The psychosocial level plays an important role in the successful treatment of atopic dermatitis. With regard to anti-inflammatory treatment, addressing treatment anxiety is an important factor. Both topical corticosteroids and calcineurin inhibitors can be used without hesitation. In more severe forms, the indication for systemic therapy should be examined. Dupilumab is now available as a highly effective and safe biologic for children with atopic dermatitis.
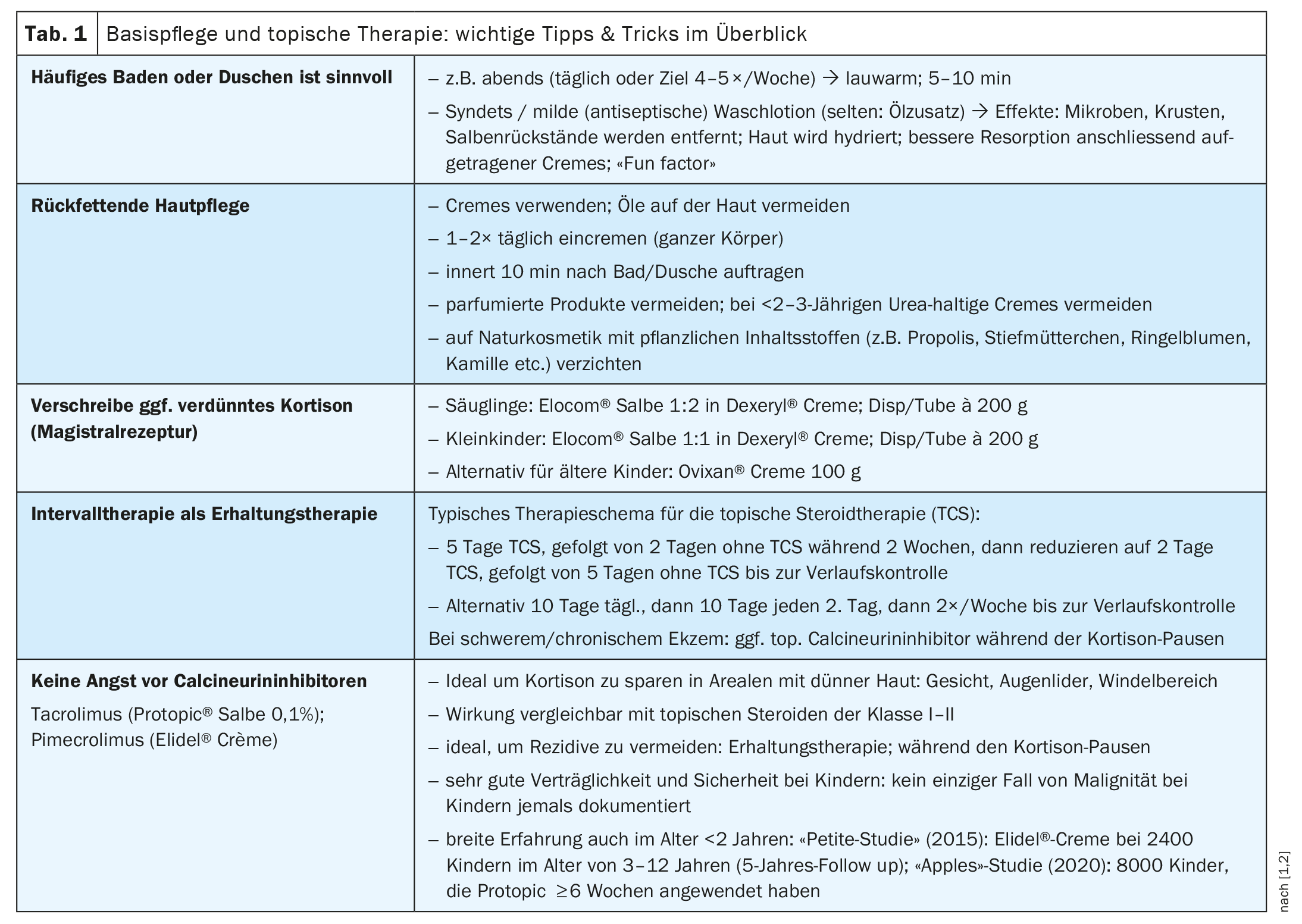
“This disease should not and does not have to be chronic and is actually well treatable at all levels,” emphasized PD Dr. med. Lisa Weibel, Head Physician, Children’s Skin Center – Dermatology, University Children’s Hospital Zurich [1]. There is often uncertainty when dealing with creams containing cortisone in atopic dermatitis (AD). People often try to postpone the use of cortisone for as long as possible for fear of side effects or due to other concerns. However, it is now known that the damage to atopic skin increases if treatment is delayed. “However, we have also learned that topical immunomodulators are absolutely ‘safe’ and have a good value for the treatment of mild and moderate eczema. And we now know that modern system therapies are available that target disease-relevant molecules, so that severe cases can now be treated very efficiently,” says Dr. Weibel [1]. The itching associated with AD not only has a negative effect on the skin, but nocturnal itching also leads to chronic sleep deprivation in many neurodermatitis sufferers. The fact that dupilumab (Dupixent®), a biologic that can be used as a systemic therapy from infancy onwards, is now available for more severe forms of AD is very encouraging, said the speaker [1].
| In order to prevent chronification and further atopic symptoms, treatment should be started as early as infancy, according to Dr. Weibel [1]. The speaker illustrated this with the following case study: A six-month-old infant had severe eczema with severe head infestation [1]. The baby had already lost 1 kg of body weight and growth had stagnated. In addition, laboratory tests showed a very pronounced blood eosinophilia. A therapy regimen with regular baths and triple-diluted mometasone followed by tacrolimus led to a healing of the eczema, but also of the general condition. “After ten days, the blood eosinophilia was gone,” says Dr. Weibel. In addition, the infant had regained body weight at the age of seven months. “The failure to thrive has completely normalized,” concluded the speaker [1]. This is an impressive example of how severe eczema can affect the overall condition and how effective adequate treatment can be [1]. If eczema is associated with failure to thrive, genetic/immunological diseases may need to be investigated in parallel with adequate AD treatment. This was also handled in the case described. |
The course of AD varies from individual to individual, but there are some patterns that are frequently encountered in everyday clinical practice. Dr. Weibel and Corinne Brunner, nursing expert APN, also from the Children’s Skin Center of the Children’s Hospital Zurich, presented some classic cases of AD patients who were referred to the Children’s Hospital Zurich for treatment [1].
The untreated infant
A patient who had had eczematous symptoms since the age of 2 months suffered from generalized eczema, itching and associated insomnia at the age of four months. He was bathed and creamed regularly, but the symptoms had not improved. As Brunner explained, new, different body lotions were used again and again when applying cream, but no local therapy was used and it was assumed that the symptoms would probably improve with age [1]. Fear of therapy on the part of the parents was a significant factor. The speaker used an 8-month-old girl who had suffered from eczema since the age of 2 months to demonstrate that there is another way. As part of the treatment prescribed by Zurich Children’s Hospital, intensive therapy was started with regular large-area application of Elocom® mixed with Dexeryl® (in a ratio of 1:2) [1,2]. Subsequently, the patient was switched to maintenance therapy; Elidel® cream was used on cortisone-free days [2]. This topical calcineurin inhibitor was also used on the face [2]. At the follow-up examination, the skin condition healed after eight weeks. In cases like these, early proactive measures, sufficiently effective therapy (i.e. a potent steroid instead of hydrocortisone) and subsequent maintenance therapy have proven to be effective for successful treatment, explained Brunner [1].
The chronic, under-treated patient
Brunner cited a 6-year-old boy who had had eczema since the age of 3 months, who had undergone a broad allergologic evaluation and various treatment attempts, including light therapy and a stay in a high-altitude clinic [1], as an example of a prolonged misguided path. Systemic and topical cortisone had also been used, but the eczema had never really healed. “He had sleepless nights because of the itching,” reported Brunner [1]. When he presented at the children’s hospital, he had a full-body infestation and there were eczematous areas with foci of bacteria. Treatment with zinc cream and selective application of Advantan® cream did not prove to be effective. After the child was admitted to hospital, topical intensive therapy was started with diluted and undiluted cortisone preparations, which were applied to the chronified areas. Long-term maintenance therapy (over a period of 1-2 years) was then arranged. The case was successfully closed at the children’s hospital two years ago. In chronic cases, an experienced treatment team and an easy-to-understand treatment plan are important. Chronic eczema can lead to sleep and behavioral disorders as well as other secondary symptoms. The children are usually easily irritable, whiny and anxious. However, it is often very stressful not only for the child itself, but also for the family.
Therapy refused – what next?
A 2-year-old boy, who had been suffering from eczema, severe itching and sleep disturbances since the age of 3 months, had been receiving homeopathic treatment since the age of six months, but had never received anti-inflammatory topical therapy [1]. The child’s parents refused topical steroids. The first step in the treatment procedure at Zurich Children’s Hospital was a parent consultation. In particular, this involved discussing the fears associated with cortisone therapy. Among other things, the parents were of the opinion that cortisone was useless, as it only treated the symptoms and did not address the causes. The parents were informed about the treatment rationale and the safety of topical corticosteroids. In time, the parents relented and topical therapy could be started with diluted and undiluted cortisone in combination with Elidel® Cream. The patient is now eczema-free at the age of 5. In cases where parents refuse therapy, cooperation with the pediatrician is very important. When setting up treatment, you should also consider whether an outpatient setting (e.g. with the support of Kinderspitex) or inpatient therapy is appropriate. Early and regular follow-up checks and a good connection are important.
“Tough nut to crack”: system therapy indicated
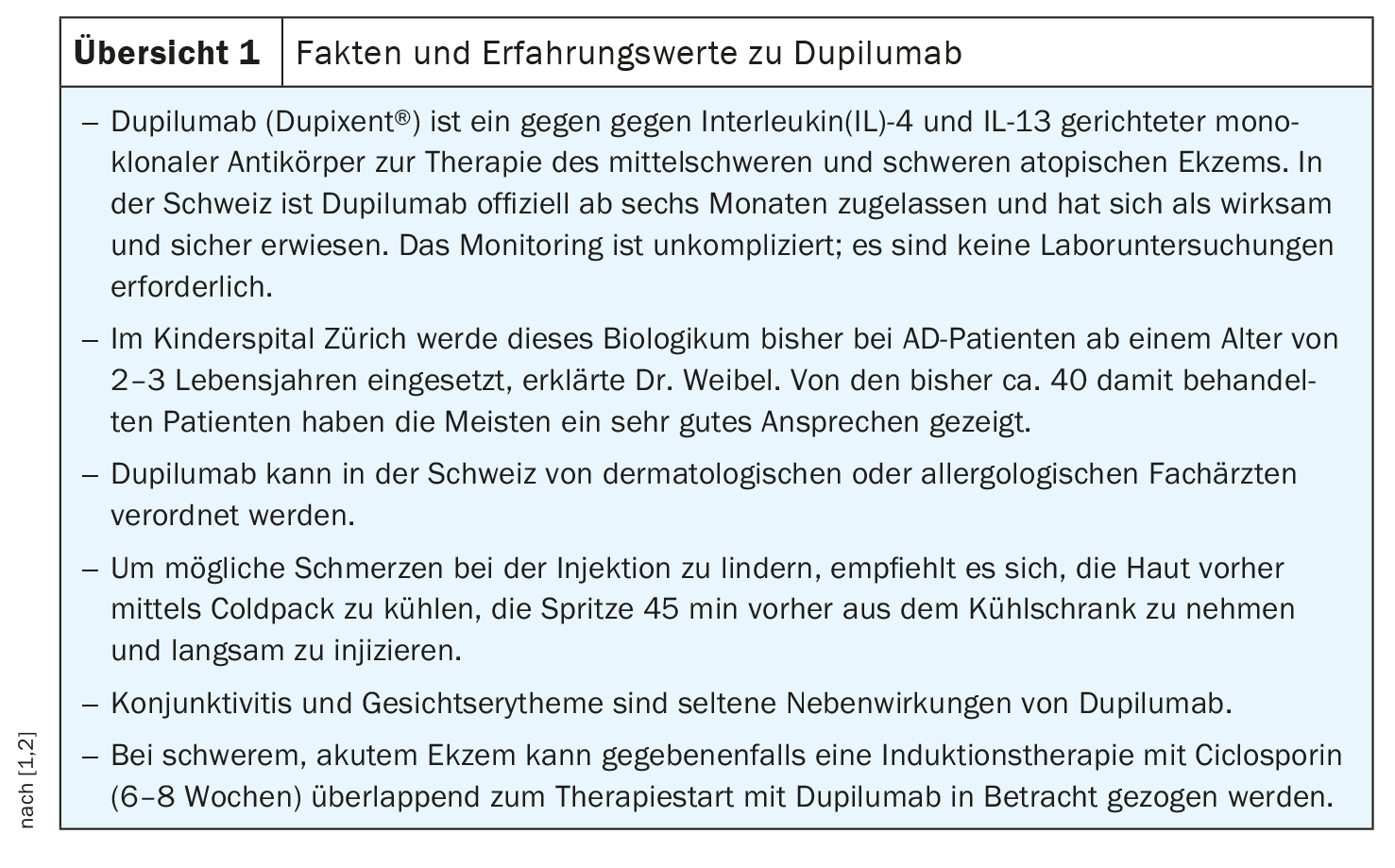
A 9-year-old female patient, who had been suffering from eczema for some time and had not responded adequately to previous treatment attempts, was admitted as an inpatient [1]. Intensive local therapy was difficult because the skin was so stressed that applying any kind of cream was painful. Treatment with oral Ciclosporin was started; the original plan was to do an overlap with Dupilumab, but the patient had a pronounced injection phobia, so this had to be put on hold and these fears had to be tackled first. After about ten days, the condition of the skin improved, but eczema and itching were still present. Over time and with psychological therapy for injection phobia, the patient agreed to biologic therapy and she was treated with Dupixent® s.c. 300 mg (Overview 1) every four weeks; Ciclosporin was stopped [1,2]. After around a year, she was eczema-free and hardly needed any more local anti-inflammatory treatment. At the same time, the quality of life for her and her family improved significantly. In this case, the speaker concluded, topical treatment alone had been used for too long and systemic therapy should have been considered earlier. Fortunately, Dupixent® then proved to be a fast and long-term effective systemic therapy [1,2].
Congress: Zurich Children’s Skin Day
Literature:
- “Atopic eczema: Why does therapy often work so poorly?”, PD Dr. med. L. Weibel; Corinne Brunner, nursing expert APN. Zurich Children’s Skin Day, 01.12.2023.
- Swissmedic: Medicinal product information, www.swissmedicinfo.ch,(last accessed 17.02.2024)
DERMATOLOGIE PRAXIS 2024; 34(1): 35-37 (published on 21.2.24, ahead of print)