At the Update Refresher General Internal Medicine at Technopark Zurich, one of the main topics was rheumatology. Here it was osteoporosis in particular that was discussed in depth. In any case, to plan the therapeutic strategy, one should go beyond DXA, as it is the most important tool for calculating fracture risk, but not the only one. Among osteoporosis drugs, bone resorption-inhibiting substances continue to be in the majority, yet an active substance with bone formation-stimulating mechanisms has also been on the market for several years. It can be a very effective option in individual cases.
One thing is certain: fractures increase the older you get, says Stefan Bützberger, MD, Schinznach-Bad, by way of introduction. Hospitalizations due to osteoporosis are common and, according to surveys, occur in significantly more cases than for other chronic diseases such as COPD or heart failure. “Due to age-related bone remodeling, we all lose bone mass (peak bone mass) starting around age 35. This loss is particularly rapid in women during menopause, yet osteoporosis also occurs in men and should not be overlooked there,” the speaker warned. About half of all 50-year-old women suffer a fracture caused by osteoporosis. A considerable proportion of these fractures are associated with increased mortality and the threat of long-term dependency on nursing care.
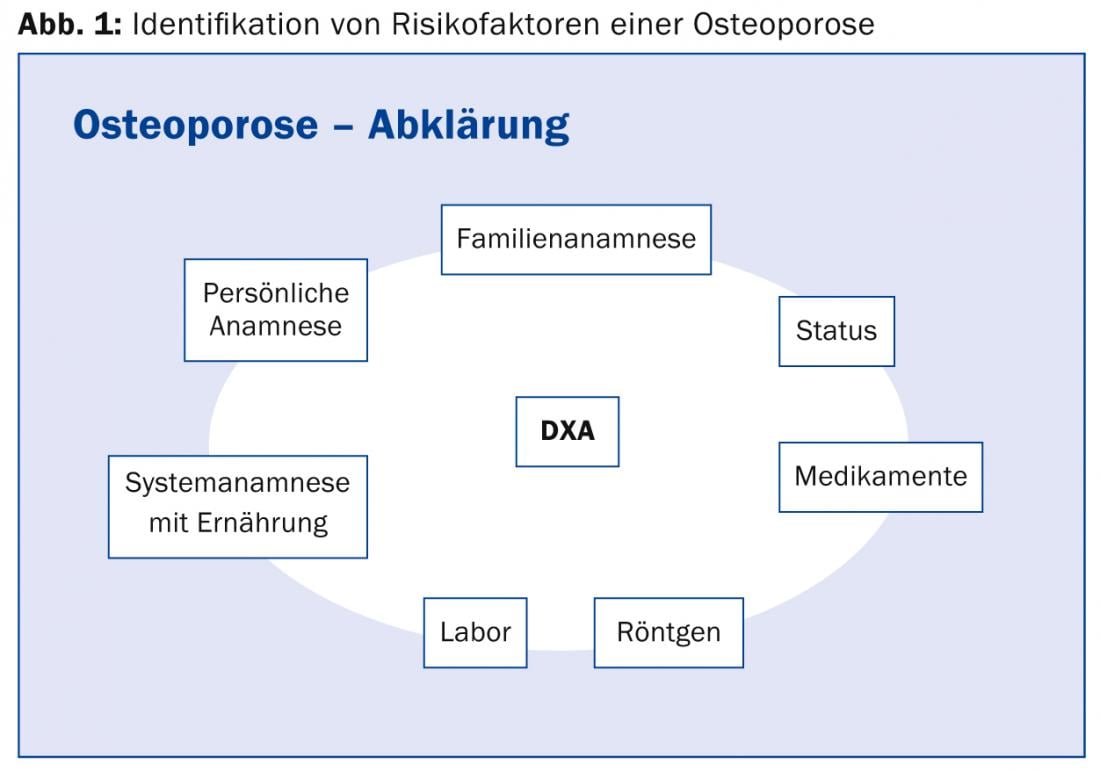
It should be noted that many fractures occur at a T-score that is still above the threshold of -2.5. Thus, although “dual-energy x-ray absorptiometry”, or DXA, is the most important basis for diagnosing osteoporosis and the best-studied tool for estimating fracture risk, it is not the only one. “If you only go by the T-score, you overtreat certain young patients and withhold necessary therapy from others, such as postmenopausal women, who often show fractures with T-scores of -1 or -1.5. The DXA is only half the truth: a measured osteopenia can equally be an osteoporosis and, depending on the case, must be treated accordingly. Today, it is the fracture risk that determines the therapy strategy,” explained Dr. Bützberger. The main assessment components for identifying risk factors of osteoporosis are shown in Figure 1. Various electronic tools are available for calculating fracture risk (e.g. FRAX® calculator from WHO). This shows that sometimes even with significant osteoporosis and a high T-score (for example, of -3), the 10-year fracture risk can be low and therefore no antiresorptive therapy is needed.
Secondary causes
“If there are indications of a secondary cause in the history or clinic, do the minimum program of laboratory tests. In men, don’t forget testosterone, sometimes values are found in the basement and the affected patient then benefits in several respects from testosterone substitution,” explained Dr. Bützberger. “Very central to bones, of course, are vitamin D and calcium. Vitamin D deficiency not only causes serum parathyroid hormone (PTH) levels to rise, leading to bone resorption, but also increases the risk of falls and fractures.” Vitamin D is also essential for calcium absorption from the intestine. The fact that undersupply is widespread, especially in our latitudes, is mainly due to the fact that required vitamin D levels (25[OH]D serum concentration, >80 nmol/l) can be poorly achieved through sun exposure or diet (in contrast to the necessary calcium requirement of 800-1200 mg). To reach the target value of >80 nmol/l, at least 1000 (international 800) E/day is needed – i.e. 10 ViDe3 drops daily.
“If diet alone is not sufficient as a source, one tablet per day (e.g. Calperos®) is usually sufficient for optimal calcium intake. I also use combination preparations of calcium and vitamin D (e.g. Kalcipos®-D3 500/800) relatively frequently; they should be taken with or after food and not fasting,” says the expert. Just as important as continuous therapy with calcium and vitamin D are an adequate calorie supply, sufficient protein (approx. 1 g/kgKG/d), active exercise (strength training, especially axial load, maintenance of good musculature), smoking cessation, moderate alcohol consumption, and fall prevention.
Osteoporosis drugs
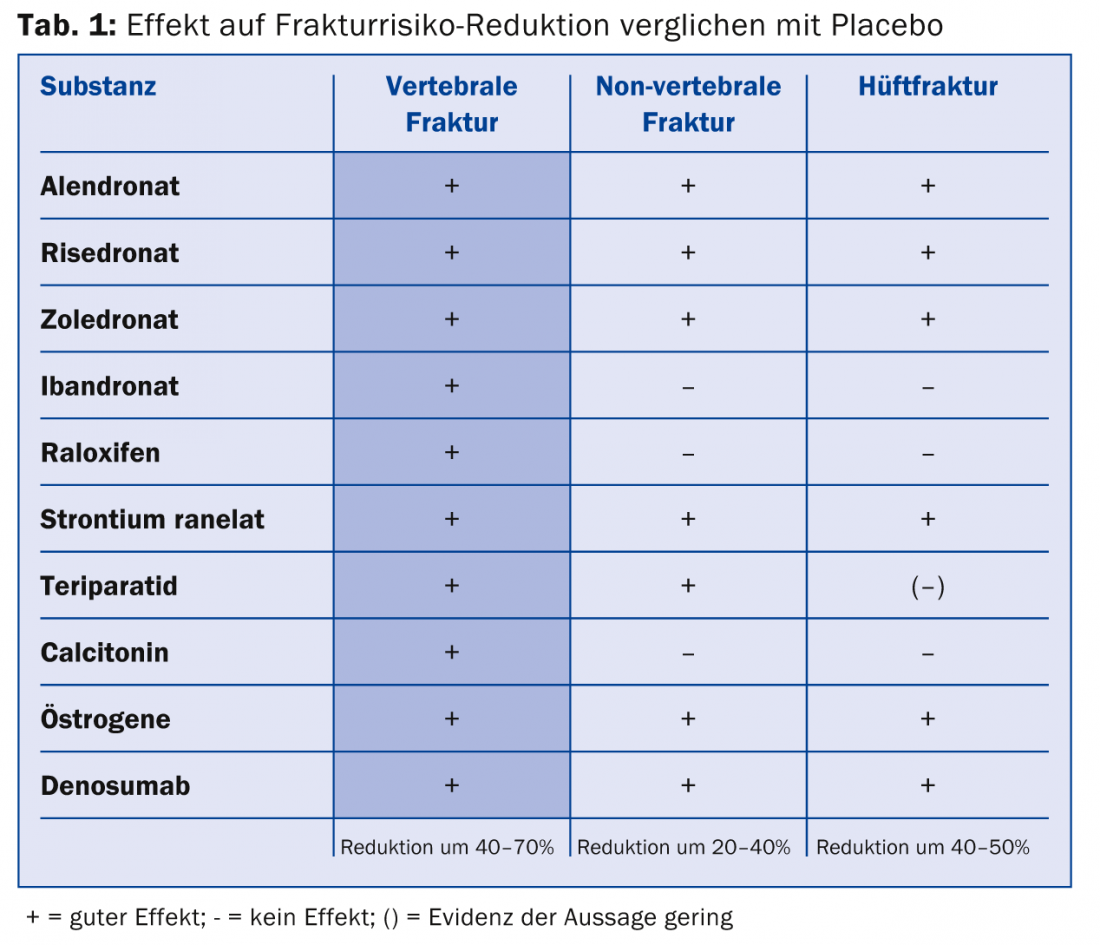
Two basic principles can be distinguished: Bone resorption-inhibiting agents (e.g. bisphosphonates, denosumab) and bone regeneration-stimulating agents (e.g. teriparatide). A summary of pharmacotherapy for osteoporosis is shown in Table 1. Bisphosponates lead to loss of resorptive function and may induce apoptosis. Bone markers remain suppressed. Therefore, bisphosphonates should only be used for a limited period of time: A five-year therapy duration brings a clear benefit with a reduced fracture incidence. Benefits of prolonged treatment are not assured; rather, increasing side effects can be expected in this case. Nevertheless, the incidence of e.g. atypical fractures remains very low (3-50/100,000 person-years). According to the speaker, individuals at high risk of fracture continue to benefit beyond five years.
Denosumab blocks RANKL and thus directly blocks osteoclast formation, function and survival. It is administered subcutaneously every six months. “The interesting thing about the substance is that, unlike the bisphosphonates, it only fully suppresses for four months. After that, the markers recover somewhat, until then the next injection follows after six months. It could be that this pattern allows longer use than we know from the bisphosphonates,” says Dr. Bützberger.
An alternative to antiresorptive therapy is teriparatide (Forsteo®), which can be a very effective option if the indication is right. Collaboration with the rheumatologist/endocrinologist is critical. Currently, it is the only drug with an osteoanabolic principle. The handling is simple (once a day subcutaneously). The maximum duration of therapy is 24 months, after which the bone structure, i.e. what has been gained, should be urgently preserved, otherwise the patient will lose everything again: Follow-up therapy is essential.
Source: Update Refresher General Internal Medicine, November 19, 2014, Zurich
HAUSARZT PRAXIS 2015; 10(2): 31-32