Zenker’s diverticulum causes passenger disturbances in the pharyngoesophageal junction. Regurgitation and regurgitation of undigested food occur frequently. As the Zenker’s diverticulum grows larger, there is a globus sensation in the throat. Radiologic evaluation may include procedures with contrast of the esophagus, as well as computed tomography or magnetic resonance imaging studies.
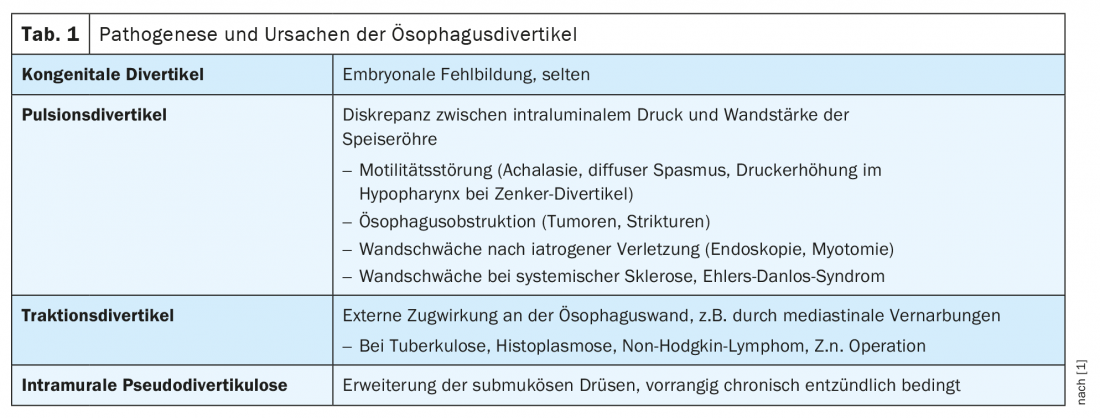
Dysphagia can have a wide range of possible causes. Achalasia and hiatal hernia have been discussed in previous publications. Diverticula of the esophagus, depending on their location and size, can also lead to obstruction of the swallowing process. Table 1 lists the pathogenesis and causes of esophageal diverticula [1].
The most common diverticulum of the esophagus is Zenker’s diverticulum. Despite its location in the pharynx, this diverticulum is usually assigned to the esophagus in the literature [4,5]. The first description was made by Ludlow already in 1769. In 1877, the Erlangen pathologist Friedrich von Zenker analyzed and described the association of the existence of this diverticulum with an increase in intrapharyngeal pressure. The incidence is 2:100,000/year, and the age of manifestation is usually 70 to 80 years. Men are more frequently affected than women [2]. Typical localization is a preexistent weak point of the dorsal wall of the pharynx between the cricopharyngeal and inferior constrictor pharyngis muscles, the Kilian triangle. Due to pressure, there may be an outpouching of the posterior pharyngeal wall with formation of a diverticulum, favored by increased tone of the cricopharyngeal muscle and impaired relaxation of the upper esophageal sphincter [3].
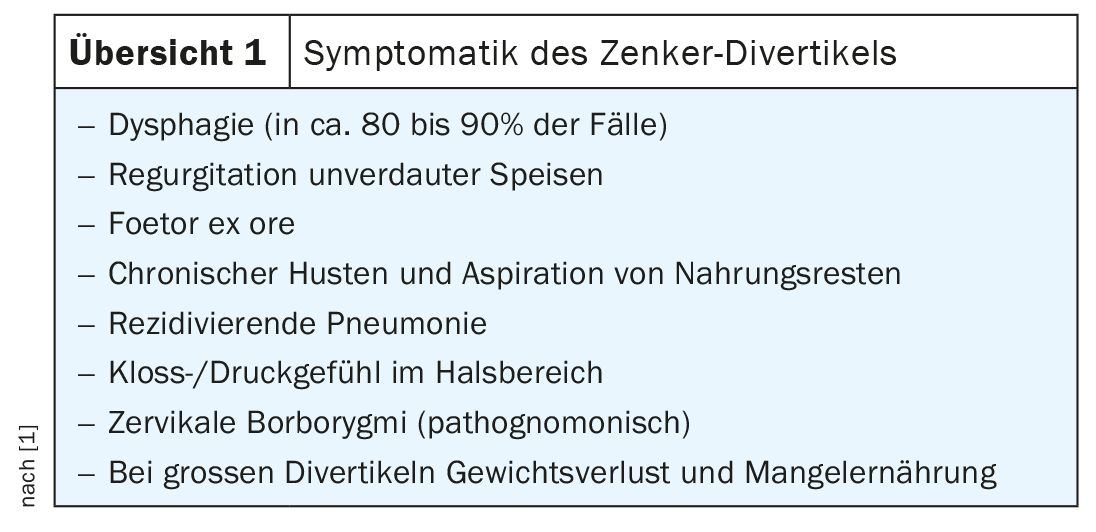
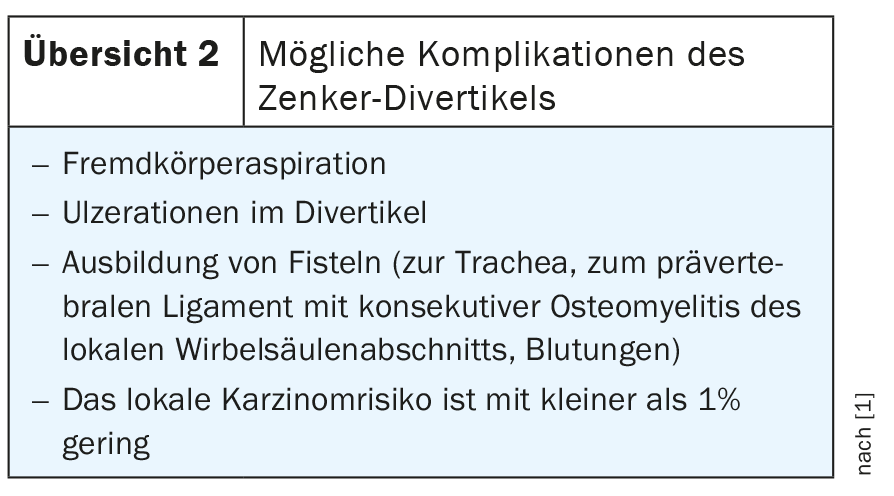
The tentative diagnosis of Zenker’s diverticulum results from symptoms summarized in Overview 1. The degree of expression is done by the Brombart classification. Potential complications of Zenker’s diverticulum are described in Overview 2.
Endoscopic clarification may have the risk of via falsa. If the endoscope is advanced into the diverticular sac rather than the esophageal lumen, there is a significant risk of perforation. Depending on the extent of the symptoms, there is an indication for surgical therapy with open (first described in 1936 by Aubin) or endoscopic procedures. In this regard, open surgical treatment was found to have a very good long-term outcome with a 94% success rate and a recurrence rate of 7.5%, although it also had a mortality rate of 3.4%.
Diverticula of the middle esophagus and those with epiphrenic location are much less common. X-ray examinations are very effective in detecting Zenker’s diverticulum. The “porridge swallow”, the images with contrast of the upper digestive tract with barium sulfate, can visualize the diverticulum very well. It is important to take images in several planes, especially also in oblique projection, to visualize the diverticulum.
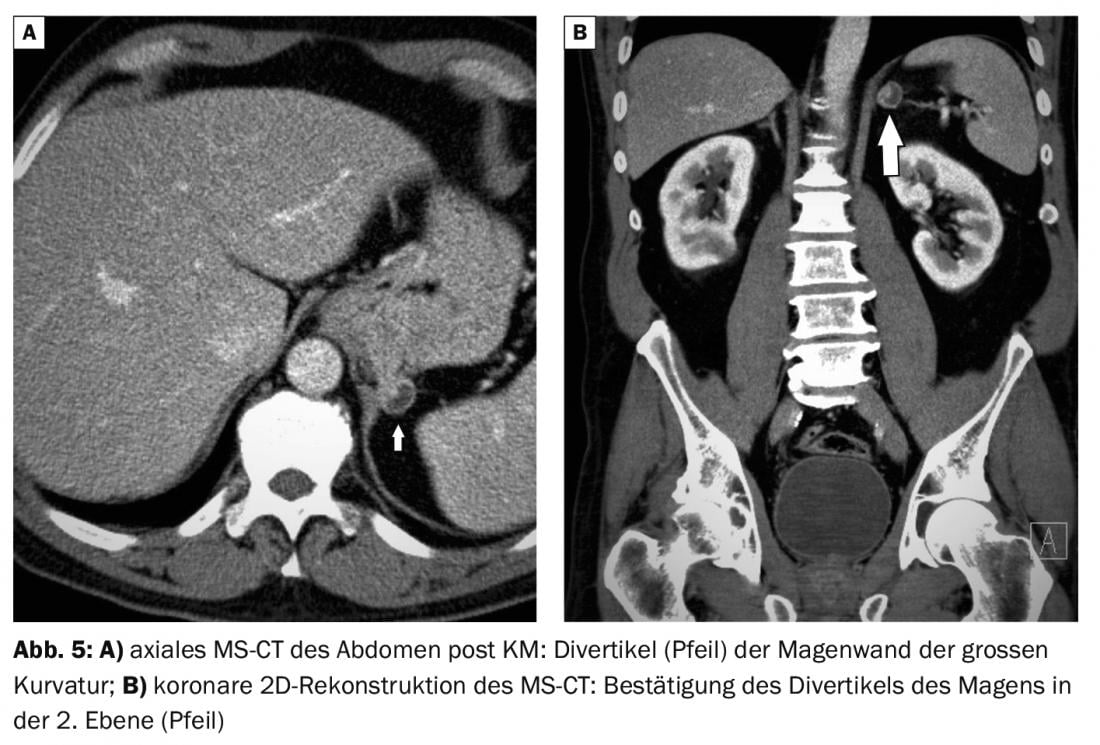
Computed tomography, similar to MRI of the pharyngeal wall, can delineate adjacent fluid-containing and also air-containing structures. Contrasting the pharynx and esophagus with swallowing iodine-containing radiographic contrast medium (barium sulfate often causes artifacts on CT) can achieve improved visualization of diverticula with KM retention.
Magnetic resonance imaging is not used for primary diagnosis of Zenker’s diverticulum. Detection may be considered incidental if cystic lesions with fluid levels are demarcable in the posterior visceral space just caudal to the pharyngoesophageal junction [6]. If local complications are suspected, then the diagnostic method is very good at detecting inflammatory processes due to the high soft tissue contrast.
Case studies

In case report 1, a 4.5-cm-diameter symptomatic diverticulum is evident at the level of the larynx (Fig. 1A and B), still without compression of the esophagus. Endoscopically, a salivary lake in the right piriform recess was conspicuous in the 80-year-old patient with dysphagia.
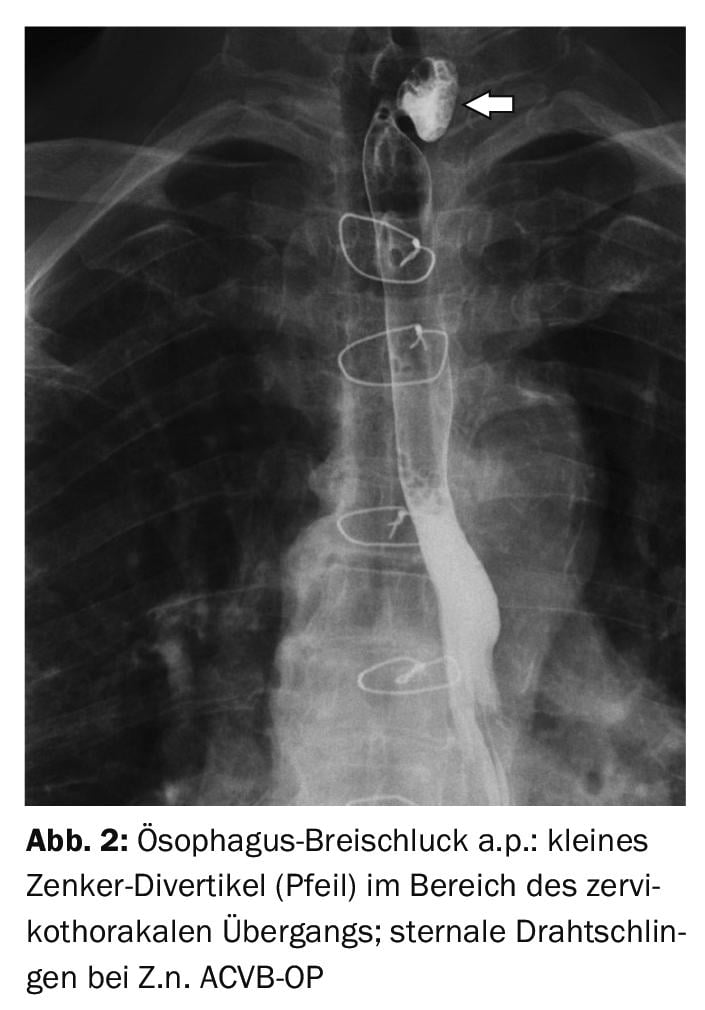
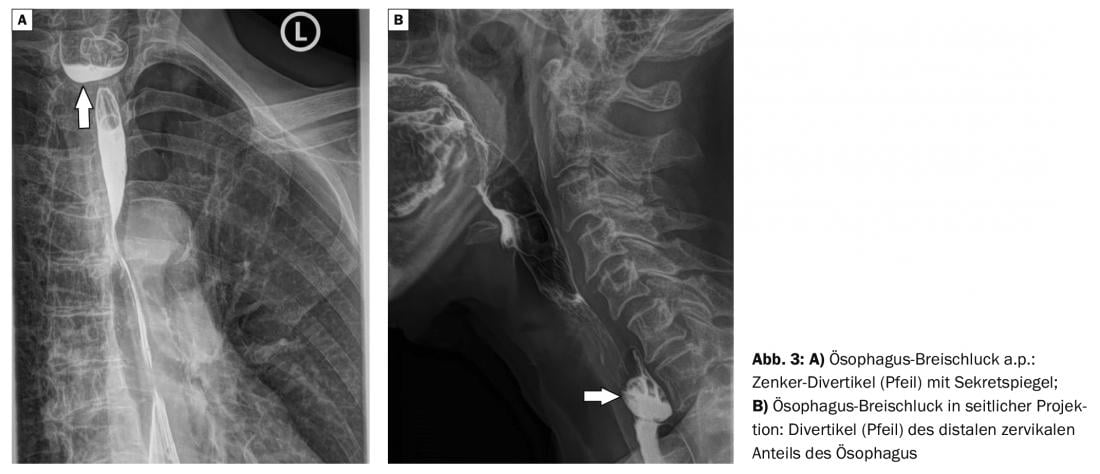
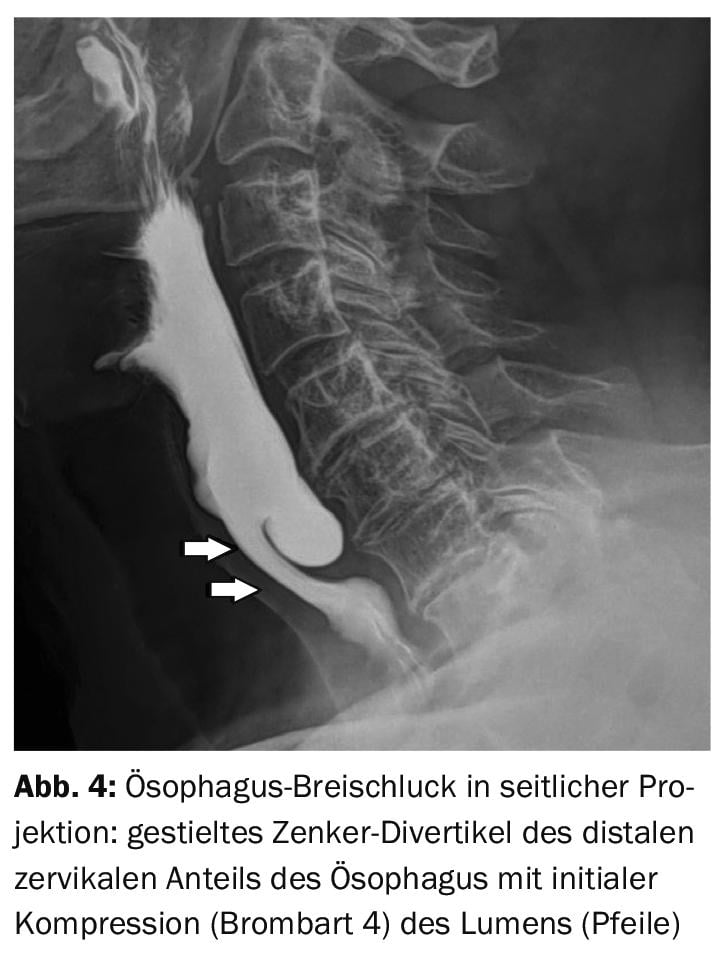
Case report 2 shows a 70-year-old patient with an approximately 2-cm-diameter Zenker’s diverticulum (Fig. 2) without evidence of functional impairment. In Z.n. ACVB-OP with recognizable sternal wire loops there was symptomatology with globus sensation and irritable cough. Dysphagia was leading clinical symptom in a 59-year-old female patient (case study 3) with an approx. 3.5 cm diameter Zenker’s diverticulum leading to initial compression of the proximal esophagus (Fig. 3A and B). A Zenker diverticulum grade 4 according to Brombart is present in the Case example 4 presented, there was significant dysphagia in the patient. (Fig. 4). Diverticula may also be detectable in other sections of the digestive tract, as demonstrated by the incidental finding of the large gastric curvature in a 59-year-old patient (Fig. 5A and B).
Take-Home Messages
- The most common diverticulum of the esophagus is Zenker’s diverticulum.
- Depending on the location and size, obstruction of the swallowing process may result.
- Typical localization of Zenker’s diverticulum is a preexistent weakness of the dorsal wall of the pharynx between the M. cricopharyngeus and M. constrictor pharyngis inferior.
- The classification of Zenker diverticula is according to Brombart with grade 1 to 4.
- Zenker’s diverticulum can lead to extensive clinical symptoms.
- Diagnostic imaging may be performed by X-ray examination with contrast of the esophagus, computed tomography or magnetic resonance imaging.
Literature:
- Bechtler M, Jakobs R: Esophageal diverticulum. Gastroenterology up2date 8, 2012. http://dx.doi.org/10.1055/s-0032-1310101.
- Ferreira LE, Simmons DT, Baron TH: Zenker’s diverticulum: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus 2008; 21: 1-8.
- Fulp SR, Castell DO: Manometric aspects of Zenker’s diverticulum. Hepatogastroenterology 1992; 39: 123.
- Zenker Diverticulum, https://flexikon.doccheck.com/de/Zenker-Divertikel, (last accessed Apr. 19, 2022).
- Vogelsang A, Schumacher B, Neuhaus H: Treatment of Zenker’s diverticulum. Dtsch Arztebl Int 2008; 105(7): 120-126.
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Differential diagnosis in MRI. Georg Thieme Verlag Stuttgart, New York, 2002: 258.
HAUSARZT PRAXIS 2022; 17(5): 20-22











