Ulcus cruris venosum is the most severe form of chronic venous insufficiency. Despite gold standard therapy using compression and phase-adapted hydroactive wound treatment, it is not uncommon for patients with an open leg to develop a refractory course. The development and evaluation of new methods and therapeutic approaches can contribute to an improvement in the care and treatment situation.
One of the most common manifestations of chronic wounds in Europe is leg ulcers (Fig. 1) [1]. Therapeutically, debridement is essential for most patients in order to remove avital tissue. This should be followed by modern, phase-adapted wound treatment and compression therapy [1]. For patients with stagnant wound healing, it is recommended that general practitioners or primary care providers involve specialized specialists or an interdisciplinary and interprofessional wound center or clinics with a focus on vascular medicine or phlebology in the treatment at an early stage [2].
POET study: patient education pays off
A multi-professional team from Erlangen University Hospital and Martha Maria Hospital in Nuremberg, with the participation of PD Dr. med. Cornelia Erfurt-Berge, presented a poster at the Wound Congress on a project in which an individual patient book on venous leg ulcers was developed and evaluated [3,4]. Particular emphasis was placed on patient-oriented wording and meaningful structuring in order to motivate patients to actively participate in the treatment process. The patient book, which is divided into various chapters, contains background information on the benefits of compression therapy, for example, and covers the topics of exercise, nutrition and skin care.
The POET study tested the following hypothesis from February 2021 to March 2022: Self-determined participation in the treatment of venous leg ulcers and the provision of understandable information in this regard can help patients to better understand the pathogenesis of the disease, understand the usefulness of the treatment and improve the management of their disease. A patient survey was conducted twice on 24 test subjects at intervals of six weeks. The following components were surveyed:
- Health-related data
- Checking the compression bandage used
- Questionnaire regarding the patient book
- Wound-QoL
- Feedback questionnaire on graduation
The results showed significant improvements in wound size, total score of the compression bandage, knowledge of the pathogenesis and understanding of the usefulness of the treatment. The disease-related quality of life also improved. On average, patients stated that they had read the patient book three times.
Catheter-assisted sclerotherapy of the next generation
Dr. Savvas Apostolidis from the Clinic for Vascular and Endovascular Surgery at the Red Cross Clinics in Frankfurt presented the first medium-term results of catheter-assisted sclerotherapy of the next generation and demonstrated its contribution to modern ulcer therapy [5]. The new endovenous non-thermal procedure enables varicose vein treatment without anesthesia, without incisions and without tumescent anesthesia. It can be used for all patients without interrupting anticoagulation and regardless of the distance between the vein to be treated and the skin under outpatient conditions. Special attention is paid to ulcer patients. The key to success is a patented double lumen catheter and a double procedure syringe. This allows the inserted sclerosant foam and the blood in the vessel to be aspirated.
Short and medium-term results (max. follow-up up to 19 months) are available for the method:
- The closure rate is well over 90% and continues to increase with user experience
- The compression treatment lasts a few days.
- The esthetic result is outstanding.
- The cosmetically disturbing brownish discoloration observed with “simple” foam sclerotherapy is eliminated.
- The healing of venous ulcers is greatly accelerated.
- All patients were positively surprised by the procedure and there were no serious complications during the treatment of the first 200 or so patients.
New device for intermittent pneumatic compression of the thigh
A team from the Nursing Research Group of the Geriatrics Research Group at Charité – Universitätsmedizin Berlin presented intermittent pneumatic compression (IPC) using a new device (“WoundExpress”) based on two case studies [6]. IPC is an additional way of improving blood circulation and favorably influencing physiology in various areas:
- Increase in venous return flow and thus reduction of venous hypertension
- reactive improvement of arterial blood flow by increasing the arterio-venous pressure gradient
- Enhancement of profibrinolytic mechanisms through increased endothelial stress.
The treatment courses outlined below illustrate the IPC procedure for two elderly patients with venous leg ulcers. The “WoundExpress” used for the IPC has a chambered cuff that is placed around the thigh, similar to the blood pressure measurement on the upper arm. The circular chambers are automatically inflated with air one after the other for two minutes until a pressure of 60 mmHg is reached. After the inflation phase, the cuff is deflated for a further two minutes, during which no pressure is exerted on the thigh. These four-minute cycles are repeated during the application. The course of treatment was documented and analyzed every two weeks using a special camera and 3D wound imaging software.
Case example 1: 72-year-old patient with a venous leg ulcer that has been present for two years and the following secondary diagnoses: type 2 diabetes mellitus, chronic renal insufficiency (stage 2), suprapubic urinary bladder catheter after prostatectomy, anemia, heart failure, visual and hearing problems. At the beginning of the study, the ulcer had an extension of 16.3 cm² and showed good granulation. After six weeks of standard therapy plus IPC, the wound size had halved and after 13 weeks there was still a minimal lesion of 0.9 cm².
Case study 2: 82-year-old female patient with a recurrent venous leg ulcer that had been present for 2.5 months. Apart from post-thrombotic syndrome, no previous illnesses were known. The ulcer had an initial size of 13.2 cm². The wound bed was found to contain approximately 85% granulation tissue and 15% fibrin coating. Participation in the study ended prematurely after 12 weeks with complete wound closure.
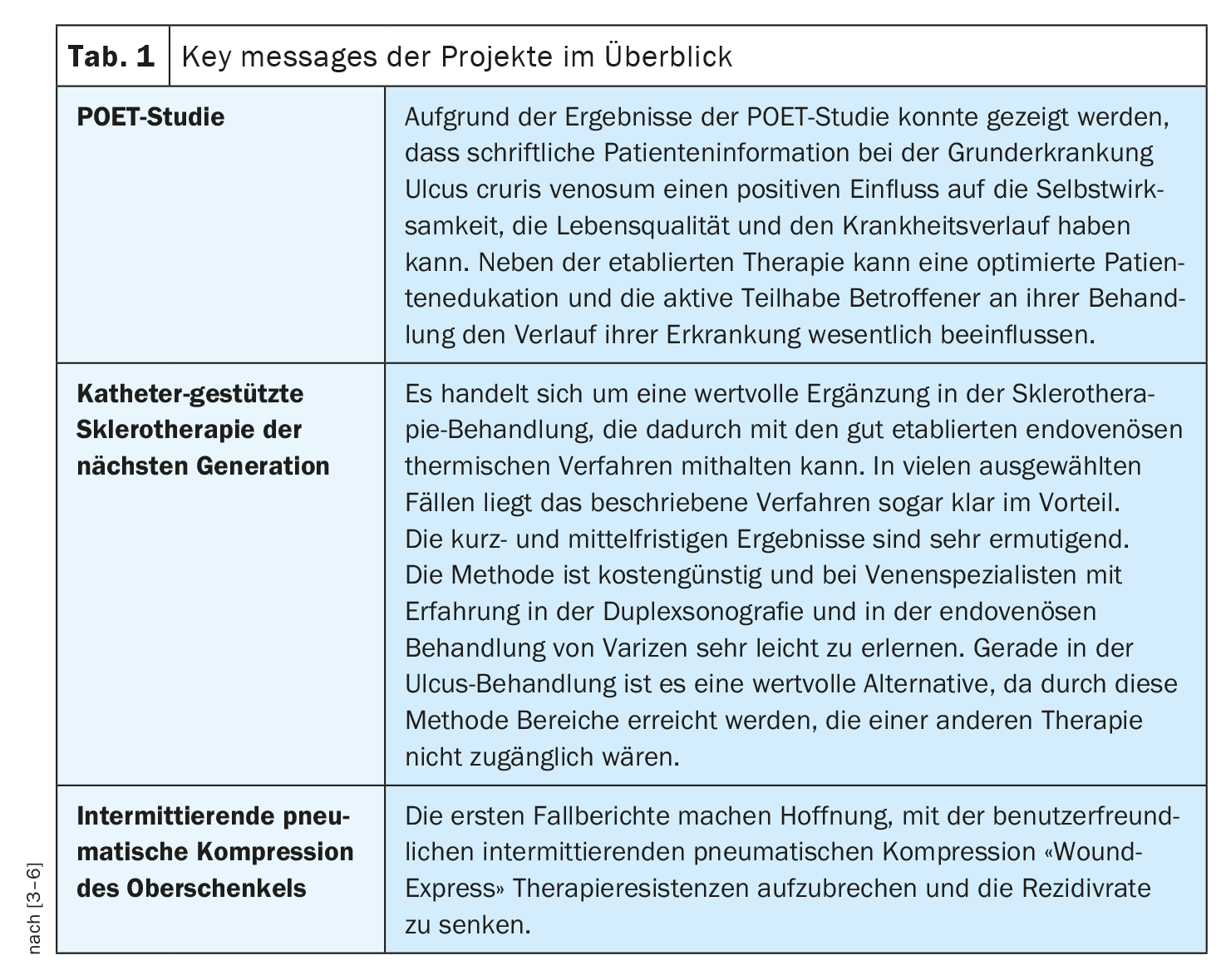
A summary of the three projects described can be found in Table 1 .
Congress: Wound Congress Nuremberg
Literature:
- Kleinhans M, Stoffels I, Dissemond J: Long-term healing of a venous leg ulcer refractory to therapy after crural fasciectomy and split-thickness skin grafting [Long-term healing of a therapy-refractory venous leg ulcer after crural fasciectomy and split skin graft transplantation]. Dermatologist 2021; 72(2): 157-162.
- Strohal R, et al: Expert recommendation for a treatment pathway for venous leg ulcers. Wound management 2021; 15(2): 58-61.
- Schutt A, Zschieschang B, Erfurt-Berge C: Influence of comprehensive patient information on disease management in venous leg ulcers, poster presentation, P11, Wundkongress Nürnberg, 23-24.11.2024.
- Schutt A, Zschieschang B, Erfurt-Berge C: Optimized education and participatory therapy of venous leg ulcers – the POET project. Wound management 2022; 16: 38-39.
- Apostolidis S: The next generation of catheter-based sclerotherapy – initial medium-term results and the contribution to modern ulcer therapy, Free lectures, FV09, Wundkongress Nürnberg, 23-24.11.2024.
- Deter K, Reader M, Haink M, Lahmann N: Intermittent pneumatic compression (IPC) of the thigh with a new device called WoundExpress (WE) for the treatment of venous leg ulcers (UCV), Free lectures, FV04, Wundkongress Nürnberg, 23-24.11.2024.
HAUSARZT PRAXIS 2024; 19(2): 41-42 (published on 20.2.24, ahead of print)