planned
- Complications are suspected
Therapy: ARS
Nasal lavage: Nasal lavage is recommended for ARS. Saline facilitates the mechanical removal of mucus, infectious agents and inflammatory mediators. It also reduces crust formation in the nasal cavity and increases mucosal clearance.
Corticosteroids: Intranasal corticosteroids should be considered for a period of 14 to 21 days in ARS. Oral corticosteroids should not be prescribed for the treatment of ARS in primary care.
Oral antihistamine: an antihistamine may have a role in the treatment of ARS with underlying AR. Symptoms suggestive of the disease include sneezing, nasal itching, nasal congestion, and rhinorrhea. The antihistamine fights sinusitis symptoms. There is evidence that sneezing improves after 14 days and nasal congestion improves after 28 days of treatment.
Antibiotics: Antibiotics may be prescribed for ABRS after weighing the benefits against possible side effects. Gastrointestinal disturbances are the most common side effects. Overuse of antibiotics has directly led to an increased prevalence of antibiotic resistance.
If ABRS is suspected, the antibiotics of choice are:
- Amoxicillin 500 mg every 8 hours for 5-7 days
OR - Amoxicillin/clavulanate 625 mg every 8 hours for 5-7 days.
Other medications:
Analgesics: Paracetamol or nonsteroidal anti-inflammatory drugs can provide symptomatic relief for viral and bacterial upper respiratory tract infections in RS.
Decongestants: topical or systemic decongestants may provide additional symptomatic relief. Because of the rebound phenomenon, topical decongestants should not be prescribed for more than two weeks. Oral decongestants should be prescribed with caution in conditions such as insomnia, glaucoma, benign prostatic hyperplasia, diabetes mellitus, and cardiovascular disease.
Mucolytics and antiviral agents
Therapy: CRS
Intranasal corticosteroids should be administered for 16-52 weeks at . Short-term oral corticosteroids (25 mg/day for 2 weeks) should be given only in exceptional cases. Nasal irrigation may provide relief.
Antihistamine: there is insufficient evidence to recommend its use for the treatment of CRS in non-AR patients. Antibiotics should not be used routinely in CRS.
Surgery: surgery should be considered for ARS with orbital or intracranial complications. Patients with CRS who do not receive optimal medical treatment should be offered functional endoscopic sinus surgery.
Bank transfer
ARS: Criteria for premature referral (within one week) are persistence of symptoms despite optimal therapy. Immunocompromised patients such as those with uncontrolled diabetes, end-stage renal failure, or human immunodeficiency virus (HIV) infection should also be referred. Other criteria include frequent recurrence (> 4 episodes per year), anatomic defects causing obstruction, and suspected malignancy. Urgent referral criteria (within 24 hours) include periorbital edema/erythema, double vision, ophthalmoplegia/restricted eye movement, decreased visual acuity, severe frontal/retroorbital headache, forehead swelling (subperiosteal abscess), and neurologic manifestations such as meningitis, altered consciousness or seizures, and septicemia.
CRS: Criteria for early referral (within one week) include failed course of therapy, >3 sinus infections/year, suspected fungal infection, and granulomatous disease or malignancy. Urgent referral criteria (within 24 hours) include severe sinus pain or swelling, especially in immunocompromised patients with uncontrolled diabetes, end-stage renal failure, or HIV infection.
HAUSARZT PRAXIS 2019; 14(9): 23-24