Dysphagia is a disorder of the swallowing act that may affect one or more phases of the swallowing process. A number of conditions can lead to dysphagia, and esophageal hernias are one possible cause. The medical workup is multidisciplinary and usually includes imaging and endoscopic diagnostics.
The term dysphagia describes any type of swallowing disorder that may affect one or more phases of the swallowing process [1,8]. Dysphagia is the painless form of impaired swallowing. Odynophagia describes the painful disturbance of the swallowing process and aphagia the completely reduced ability to swallow. If the lumen of the esophagus is narrowed below 13 mm, the passage of solid food is restricted. Fluid passage is reduced for stenosis less than 5 mm.
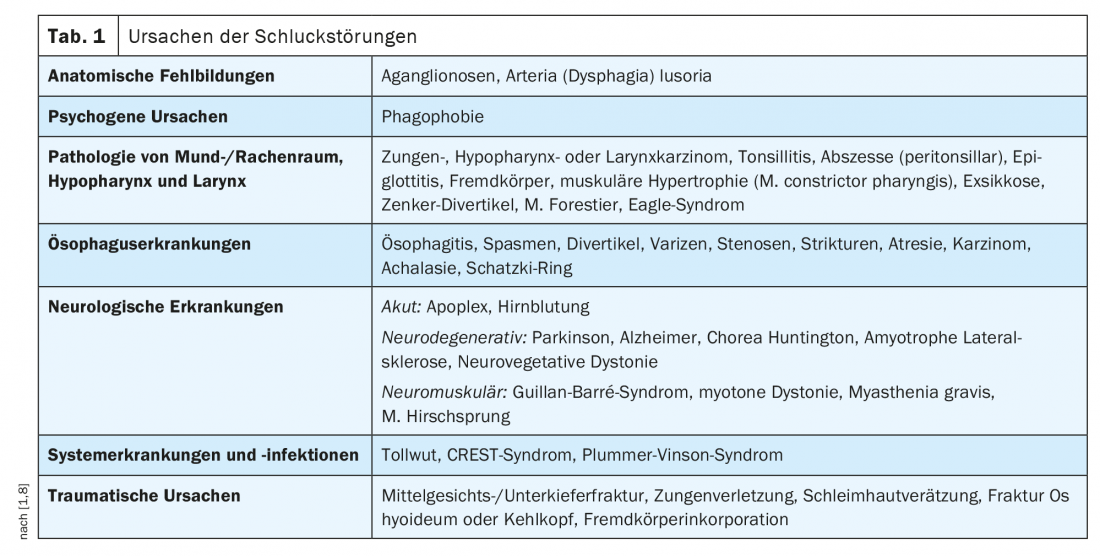
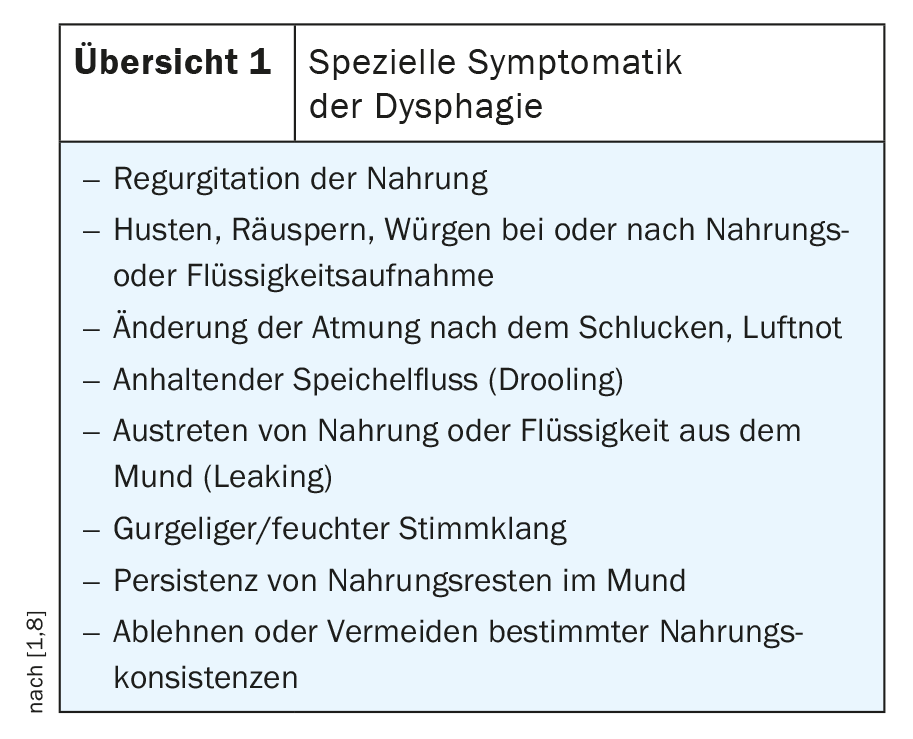
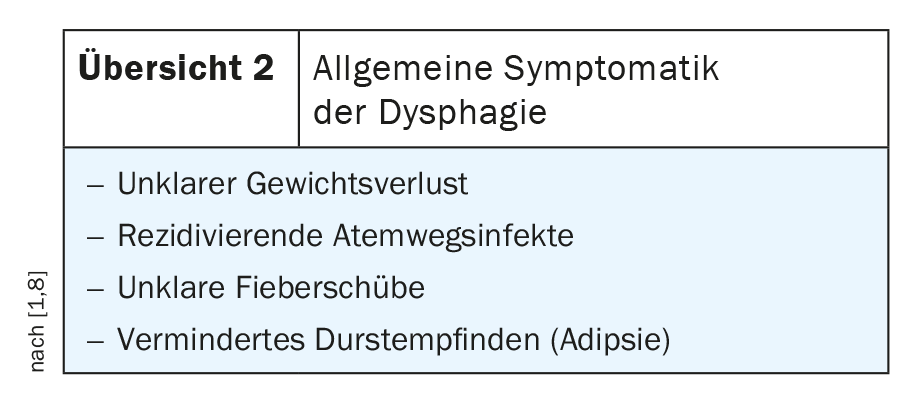
A variety of possible causes of dysphagia are listed in Table 1 . The symptoms are also varied and diverse, as shown in the overview at 1 and 2 .
Due to age, the risk of swallowing disorders increases. Tissue weaknesses, drug side effects, and postural changes can be relatively innocuous causes with great impact [2]. In Germany, between 80,000 and 160,000 patient-doctor contacts are documented each year for new-onset dysphagia, affecting one in six people over the age of 65. Due to diet and lack of exercise, the number of obese patients is increasing, and with it gastroesophageal reflux. Increasing allergic dispositions may also cause eosinophilic esophagitis [7].
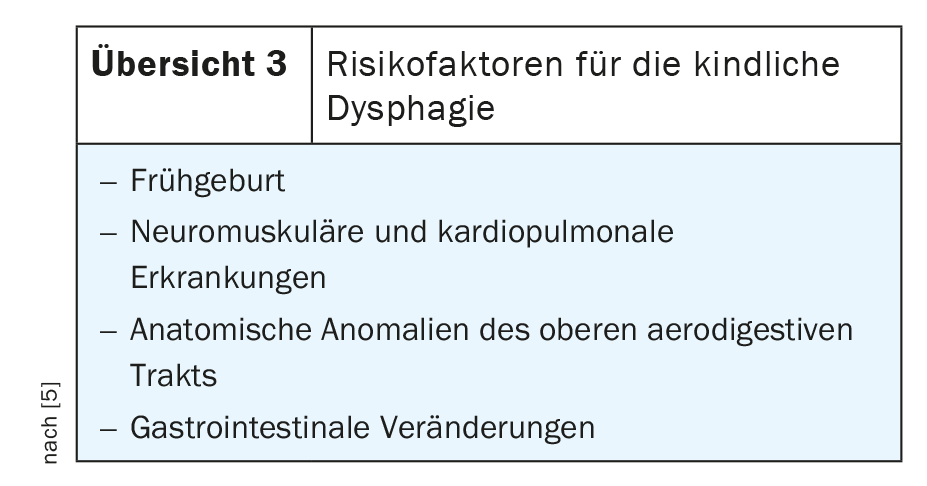
However, there has also been an increase in the pediatric patient population with dysphagia [4]. Overview 3 lists the possible risk factors for infantile dysphagia. In addition to the causes listed in the table, strumen can also lead to impaired passage, esophageal hernia or cervical spine dysstatics to myogelosis and consecutive feelings of pressure and lumpiness.
This article focuses on esophageal hernias as a possible cause of dysphagia. Superficially, a muscular weakness of the diaphragm in the region of the hiatus is considered to be a favoring factor in the development of hiatal hernias, as well as an intra-abdominal pressure increase. In principle, the clarification of dysphagia requires multidisciplinary screening including adequate imaging or endoscopic diagnosis given the broad spectrum of causes. The Makuuchi classification [6] distinguishes 4 types of hiatal hernias, with type I corresponding to esophagoaxial hernia and types II to IV corresponding to the paraesophageal hiatal hernia variants. However, these account for only about 5% of all hiatal hernias [5]. Hiatal hernia is defined as transdiaphragmatic protrusion/migration of gastric portion to intrathoracic [9]. The extreme case is the thoracic stomach with complete dislocation of the stomach into the mediastinum. The indication for surgical therapy is given for stages II to IV.
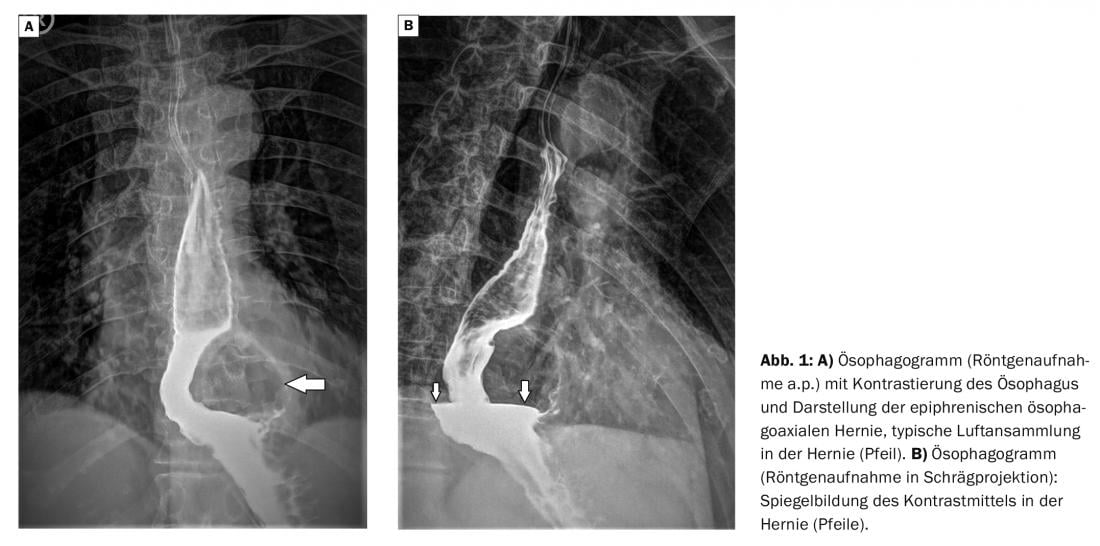
Radiographs can visualize functional or mechanical dysfunction of the swallowing cycle and changes in the esophagus with oral contrast of the esophagus with static images, and even better with fluoroscopy and cinematographic documentation of the swallowing cycle [2].
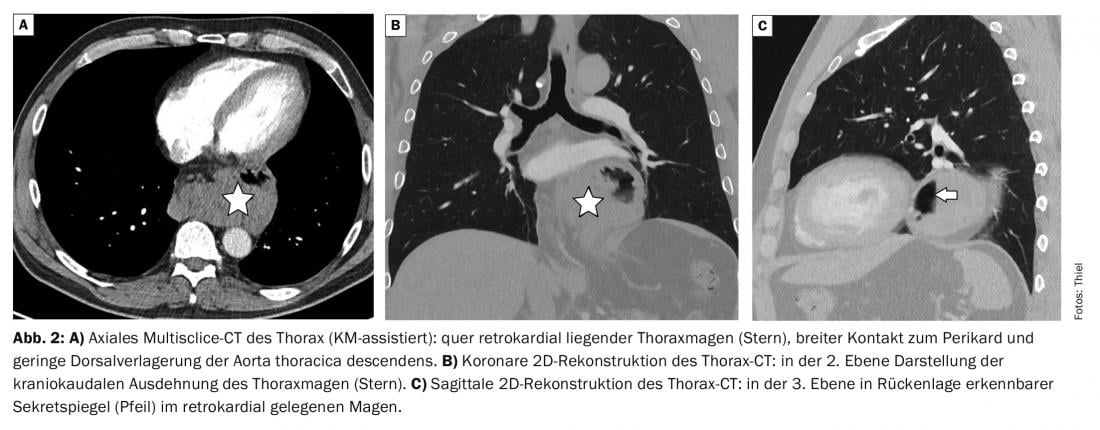
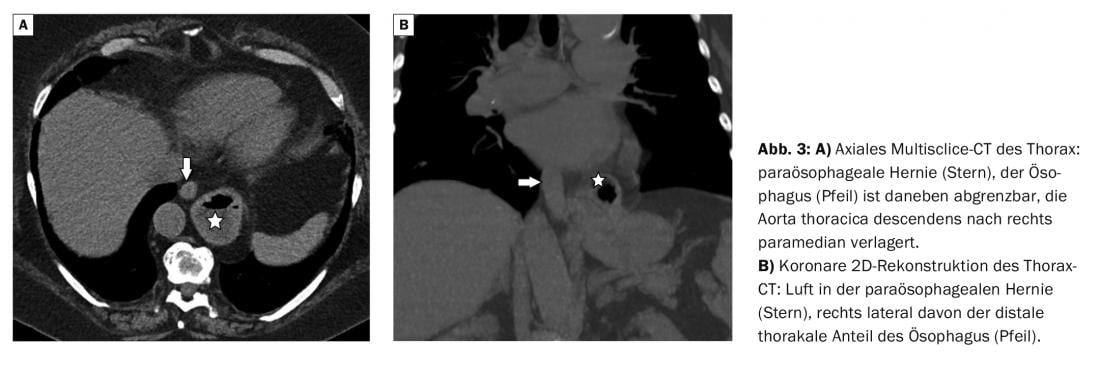
Computed tomographic examinations reliably differentiate between esophagoaxial and paraesophageal hernia. Even with multiplanar reconstruction, the modern multisclice scanners allow coronal and sagittal plane or any freely selectable oblique reconstruction in addition to the primarily axial generated images. Intravenous contrast agent administration is not required for this diagnostic issue.
With its high soft tissue contrast and primary multiplanar imaging of pathological processes, magnetic resonance imaging has diagnostic advantages for the clarification of inflammatory or tumorous changes, but also disadvantages compared with CT in the assessment of pulmonary structures.
Case studies
In case report 1 , a 68-year-old female patient was radiographically verified to have a gastroscopically diagnosed axial sliding hernia of the esophagus. The woman complained of long-lasting nonspecific upper abdominal discomfort, occasional dysphagia, and heartburn. Esophagography confirmed the epiphrenic hernia to be approximately 5 cm in extent (Fig. 1A and B).
Case report 2 demonstrates a thoracic stomach on computed tomographic examination of a 55-year-old man with dysphagia, epigastric discomfort, and regurgitation. Only a small portion of the stomach was found subphrenically (Fig. 2A to C).
In case report 3 (Fig. 3A and B) , a 52-year-old man was diagnosed with paraesophageal gastric hernia on CT who also complained of epigastric discomfort and occasional dysphagia.
Take-Home Messages
- Dysphagia should be considered a symptom, not a diagnosis.
- There are many causes, which require close cooperation of general practitioner, internist, neurologist, radiologist and surgeon in the clarification and also therapy.
- In addition to endoscopy, imaging techniques such as X-ray kinematography, CT or MRI are helpful tools in the differential diagnosis of dysphagia.
- Dysphagia is not a change limited to a certain age, however, the normal aging processes can negatively affect its course.
- Hiatal hernia as a possible cause of dysphagia is differentiated into esophagoaxial and paraesophageal hernia and worthy of surgery from stage II according to Makuuchi.
- In extreme cases, the entire stomach may luxate intrathoracically.
Literature:
- Dysphagia. https://flexikon.doccheck.com/de/Dysphagie (last accessed Feb. 15, 2022).
- Khan A, Carmora R, Traube M: Dysphagia in the elderly. Clin Geriatr Med 2014; 30(1): 43-53.
- Lancaster J: Dysphagia: its nature, assessment and management. Br J Community Nurs 2015; Suppl Nutrition: S28-32.
- Lawlor CM, Choi S: Diagnosis and Management of Pediatric Dysphagia. Review. JAMA Otolaryngol Head Neck Surg 2020; 146(2): 183-191.
- Mori T, Nagao G, Sugiyama M: Paraesophageal hernia repair. Ann Thorac Cardiovasc Surg 2012; 18(4): 297-305.
- Nishizawa T, Suzuki H: Hiatal hernia. Nihon Rinsho 2016; 74(8): 1339-1342.
- Philpott H, Garg M, Tomic D, Balasubramanian S, Sweis R: Dysphagia: thinking outside the box. World J Gastroenterol 2017; 23(38): 6942-6951.
- Tiefenböck F: Dysphagia, www.netdoktor.de/symptome/dysphagie (last accessed Feb. 15, 2022).
- Weyhe D, Uslar V, Kühne J, Kluge A: Hiatus hernia: Standards and controversies in diagnostics and treatment. Surgeon 2019; 90(4): 331-348.
HAUSARZT PRAXIS 2022; 17(3): 21-23











