Depending on individual risk factors, medication should already be used to treat osteopenia. FRAX and TOP are proven risk assessment tools. For a differentiated diagnosis, osteodensitometry can be combined with the “Trabecular bone score”. If pharmacotherapy is indicated, the risk of “rebound” effects must be considered. A combination with lifestyle measures can have a positive effect on the course.
Low mineral salt content, low bone density, and disturbed bone architecture are typical osteoporotic disease features. Bone loss may be clinically silent for a long time, but the risk of fracture is increased and even minor injuries or everyday stress can lead to a fracture. The most commonly affected parts of the body are the femur (neck of femur), upper or lower arm, ribs and spine (vertebral fracture). Women have twice the risk of osteoporosis compared to men, and this risk increases with age, as bone density decreases 3-5% per year during menopause. Half of the female population over 50 years of age in Switzerland is at high risk of osteoporosis fraction in their remaining lifetime [1]. According to prevalence data from the EPOS study, there is an age-correlated increase in women from 15% in 50-60 year olds to 45% in >70 year olds [2]. Estrogen deficiency leads to accelerated bone metabolism, and declining estrogen levels reduce calcium absorption. The risk of vitamin D deficiency and an associated reduction in calcium absorption from the intestine and calcium incorporation into the bones increases. In both sexes, secondary osteoporosis may also occur as a result of other diseases (e.g., kidney, liver, and intestinal diseases, as well as hormonal and metabolic diseases).
Intervene already in osteopenia
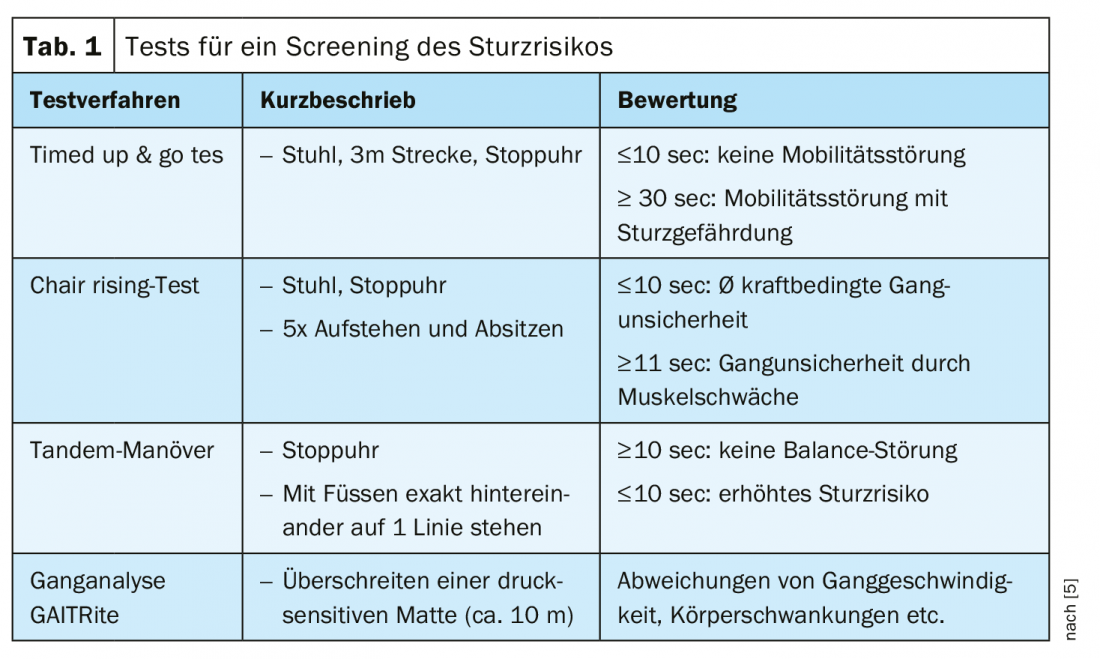
The tendency for more frequent falls without external impact is related to an increased osteoporotic fracture risk in women after menopause and in men especially in the age group 70 years and older. A bone density measurement, so-called osteodensitometry, by means of DEXA (double energy X-ray absorptiometry) gives the “bone mineral density” (BMD, g/cm2). The standardized unit of measurement is the T-score, which indicates the deviation from the mean. According to WHO [3,4], a T-score ≤-2.5 indicates a high risk of fracture and an indication for therapeutic measures. If the T-score is in the range -1.5 to -2.5, a medium risk is present according to this definition. Drug therapy is considered necessary when risk factors are present (e.g., history of fractures, age >70 years, steroid use, obesity, smoking, excessive alcohol consumption). With a T-score above -1.5, the risk is considered low and general preventive measures should suffice. In Switzerland, the costs of a DEXA are covered by the health insurance for certain indications [5]. That the risk of fracture increases with the number of fractures suffered is shown by the following figures [6]: With a BMD T-score of -2.6, the risk is about 8% if there are 0 vertebral fractures in the history, about 22% if there are 2 of them, and about 28% if ≥3 fractures have already been suffered. “We know that 90% of all fractures in old age are a consequence of falls,” summarizes Michael Gengenbacher, MD, Medical Director and Chief Physician, RehaClinic Group, Bad Zurzach [5]. For a screening of fall risk, easy to perform tests can be used (Timed up & go tes, Chair rising test, Tandem maneuver, Gait analysis GAITRite) (Tab. 1).
Combination of TBS and BMD increases diagnostic significance
Densitometry measures only the mineral content of the bone and is not equivalent to an assessment of individual fracture risk. It has been shown that a supplementary determination of the TBS (“Trabecular bone score”) value allows a more differentiated assessment of the fracture risk than BMD measurement alone [7]. The TBS is a structural metric that evaluates the variations in gray levels of individual pixels in the DEXA image of the lumbar spine and provides an indirect index of trabecular microarchitecture. TBS correlates with bone microarchitecture parameters (analysis of the spatial arrangement of pixel intensity corresponding to the differences between the X-ray absorptivity of an osteoporotic bone and that of a healthy cancellous bone). A secondary analysis has shown that TBS levels have been shown to be associated with the occurrence of fractures [7]. In postmenopausal women and in men with previous fractures, TBS levels are lower than in fracture-free individuals [8]. In addition, TBS is associated with bone fracture risk in individuals with conditions associated with reduced bone mass or bone quality. In addition to a prognostic value, it is a parameter relevant for follow-up.
Include 10-year fracture risk
The speaker emphasized the relevance of early detection of risk factors and appropriate measures even in cases of low risk according to the T-score: “Most fractures in the spine occur in osteopenia”. Osteopenia is a precursor of osteoporosis and is defined by a BMD 1-2.5 standard deviations below the T-score mean (osteoporosis: BMD < -2.5). To address this, WHO has created and disseminated an Internet-based fracture risk calculation tool [8]:
The Fracture Risk Assessment Tool (FRAX). This allows the 10-year fracture risk to be calculated for the major 4 osteoporotic fractures (“major osteoporotic fractures”: vertebrae, proximal humerus, distal radius, and hip) or in isolation for the hip fracture. The TOP SGR tool of the Osteoporosis Platform of the Swiss Society of Rheumatology is an instrument adapted to Switzerland to determine the 10-year fracture risk of 50-90-year-old patients [9]. In contrast to the FRAX, it is intended to be a concrete decision aid for the physician regarding the following aspects: 1) Indication for bone densitometry with DEXA in suspected osteoporosis, 2) Indication for drug treatment (in addition to calcium and vitamin D) in patients with decreased bone density after calculating the absolute risk of fracture in the next 10 years, 3) Cost coverage by health insurance depending on relevant factors (e.g. risk factors, bone density values, indication, limitatio).
Individually adapted pharmacotherapy – avoiding “rebound” effects
Currently, bisphosphonates, denosumab, selective estrogen receptor modulators (SERM), and teriparatide (Forsteo®) are used in Switzerland to treat osteoporosis. Antiresorptive substances inhibit bone resorption, anabolic substances promote bone formation [10,13]. Anabolic-acting preparations are particularly suitable for osteoporosis of high severity and in cases of poor response or intolerance to other active substances.
Bisphosphonates (antiresorptive via osteoclast inhibition): Alendronate, risedronate, and zoledronate reduce vertebral, hip, and non-vertebral fractures. For ibandronate, only vertebral fracture reduction has been documented to date. For therapy duration >3/5 years, the evidence base is so far low.
Denosumab (antiresorptive via RANK-L inhibition): Risk reduction of vertebral and hip fractures (by 70% and 40%, respectively). BMD increase could still be demonstrated after 10 years. Rebound with risk of multiple vertebral body fractures: occurrence 5 to 18 months after stop; incidence data highly variable (5-15%).
SERM: Raloxifene and bazedoxifene reduce vertebral fractures by about 30-40% (CAVE thrombosis risk, cardiovascular risk, vasomotor symptoms).
Teriparatide (anabolic): reduces vertebral and non-vertebral fractures (hip fractures not yet proven). Optimal treatment duration unclear, follow-up therapy important. According to randomized trial in severe osteoporosis better efficacy than risedronate [11].
The duration of treatment depends on the patient or his individual fracture risk on the one hand, and on the preparation on the other hand [12]. If treatment is too short, the risk of fracture remains elevated. After discontinuation of a therapeutic agent, regular follow-up should be performed and, if bone mineral content deteriorates or a new fracture occurs, a new cycle of therapy may be considered based on an individual benefit-risk analysis. Bisphosphonates may be discontinued or paused during the course of therapy because of their residual long-term effects in patients at low to moderate risk.
Denosumab significantly improves bone mineralization and thus bone density, but after discontinuation of therapy, a rebound effect may occur due to decreasing inhibition of bone resorbing cells (osteoclasts). To reduce the risk of vertebral fractures and bone mineral density loss after discontinuation of therapy with Prolia® (denosumab), sequential therapy with a bisphosphonate for 12-24 months is indicated [14,16].
The bone-forming monoclonal antibody Romosozumab (Evenity®) has recently been approved in the EU [15]. The drug has a dual action, increasing bone formation on the one hand and decreasing bone resorption on the other.
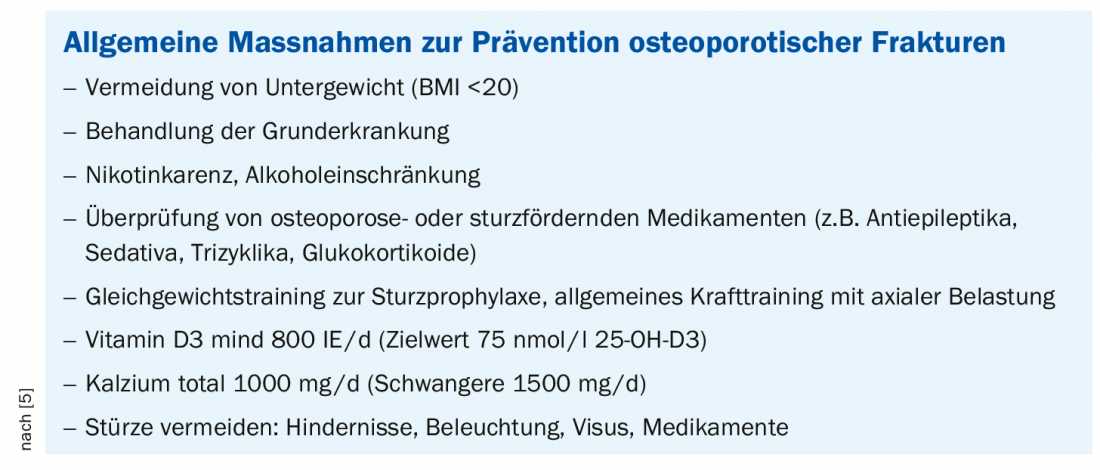
Regarding lifestyle factors as complementary measures, the recommendations according to SVGO are as follows [12]: sufficient calcium intake (1000 mg/day) and vitamin D supply (≥800 E/day, ev. Vitamin D supplementation) as well as a balanced diet with sufficient protein intake (1 g/kg body weight) and regular physical activity, fall prevention and avoidance of risk factors (e.g. smoking, excessive alcohol consumption).
Literature:
- brainMAG: Interview with Elisabeth Treuer Felder, MD, by Athena Tsatsamba Welsch. brainMAG Neurology Psychiatry Geriatrics 2019; 1: 37-40.
- Gourlay ML, et al: Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med 2012; 19; 366(3): 225-233.
- WHO, www.who.int
- AACE Guidelines, American Association of Clinical Endocrinologist, www.aace.com
- Gengenbacher M: Osteoporosis 2020 – News from diagnostics and therapy. Michael Gengenbacher, MD, Medical Director and Chief Physician, RehaClinic Group, FOMF Basel, Jan. 30, 2020
- Siris ES, et al: Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 2007; 18: 761-770.
- Silva BC, et al: Trabecular Bone Score: A Noninvasive Analytical Method Based Upon the DXA Image. J Bone Miner Res 2014; 29(3): 518-530.
- FRAX, www.sheffield.ac.uk/FRAX/Tool
- SGR: Swiss Society of Rheumatology, www.rheuma-net.ch/de/aktuelles
- Schmid G: Osteoporosis – Update Dr. med. Gernot Schmid, advanced training 22.03.2019, www.luks.ch
- Kendler DL, et al: Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 2018; 391(10117): 230-240.
- SVGO (Swiss Association against Osteoporosis): Recommendations 2015. www.svgo.ch
- Haas AV, LeBoff MS: Osteoanabolic Agents for Osteoporosis. J Endocr Soc 2018; 2(8): 922-932.
- Swissmedic: www.swissmedic.ch/swissmedic/en/home/humanarzneimittel/market-surveillance/
- Evenity®: https://arznei-news.de/romosozumab/
- Medix: www.medix.ch/wissen/guidelines
HAUSARZT PRAXIS 2020; 15(3): 20-22 (published 3/24/20, ahead of print).