Erysipelas and limited phlegmon are common soft tissue infections in immunocompetent individuals. Regarding differential diagnosis, the relevant literature mentions that a stronger systemic inflammatory reaction indicates erysipelas. To verify this empirically, laboratory chemistry parameters were compared with clinical findings in a study published in the JDDG. Correlates could be identified, which are helpful for the differential diagnosis.
Erysipelas (Fig. 1) and limited phlegmon differ in particular with regard to the underlying microbial cause [1]. Erysipelas, also called erysipelas, is an acute bacterial non-purulent infection of the dermis and lymphatics caused by beta-hemolytic streptococci, usually group A (Streptococcus pyogenes) [1]. Infection usually begins through very small ports of entry (such as interdigital mycosis), and spreads into the dermis and along lymphatic clefts. Clinically, erysipelas is characterized by acute, overheated, mildly painful bright red erythema with a shiny surface, sharply defined border, and tongue-like extensions, usually accompanied by a systemic inflammatory reaction with fever and/or chills [2]. In contrast, limited phlegmon is often caused by Staphylococcus aureus [1,2]. Clinically, warm, mildly painful erythema is characteristic. Compared to erysipelas, this is more edematous, the redness is darker, and the margins are less sharply defined. Most commonly, limited phlegmon develops around larger ports of entry such as wounds or ulcers.

Erysipelas can be effectively treated with penicillin
Since beta-hemolytic streptococci have not yet developed resistance to penicillin, erysipelas can be treated very efficiently with the well-tolerated penicillin despite its narrow spectrum of activity [1]. This has minimal potential for selection of resistant strains or collateral damage to the microbiome of other organs [3]. In limited phlegmon, on the other hand, the pathogenic germs (usually Staphylococcus aureus) are often resistant to penicillin. In some cases, gram-negative bacteria cannot be excluded as causative agents. In many cases, first-generation flucloxacillin or cephalosporins are sufficient [4], but broader-spectrum antibiotics are often prescribed to cover Gram-negative pathogens. In the absence of adequate treatment of limited phlegmon, it may develop into severe phlegmon, often purulent and extending to the fascia. In such a case, surgical treatment is required in addition to antibiotic treatment [1]. This also applies to life-threatening necrotizing fasciitis.
Differential diagnosis can be difficult
The clinical differential diagnosis between erysipelas and limited phlegmon can be challenging in some cases, especially when the site of infection also looks altered by noninfectious inflammatory processes, such as stasis dermatitis. Therefore, additional diagnostic criteria are required. There is evidence in the literature that limited phlegmon is associated with a less pronounced clinical inflammatory response (fever, chills) and with lower laboratory inflammatory parameters compared with erysipelas, but a study explicitly addressing this issue has been lacking [1]. CRP and leukocyte count are considered established markers for bacterial infections [5–7], but not much data exist on the relevance of these parameters in the differential diagnosis of soft tissue infections [8].
This was the starting point of the 2020 study described below and published in the Journal of the German Dermatological Society, in which relevant laboratory chemistry parameters were identified to differentiate between erysipelas and limited phlegmon [1].
Retrospective analysis to detect laboratory chemistry differences.
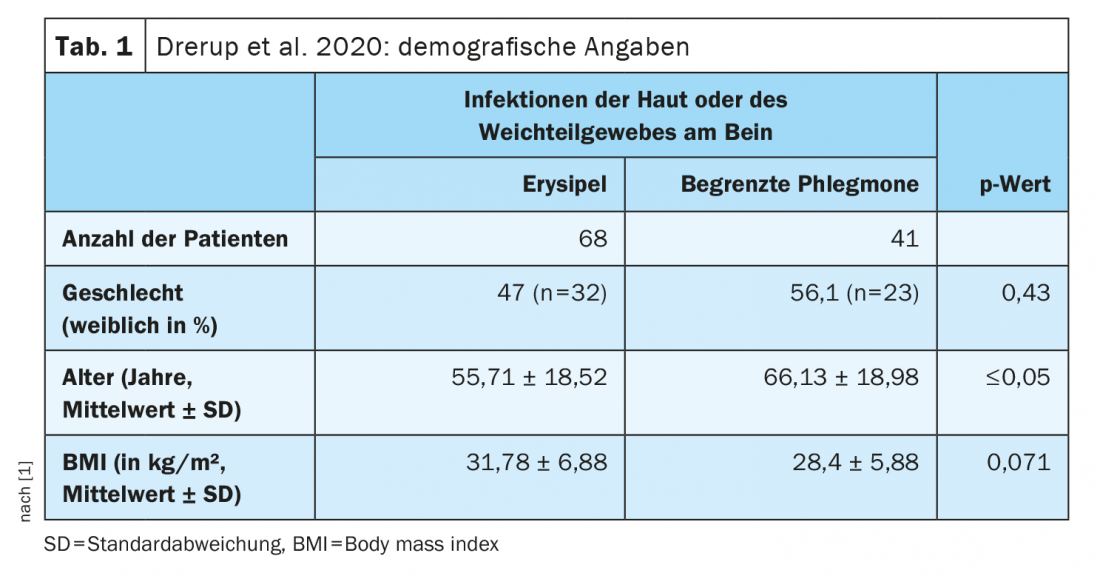
The study included 163 patients with skin and soft tissue infections. Laboratory parameters of patients with erysipelas (n=68) were compared with those of patients with limited phlegmon (n=41) (Tab. 1). All cases were leg infections. The diagnosis of “erysipelas” or “limited phlegmon” was made clinically; in addition, a rapid response to penicillin was taken as confirmation of the diagnosis of “erysipelas.”
Laboratory diagnostic evaluations showed that the inflammatory response was more pronounced in erysipelas. Overall, patients with erysipelas had significantly higher values (p≤0.05) of body temperature, CRP, leukocytes, erythrocytes, monocytes, and immature granulocytes compared to patients with limited phlegmon. In contrast, the number of eosinophils was higher in the patients with limited phlegmon (p=0.05) (Tab. 2). The best parameters to distinguish between erysipelas and limited phlegmon were CRP and leukocyte count. A CRP value of ≥3.27 mg/dl spoke to the diagnosis of “erysipelas” with over 70% sensitivity and specificity. Statistical analyses controlling for the factor of age showed an age-adjusted OR 1.13 per 1 mg/dl CRP in logistic regression, specifically meaning that the higher the CRP, the more likely the diagnosis of erysipelas. From random forest analysis and logistic regression, the combination of CRP, leukocytes, and body temperature was best at discriminating between erysipelas and limited phlegmon. Thus, higher leukocyte counts and higher body temperature were also more likely to indicate erysipelas. The results on CRP and leukocytes and neutrophils were as follows:
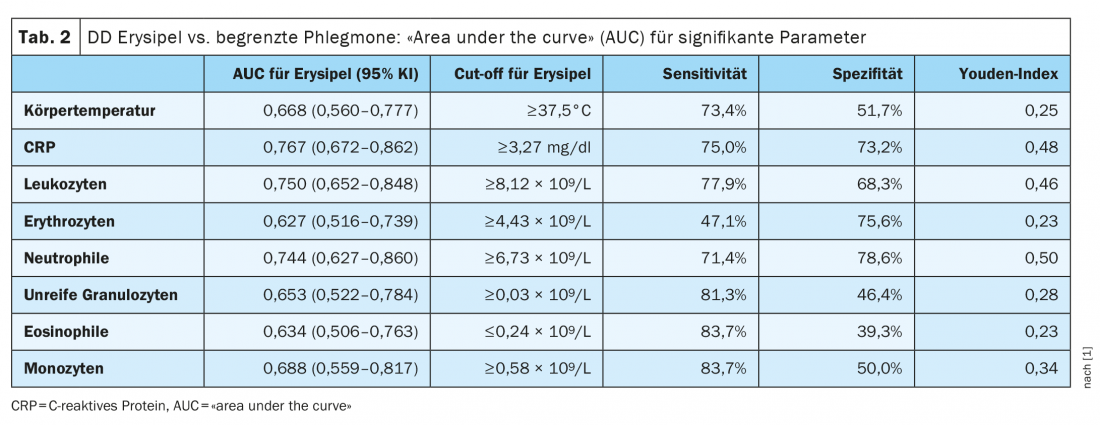
CRP: The investigators found that a threshold of ≥3.27 mg/dl for CRP indicated a diagnosis of erysipelas versus limited phlegmon with a sensitivity of 75% and a specificity of 73.2%. While only 1.5% (1/68) of patients with erysipelas had a CRP of <0.5 mg/dl on hospital admission, this was true for 12.2% (5/41) of patients with limited phlegmon. These data are consistent with previous findings that 3-12% of patients with SSTI had normal CRP levels on admission [9,10].
leukocytes and neutrophils: The optimal cut-offs for the diagnosis of erysipelas are 8.12 ×109 /L for leukocytes and ≥6.73 ×109 /L for neutrophils. Compared with CRP values, AUCs were only slightly lower in the ROC analysis, and cut-off values showed similar sensitivity and specificity.
Literature:
- Drerup C, et al: Diagnostic value of laboratory parameters in distinguishing erysipelas from limited phlegmon. JDDG 2020; 18(12): 1417-1425.
- Sunderkötter C, et al: S2k Guideline Skin- and Soft tissue infection – Excerpt from S2k Guideline Calculated initial parenteral therapy of bacterial infections in adults. J Dtsch Dermatol Ges 2019; 17(3): 345-369.
- Zimmermann P, Curtis N: The effect of antibiotics on the composition of the intestinal microbiota – a systematic review. J Infect 2019; 79(6): 471-489.
- Sunderkötter C, Becker K: Frequent bacterial skin and soft tissue infections: diagnostic signs and treatment. J Dtsch Dermatol Ges 2015; 13(6): 501-524; quiz 525-526.
- Chalupa P, et al: Evaluation of potential biomarkers for the discrimination of bacterial and viral infections. Infection 2011; 39(5): 411-417.
- Bruun T, et al: Early response in cellulitis: a prospective study of dynamics and predictors. Clin Infect Dis 2016; 63(8): 1034-1041.
- Brindle RJ, Ijaz A, Davies P : Procalcitonin and cellulitis: correlation of procalcitonin blood levels with measurements of severity and outcome in patients with limb cellulitis. Biomarkers 2019; 24(2): 127-130.
- Bruun T, et al: Etiology of cellulitis and clinical prediction of streptococcal disease: a prospective study. Open Forum Infect Dis 2016; 3(1): ofv181.
- Lazzarini L, Conti E, Tositti G, deLalla F: Erysipelas and cellulitis: clinical and microbiological spectrum in an Italian tertiary care hospital. J Infect 2005; 51(5): 383-389.
- Noh SH, Park SD, Kim EJ: Serum procalcitonin level reflects the severity of cellulitis. Ann Dermatol 2016; 28(6): 704-710.
DERMATOLOGY PRACTICE 2021, 31(6): 47-48