In certain underlying diseases such as heart failure or chronic kidney disease, transferrin saturation and soluble transferrin receptor should be determined in addition to serum ferritin levels. Inflammation is accompanied by the increased release of hepcidin. This protein inhibits iron absorption from the intestine and the release of iron from iron stores. In addition to oral preparations, well-tolerated intravenous high-dose iron therapy preparations are available for iron substitution.
Iron is a vital trace element and plays a key role in many metabolic processes. Even a slight disturbance in the balance between absorption and loss can lead to iron deficiency [1]. Most of the iron is bound in the hemoglobin of erythrocytes, where it is responsible for oxygen transport. But it is also found in muscle cells, as storage iron, and in some enzymes. This is also the reason for the versatile symptoms with which an iron deficiency can present itself. Affected patients often suffer from fatigue, poor concentration, pallor, mouth rhagades and hair loss [1]. Iron deficiency is mostly caused by increased iron loss or increased iron demand, less often by absorption disorders. In iron deficiency without anemia, there is a deficiency of storage iron manifested by a low concentration of ferritin. According to WHO, iron deficiency anemia is present when the hemoglobin concentration due to iron deficiency is below 12 g/dL in women and below 13 g/dL in men [2].
Iron deficiency in chronic inflammation is multifactorial in nature
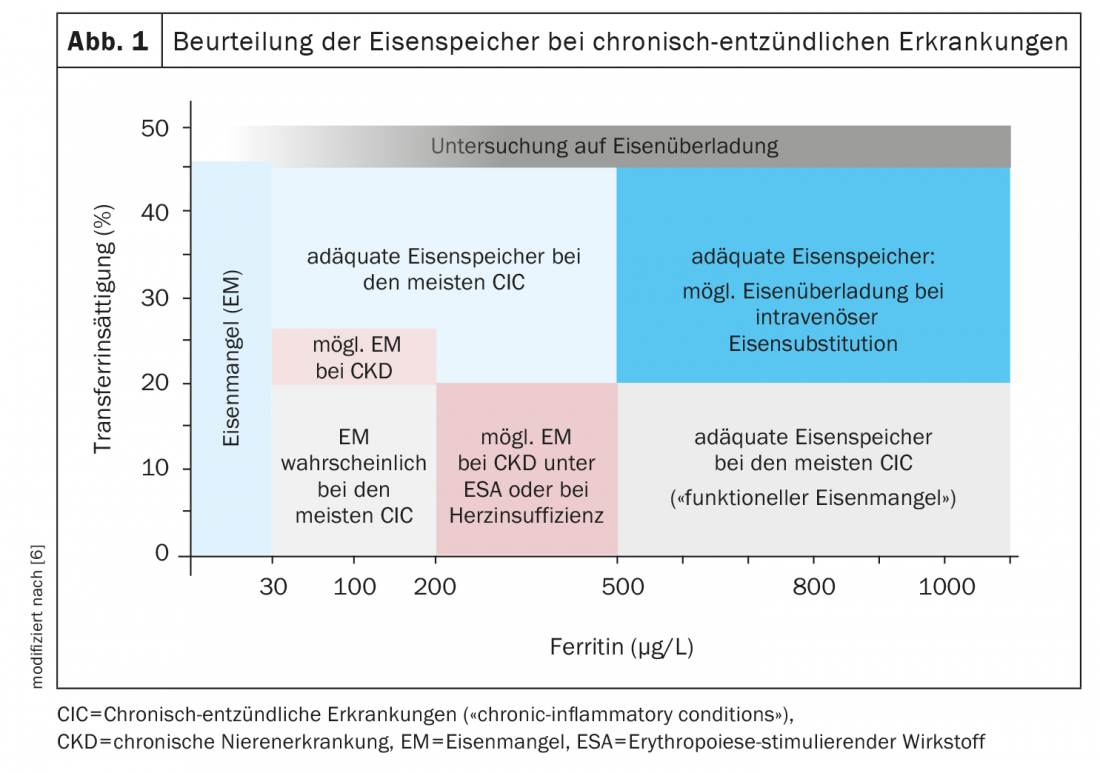
According to guidelines, patients with concomitant diseases such as chronic kidney disease, heart failure, or chronic inflammatory bowel disease may be iron deficient at ferritin levels as low as 500 μg/L [5,6] (Fig. 1) . However, if mobilization of iron stores is impaired, iron-deficient erythropoiesis may result despite adequate iron stores. This functional iron deficiency is typical of inflammatory anemia [8]. Chronic inflammation leads to upregulation of hepcidin in the liver, which binds to ferroportin [3]. Enterocytes are prevented from exporting absorbed iron into the bloodstream. In hepatocytes and macrophages, iron is also bound intracellularly and stored as iron-rich ferritin, while macrophages increase iron-poor serum ferritin in the bloodstream. A high intracellular iron concentration leads to a decrease in transferrin production and thus to a decrease in total iron binding capacity. Iron release is limited, so despite the low value of total iron binding capacity, transfer saturation (TSAT) continues to decrease. “Depending on how much iron is still available in the bone marrow, an iron deficiency can develop in addition to the inflammation,” explained Prof. Jörg Halter, M.D., Senior Physician, Hematology, University Hospital Basel. Iron restriction eventually leads to anemia. As is now known, chronic inflammatory anemias are multifactorial and often difficult to understand in individual cases, said the speaker [3]. Most patients with chronic inflammation associated with iron deficiency have a TSAT<20% and ferritin levels <200 μg/L, but in individual cases iron supplementation may be indicated even at higher levels [6].
Hepcidin inhibits the iron transporter ferroportin
Serum ferritin concentration reflects intracellular ferritin concentration. In iron deficiency, serum ferritin is below the age norm. However, in systemic inflammatory reactions, the sole determination of serum ferritin concentration is not a reliable parameter for the diagnosis of iron deficiency. In these cases, other parameters should be consulted, explained Prof. Halter [3]. Soluble transferrin receptor concentration, together with serum ferritin concentration, independently of concomitant diseases, reflects iron status and is elevated in iron deficiency. In iron deficiency, more transferrin receptors and less ferritin are produced in the cell, which is linked to increased iron uptake and decreased storage [4]. The protein hepcidin plays a central role in iron metabolism. It inhibits the iron transporter ferroportin and thereby both intestinal iron absorption and iron release from the reticuloendothelial system. This is because the iron transporter ferroportin is responsible for releasing the iron absorbed in the intestine into the blood, where it is bound to transferrin and then transported to the bone marrow, where the iron is incorporated. In functional iron deficiency, there is usually a sharp increase in hepcidin, which throttles iron absorption and release.
Iron substitution: oral or intravenous?
Whether iron therapy is given orally or intravenously is an individual decision. Intravenous iron supplementation may be particularly useful when oral iron is not tolerated or is insufficiently absorbed, as well as in pregnant women, chronic inflammatory bowel disease, or chronic kidney disease [2,7]. Among oral preparations, those with bivalent iron are better utilized than those with trivalent iron. Iron tablets should be taken 30 minutes before or 2 hours after food and not with dairy products. The duration of use is variable, with a recommended minimum of three months beyond correction of the anemia, or permanently if necessary in the case of chronic blood loss. “Intravenous iron substitution is an alternative, especially if iron absorption disorders exist,” Prof. Halter said. The most commonly used are carboxymaltose (Ferinject®) and ferric isomaltose (Monofer®). Based on the determined iron requirement, the individually adequate dose is administered. Anaphylactic reactions are extremely rare nowadays, the speaker said.
Congress: medArt
Literature:
- Iron deficiency anemia, S1 guideline, AWMF guideline 025/021. www.awmf.org/uploads, (last accessed Aug. 30, 2022)
- Chmiel C, Beise U: Iron deficiency, last revised: 07/2022, www.medix.ch, (last accessed Aug 30, 2022).
- “Anemia,” Prof. Jörg Halter, MD, medArt June 20-24, 2022.
- Warnck C: Iron substitution. To be noted, www.pharmazeutische-zeitung.de/spurenelement-mit-schluesselfunktion-119643/seite/alle, (last accessed Aug. 30, 2022).
- Cappellini MD, et al; IRON CORE Group. Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management. Am J Hematol 2017; 92(10): 1068-1078.
- Fertrin KY: Diagnosis and management of iron deficiency in chronic inflammatory conditions (CIC): is too little iron making your patient sick? Hematology Am Soc Hematol Educ Program 2020; 2020(1): 478-486.
- Auerbach M: Treatment of iron deficiency anemia in adults UpToDate, www.uptodate.com, (last accessed Aug. 30, 2022).
- Jimenez K, Lang M: Algorithm for the diagnosis of iron deficiency anemia. Wien Med Wochenschr 2016; 166: 402-410.
HAUSARZT PRAXIS 2022; 17(9): 24-25