The only chance of long-term survival in pancreatic cancer is radical resection (R0) with adjuvant chemotherapy. To achieve radical resection, extended surgery with resection of the venous porto-mesenteric vessels as well as adjacent organs (multivisceral resections) has been established with good perioperative and oncologic outcomes. Resection of arterial vessels cannot be recommended in principle, but is technically possible in individual cases. In cases of local inoperability due to arterial vascular infiltration, neoadjuvant (radio)chemotherapy is performed. This achieves resectability in one-third of patients. Isolated local recurrences can be resected again with good outcome in individual cases.
Pancreatic cancer is the fourth leading cause of death from cancer. Radical surgery followed by adjuvant chemotherapy is the only option that can achieve long-term survival of 25-30%, and up to 60% at five years in subpopulations with favorable risk profiles [1,2]. Close interdisciplinary collaboration is necessary to achieve optimal outcomes for pancreatic cancer patients undergoing surgery. To assess resectability with the goal of an R0 situation, the extent of the tumor, infiltration of surrounding organs, involvement of arteries and veins, and exclusion of organ metastases are crucial for the surgeon. The appropriate assessment is usually performed preoperatively using CT or MRI images.
Operable or non-operable?
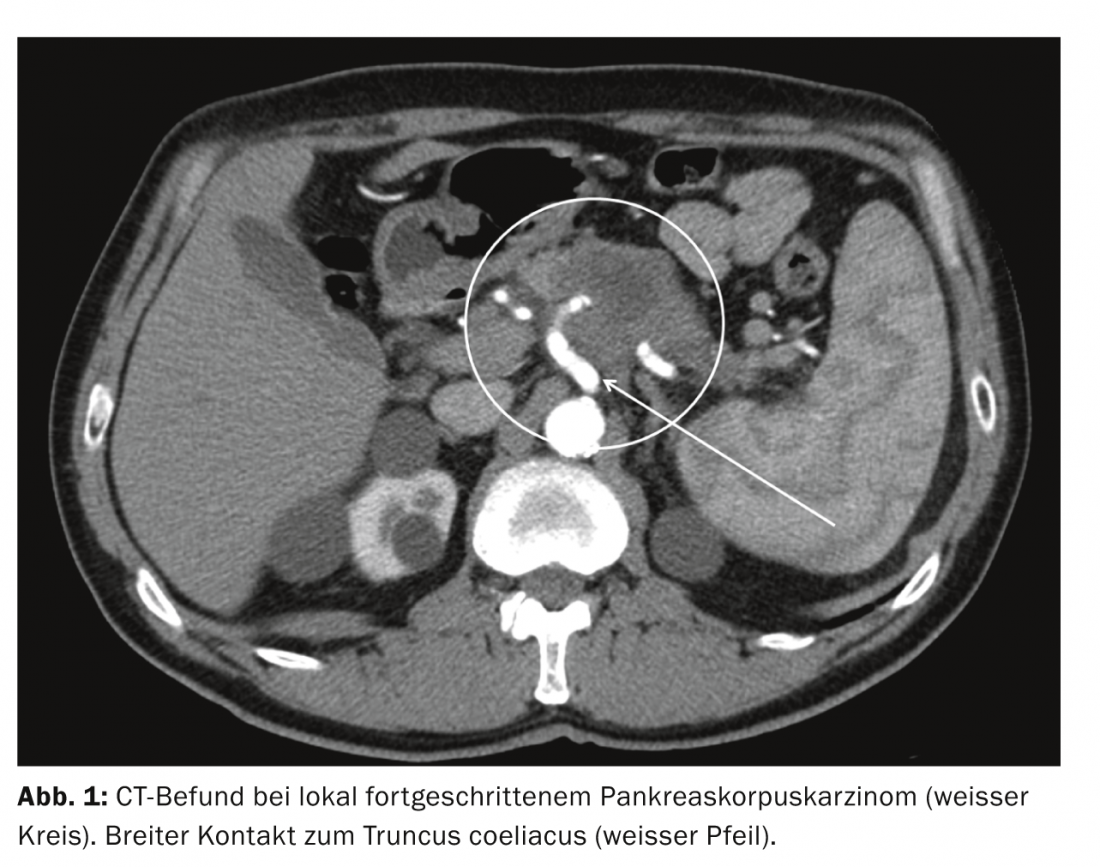
Local operability depends primarily on the extent to which large vessels are reached by the tumor: Pancreatic tumors that surround or infiltrate the superior mesenteric artery, the coeliac trunk, or the hepatic artery by more than 180° (T4 situation) or that extend broadly to the aorta are considered primarily inoperable. In case of tumor involvement of portal vein or superior mesenteric vein, the possibility of reanastomosis after resection should be assessed on the basis of CT images (especially distal connection to superior mesenteric vein); reanastomosis can be performed as a standard procedure if the vessel caliber is sufficient.
If CT demonstrates infiltration per continuitatem into surrounding organs such as the stomach, colon, adrenal gland, kidney, or spleen, the appropriate organ (partial) resections can be planned preoperatively. Duodenum as well as distal bile duct are removed anyway during partial pancreaticoduodenectomy.
Metastasis to local lymph nodes is not a contraindication to a resection procedure, as lymphadenectomy is routinely performed as part of oncologic resection according to the guidelines of the S3 guideline “Exocrine Pancreatic Cancer” written in 2007 and updated in 2013 [3]. For tumors in the pancreatic head, this means standard lymphadenectomy peripancreatic and periduodenal, in the lig. hepatoduodenal and on the right side of the mesenteric axis and right side of the coeliac trunk. For tumors in the corpus or tail region, left mesenteric lymphadenectomy and splenectomy are performed.
Primary local inoperability and neoadjuvant therapy.
In the case of a locally advanced pancreatic tumor with broad contact or infiltration of the large arteries (superior mesenteric artery, coeliac trunk, and hepatic artery), which should therefore be considered primarily inoperable, neoadjuvant therapy is indicated (Fig. 1).
According to most protocols, daily fractionated irradiation is given up to a total dose of approximately 50 Gy, accompanied by chemotherapy with weekly gemcitabine doses. Four to six weeks after completion of radiotherapy with continued gemcitabine administration, a control CT should be used to re-evaluate operability [4,5]. In the course of exploration with the intention to resect the tumor, which is successful in about 30% of patients, there is also the possibility of intraoperative radiotherapy in some centers [4].
Alternative protocols of neoadjuvant therapy are center-dependent, such as the FOLFIRINOX regimen, and are performed in trials. To date, there are no valid data on how many patients achieve resectability after completion of this therapy.
Surgical therapy: advanced surgical procedures and options.
Partial pancreaticoduodenectomy as a standard procedure for pancreatic head tumors, distal pancreatectomy (left resection) for tumors in the corpus or tail, and total pancreaticoduodenectomy for extensive tumor involvement (no preservation of part of the pancreas) can each be extended in terms of vascular and/or multivisceral resections [6]. These surgical procedures are grouped and classified as “extended resections” according to the consensus definition of the International Study Group for Pancreatic Surgery [7].
In case of involvement of the porto-mesenteric vein axis, resection of the tumor with the affected vascular segment en bloc should be attempted, if necessary – in case of long-distance vein involvement – using a vascular interposition device [8]. Perioperative morbidity from vein resection is not increased with appropriate experience, and long-term survival is comparable to procedures without the need for vascular resection, so the appropriate recommendations can be found in the interdisciplinary S3 guidelines [3].
In cases of tumor infiltration per continuitatem into neighboring organs, en bloc resection of these organs (e.g., adrenal gland or left hemicolon in pancreatic left resection) is also safely feasible if complete tumor removal can be achieved in this manner. Although there is an increased perioperative morbidity risk, mortality as well as oncologic outcome are comparable to the results of standard resections [9].
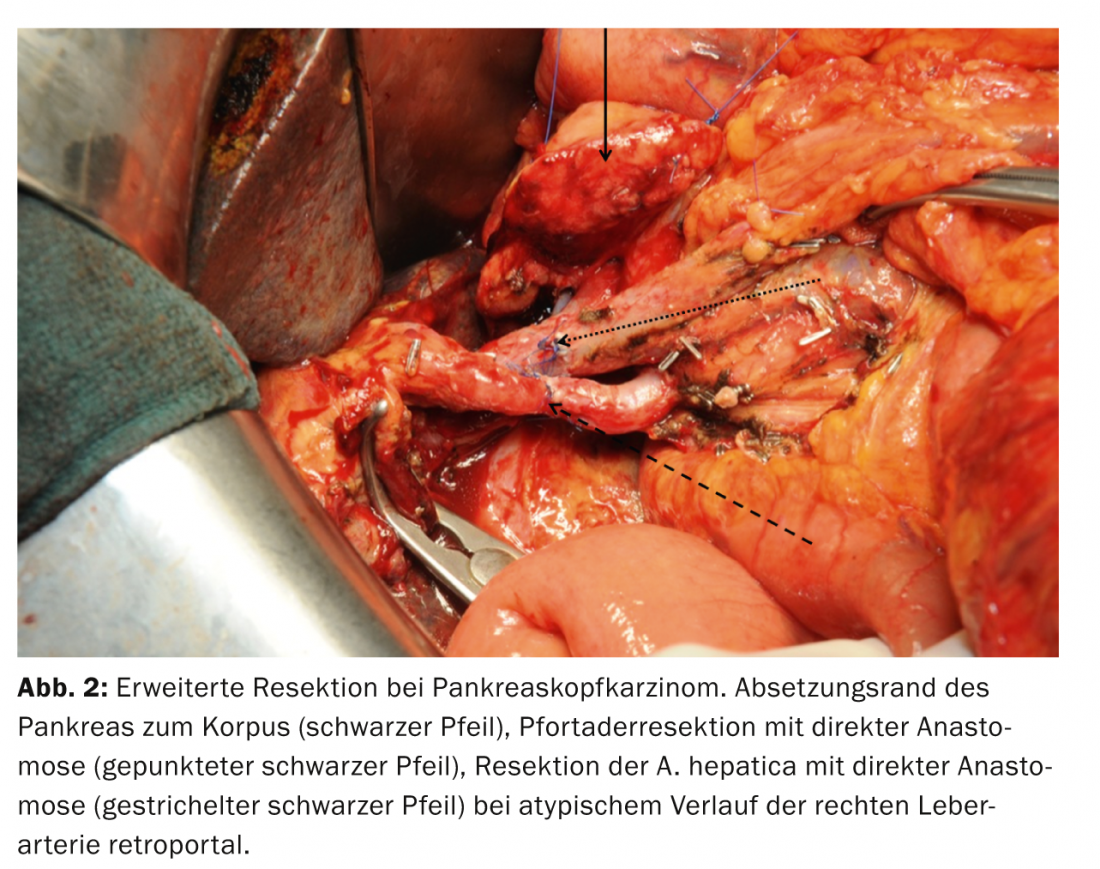
If large visceral arteries (superior mesenteric artery, coeliac trunk or hepatic artery) are infiltrated by the pancreatic tumor (T4 situation), their resection and reconstruction, for example by transposition of the lienal artery, are technically feasible in individual cases. However, these procedures are associated with significantly increased morbidity and mortality as well as poorer oncological prognosis and are therefore only considered as an option in individual cases (Fig. 2) . According to the literature and experience to date, no therapeutic advantage can be achieved by metastasis resection. Therefore, resection of metastases is not indicated in principle, even if their localization would allow resection. Surgical removal of metastases is therefore reserved for individual case decisions.
Recurrences: Importance of reoperation
After resection of pancreatic cancer, the rate of isolated local recurrence is 25-35% in large collectives. On CT, the differential diagnosis between recurrence and nonspecific postoperative soft tissue reaction is often difficult. Signposts here are – if present – rising values of tumor markers and a positive finding in the PET examination. Further tumor manifestations should be excluded in order to consider renewed surgical therapy.
Because recurrence is often localized to the major arterial vessels, accurate preoperative imaging must be obtained, preferably by CT, to plan resection. Resection is possible in up to 70% of patients; this can be combined with pre-radiation and possibly intraoperative radiotherapy as a neoadjuvant approach [10]. With a median survival of 26 months, prognosis is significantly better after surgical resection of a local recurrence than with palliative therapy alone.
Forecast
To achieve long-term survival in patients with pancreatic cancer, surgical therapy followed by adjuvant chemotherapy is the only option. Overall 5-year survival is 25-30% in large series (Table 1) .
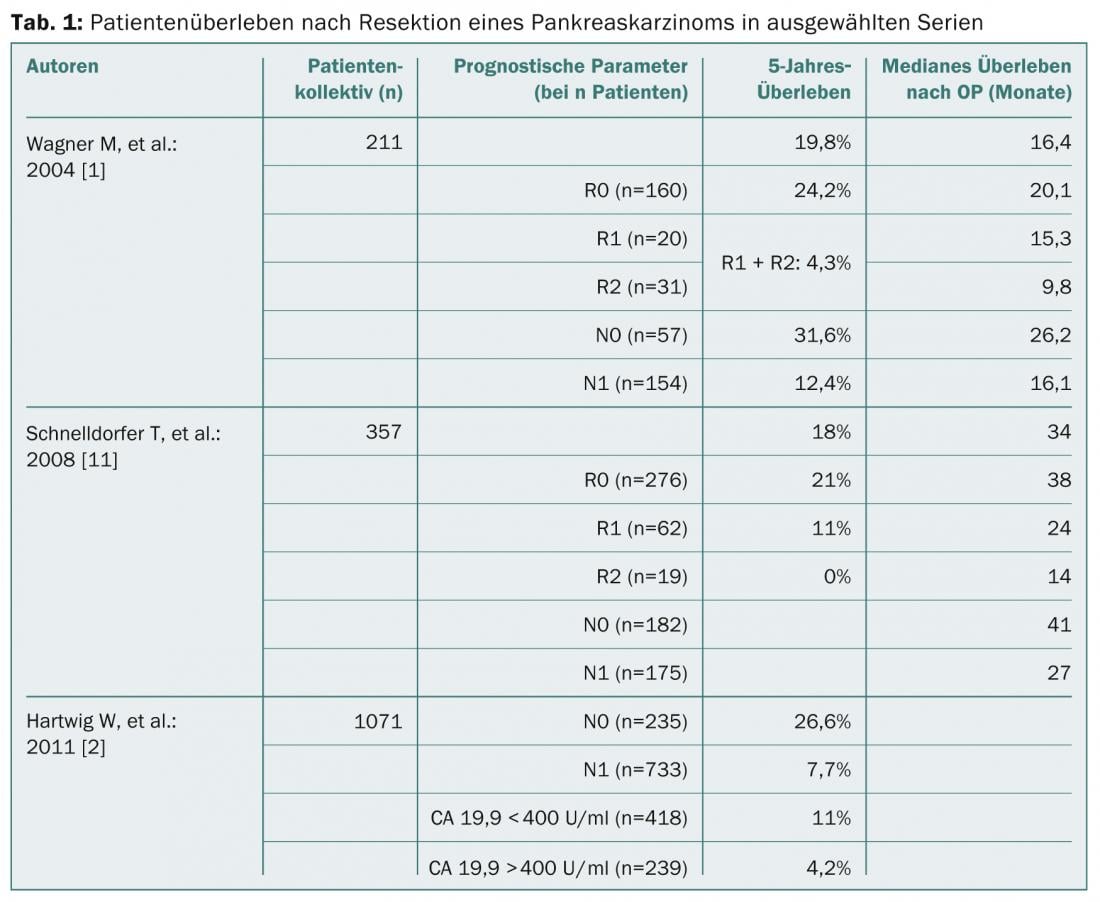
In this context, tumor removal that is as complete as possible (R0 situation) is of decisive prognostic importance. In patients who can undergo surgery, the following patient-related factors are associated with more favorable survival prognoses [2]:
- Age <70 years
- Pre-existing diabetes mellitus
- CA 19.9 preoperative <400 U/ml
- Lymph node ratio >0.2
- Tumor stage TiS, T1, T2 as well as G1.
In the corresponding subgroups with early tumor stages and without lymph node involvement, 5-year survival rates of up to 60% could be demonstrated in large patient collectives, so that especially these patients benefit from surgical therapy.
Early detection of risk constellations is therefore of particular importance, especially in the management of patients with IPMN (intraductal papillary mucinous neoplasia). IPMN are diagnosed with increasing incidence and offer the opportunity for timely resection, either while the tumor is still premalignant or at a very early stage, resulting in an excellent long-term prognosis.
Prof. Dr. med. Thilo Hackert
Prof. Dr. med. Markus W. Büchler
Literature:
- Wagner M, et al: Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004; 91: 586-594.
- Hartwig W, et al: Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg 2011; 254: 311-319.
- Seufferlein T, et al: S3-guideline exocrine pancreatic cancer. Z Gastroenterol 2013; 51: 1395-1440.
- Combs SE, et al: Prognostic Impact of CA 19-9 on Outcome after Neoadjuvant Chemoradiation in Patients with Locally Advanced Pancreatic Cancer. Ann Surg Oncol 2014; 21: 2801-2807.
- Gillen S, et al: Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med 2010; 7: e1000267.
- Hartwig W, et al: Total Pancreatectomy for Primary Pancreatic Neoplasms: Renaissance of an Unpopular Operation. Ann Surg 2014 Jun 27 [Epub ahead of print].
- Hartwig W, et al: Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery 2014; 156:1-14.
- Siriwardana H, Siriwardena A.: Systematic review of outcome of synchronous portal-superior mesenteric vein resection during pancreatectomy for cancer. Br J Surg 2006; 93: 662-673.
- Hartwig W, et al: Multivisceral resection for pancreatic malignancies: risk-analysis and long-term outcome. Ann Surg 2009; 250: 81-87.
- Strobel O, et al: Re-resection for Isolated Local Recurrence of Pancreatic Cancer is Feasible, Safe, and Associated with Encouraging Survival. Ann Surg Oncol 2013; 20: 964-972.
- Schnelldorfer T, et al: Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg 2008; 247: 456-462.
InFo Oncology & Hematology 2014; 2(7): 15-18.