Prof. Dr. med. Michael Dickenmann, deputy. Chief of Nephrology and Transplantation Immunology, Basel, discusses the nephrological consequences of hypertension and its effective treatment in this interview. Furthermore, he mentions the advantages of living kidney donation and discusses aspects of diabetic as well as atherosclerosis-associated nephropathy.
Prof. Dickenmann, hypertension is a widespread disease, but at the same time many people may not notice it for years. How dangerous is this condition for the kidneys and how can it be prevented?
Prof. Michael Dickenmann, MD: Arterial hypertension, together with the other cardiovascular risk factors, is responsible for about one fifth of chronic kidney failures in Switzerland. This shows their dangerousness. Often it is not hypertension alone but, as with all vessels, a combination of all cardiovascular risk factors that leads to chronic nephropathy. Early detection and treatment, preferably with an ACE inhibitor or an angiotensin antagonist, is essential to prevent or delay the progression of chronic nephropathy.
The diagnosis of hypertension is easy to make, but there are different approaches to therapy. In which cases do you advise patients to make lifestyle changes (stress reduction, weight loss), and in which cases do you use drug therapy?
In my personal experience, lifestyle modification can support the treatment of arterial hypertension, but it is not sufficient on its own. Both in the prevention and treatment of arterial hypertension, salt restriction is a very efficient measure. However, this therapy is often not tolerated due to the reduction in quality of life.
Kidney damage can also cause secondary hypertension. Does a vicious circle develop here (increase in blood pressure, damage to the kidneys, renewed increase in blood pressure)?
Exactly! Therapeutically, it is important to break this vicious circle, the sooner the better. The combination of an antihypertensive with a diuretic is a logical consequence. The diuretic treats secondary volume (=salt) hypertension.
In case of kidney failure: the number of organ donations from deceased patients is relatively low in Switzerland, transplant candidates are usually on the waiting list for years. Living kidney donations, on the other hand, are on the rise. What are the advantages of this type of transplant?
Living kidney donation is the oldest and most successful kidney replacement procedure. It was first successfully performed in 1954, almost ten years before hemodialysis treatment became commonplace in clinical practice. Living donated kidneys function longer than organs from deceased patients, and patient survival is significantly better than long-term dialysis treatment in all age groups. A successful transplant enables a normal life with a good quality of life. Finally, living kidney donation makes economic sense because the cost of transplantation and long-term costs are much lower than chronic dialysis treatment. The living donor rate in Switzerland is among the highest in the world. Up to 50% of all kidney transplants in our country are performed by living donors.
What are the risks and long-term consequences of living donation for the donor?
Basically, you live with one kidney the same length of time and just as well as with two if you are healthy and have normal kidney function at the time of donation. In Switzerland, no living kidney donor has died as a direct result of organ removal. Worldwide, there is a mortality risk of 0.03%. The surgery itself carries all the risks of an elective urinary tract procedure. In the long term, blood pressure, kidney function and protein excretion in the urine must be monitored periodically. The significance of described chronic fatigue after kidney donation is unclear.
About one-third of diabetics develop diabetic nephropathy after 15 to 20 years. Early detection is important here to prevent dialysis. What are the symptoms for diagnosis?
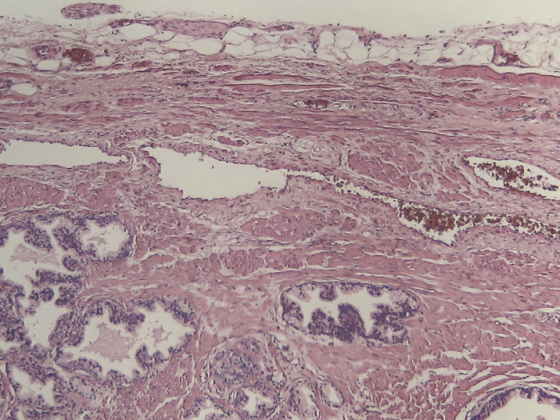
Unfortunately, there are no clinical symptoms that indicate the development of diabetic nephropathy. Regular protein screening in urine can look for diabetic nephropathy. But beware: not every diabetic has diabetic nephropathy! Therefore, when in doubt, a kidney biopsy is useful to avoid missing other potentially treatable causes.
What measures are critical to curbing the progression of diabetic kidney disease?
Consistent blood pressure control and a reduction of proteinuria by at least 50% are critical. ACE inhibitors or angiotensin antagonists are the first choice!
To what extent is kidney damage associated with atherosclerosis?
Frequently! And it goes both ways, i.e., atherosclerosis favors chronic nephropathy and chronic nephropathy favors the development of atherosclerosis.
Interview: Andreas Grossmann
CARDIOVASC 2013; 12(6): 27-28