In the case of arthritic complaints, regular progress assessment using the ACR/EULAR criteria is significant so that the time for disease-modifying therapy is not missed. Controlling disease activity at an early stage of the disease has a favorable prognostic impact.
Undifferentiated rheumatic diseases refer to symptoms in which some manifestations of a rheumatic disease are present, but the classification criteria are not fully met at the time of diagnostic workup, explains Prof. Pius Brühlmann, MD, Rheumaklinik Bethanien, Zurich [1]. In these patients, it is important to re-evaluate the symptomatology as soon as new signs of disease appear. Most patients with new-onset musculoskeletal symptoms first contact their primary care physician, who plays a critical role in the management of early rheumatic disease.
Early stage of rheumatoid arthritis?
While diagnosis is relatively straightforward in established rheumatoid arthritis, this disease may still be discrete, atypical, or only transiently symptomatic in early phases [2]. Empirical studies on predictors for the transition of an early, undifferentiated arthritis into a persistent or destructive inflammatory joint disease, could demonstrate the importance of anamnestic (duration and localization of symptoms), clinical (findings and distribution of synovitis) and serological findings for the diagnosis of early rheumatoid arthritis [2,3]. Serologic findings in this context include detection of rheumatoid factors and antibodies to cyclic citrullinated peptides. The ACR/EULAR classification criteria are based on these risk factors and facilitate early diagnosis of rheumatoid arthritis and early initiation of disease-modifying therapy [4]. According to this classification scheme, a score ≥6 points is rheumatoid arthritis [4] (overview 1).
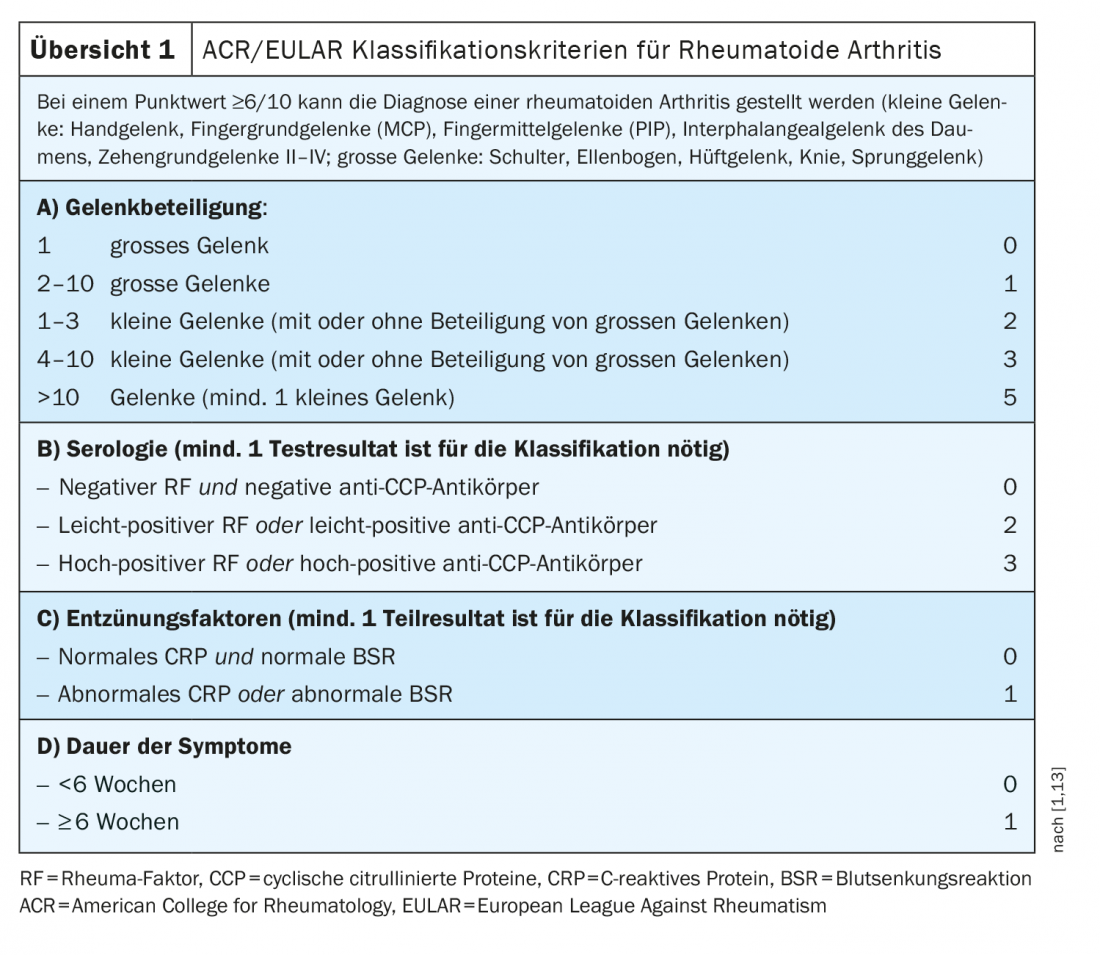
A score of 5 increases the likelihood that rheumatoid arthritis will manifest later, but such arthritis is not classifiable at this time.
Differentiation from osteoarthritis is important
A critical factor in the detection of early arthritis is the distinction between arthritis and arthralgia alone. A typical sign of arthritis is a palpable, soft, “elastic” swelling of a joint due to effusion and/or inflammatory thickening of the synovium (synovitis, synovialitis), accompanied by pain and joint stiffness [5]. Regarding the distinction between arthritis and osteoarthritis, a statement in the 2019 new edition of the S3 guideline on the management of early rheumatoid arthritis reads as follows: “The likelihood of developing rheumatoid arthritis increases with the number of affected joints and their distribution among the four extremities, as well as the duration of morning stiffness over 30 min [9–11]which does not recur during the day – even after periods of rest (in contrast to recurrent joint stiffness and recurrent start-up pain after short periods of rest in osteoarthritis). Arthritis typically causes discomfort even at rest; in osteoarthritis, these are mainly load- and movement-dependent. Medium and large joints may also be affected in the early phase of the disease. Joint changes in the finger end joints, thumb saddle joints, and big toe metacarpophalangeal joints are usually arthritic, and therefore these joints are specifically excluded from evaluation under the new classification criteria for rheumatoid arthritis [12].”
Disease-modifying basic therapy counteracts joint destruction
The underlying joint inflammation of rheumatoid arthritis leads not only to painful and swollen joints and functional limitations, but also to progressive joint destruction if inadequately treated [5]. Long-acting antirheumatic drugs are used in basic therapy, which means that the effect of these drugs takes several weeks to months to appear. These so-called disease-modifying anti-rheumatic drugs (DMARDs) alter the course of the disease by targeting the inflammatory processes in the immune system, slowing down the inflammatory process and, in the best case, bringing it to a halt, whereupon the symptoms subsequently recede [5]. Currently available on the market are conventional disease-modifying agents (csDMARDs), biologics and biosimilars (bDMARDs), and partially synthetic DMARDs (tsDMARDs). As recent studies have shown, rapid control of disease activity by early initiation of therapy with disease-modifying agents has a positive effect on further prognosis [2,6–8]This implies that coordinated collaborative multidisciplinary care is ensured so that disease signals are correctly interpreted as early as possible and the indication for disease-modifying therapy is assessed [5].
Literature:
- Brühlmann P: Undifferentiated diseases in rheumatology. Pius Brühlmann, MD, FOMF Update Refresher (Livestream), June 26, 2020.
- Combe B, et al: Annals of the rheumatic diseases 2017; 76: 948-959.
- Emery P, et al: Annals of the rheumatic diseases 2002; 61: 290-297.
- Radner H, et al: Arthritis Research & Therapy 2014; 16: Article number: R56.
- Schneider M, et al: Guideline for the management of early rheumatoid arthritis. German Society of Rheumatology 4th edition, Last content update: 12/18/2019, valid until 12/17/2024.
- van Nies JA, et al: Ann Rheum Dis 2015; 74: 806-812.
- Emery P: Br J Rheumatol 1995; 34(Suppl 2): 87-90.
- Machold KP, et al: J Rheumatol Suppl 1998; 53: 13-19.
- van der Helm-van Mil AHM, et al: Arthritis Rheum 2007; 56: 433-440.
- van der Helm-van Mil AHM, et al: Arthritis Rheum 2008; 58: 2241-2247.
- Visser H, et al: Arthritis Rheum 2002; 46: 357-365.
- Aletaha D, et al: Ann Rheum Dis 2010; 69: 1580-1588.
HAUSARZT PRAXIS 2020; 15(12): 42-43