Carcinoma of the urinary bladder is one of the common malignant diseases. While the prognosis of patients with superficial tumors is usually favorable, the situation is much worse for muscle-infiltrating and organ-transcending urothelial carcinoma. But something is happening in the treatment management of advanced/metastatic bladder cancer. In particular, treatment with immune checkpoint inhibitors is highly effective after radical resection.
Every year, around 1150 people in Switzerland are newly diagnosed with urothelial carcinoma of the urinary bladder. This makes it one of the most common forms of cancer in older people. Men are affected in around three quarters of all cases, making bladder cancer the fourth most common tumor in men and the ninth most common tumor in women. The origin of the malignant mass is usually found in the mucous membrane of the urinary tract. A distinction is made between non-muscle-invasive bladder carcinoma and muscle-invasive bladder carcinoma. 75% of all bladder carcinomas are in a non-muscle-invasive stage. The pathomechanisms of urothelial carcinoma are complex. One pathway, for example, is associated with genetic alterations in the FGFR3 and HRAS genes, which activates the RAS/MEK/ERK signaling pathway. The immune system plays a decisive role with pro- and anti-tumor effects. The contributing factors include chronic bladder infections, smoking, the use of certain medications and contact with various chemicals.
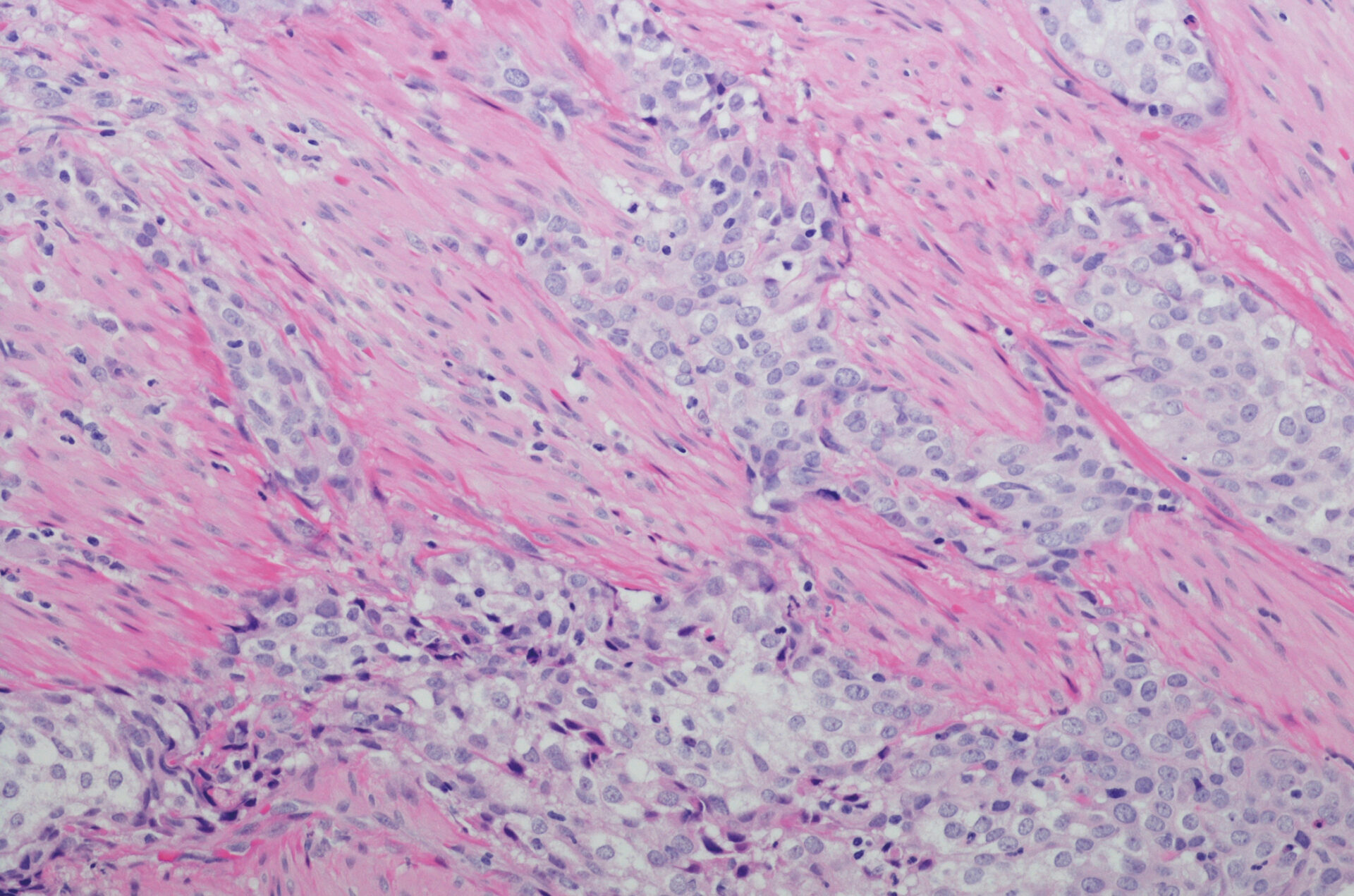
Non-specific irritation symptoms such as pollakiuria, dysuria or urinary urgency may indicate the presence of bladder cancer. The main symptom is ultimately hematuria in the form of microhematuria or painless macrohematuria. If a diagnosis is suspected, an imaging procedure such as ultrasound, computed tomography (CT), CT urography and magnetic resonance imaging (MRI) is used in addition to a palpation examination of the abdomen and kidneys. This is usually followed by a cystoscopy with the removal of a tissue sample. CT and urography can be used to determine whether the tumor has spread to surrounding tissue or affected other organs. The histopathological classification is based on the WHO classification for bladder tumors.
Something is happening in the metastatic setting
Treatment management depends on the histology, stage and other risk factors. First-line treatment for non-muscle-invasive bladder cancer focuses on local therapeutic measures such as transurethral bladder resection (TURB) and instillation therapy. If, on the other hand, the tumor is locally advanced or metastatic, systemic neoadjuvant, adjuvant or palliative drug treatment is of great importance. Platinum-based chemotherapy is primarily used, but other substances such as checkpoint inhibitors are also playing an increasing role.
Radical cystectomy is the standard treatment for muscle-invasive urothelial carcinoma of the bladder. While organ-confined tumors show high cure rates after complete resection, organ-transcending tumors with or without accompanying lymph node metastases are associated with a high risk of recurrence of up to 80%. Adjuvant chemotherapy should therefore be given. Cisplatin-eligible patients. with a high risk of recurrence after curative radical cystectomy and lymph node metastases usually receive 3-4 cycles of gemcitabine/cisplatin. However, there is also a considerable proportion of patients who refuse adjuvant polychemotherapy after curative surgery or do not receive it due to other factors (multimorbidity, impaired kidney function, etc.). Immune checkpoint inhibitors show good efficacy here.
Further reading:
- www.onkopedia.com/de/onkopedia/guidelines/blasenkarzinom-urothelkarzinom/@@guideline/html/index.html (last accessed on 06.12.2023)
- www.dgho.de/publikationen/stellungnahmen/fruehe-nutzenbewertung/nivolumab/nivolumab-urothelkarzinom-stellungnahme-20220822.pdf (last accessed on 06.12.2023)
- www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/krebsarten/andere-krebsarten/blasenkrebs/definition-und-haeufigkeit.html (last accessed on 06.12.2023)
- NICER: National cancer incidence statistics. www.nicer.org/de/statistiken-atlas/krebsinzidenz (last accessed on 06.12.2023)
- www.gekid.de (last accessed on 06.12.2023).
InFo ONCOLOGY & HEMATOLOGY 2023; 11(6): 37