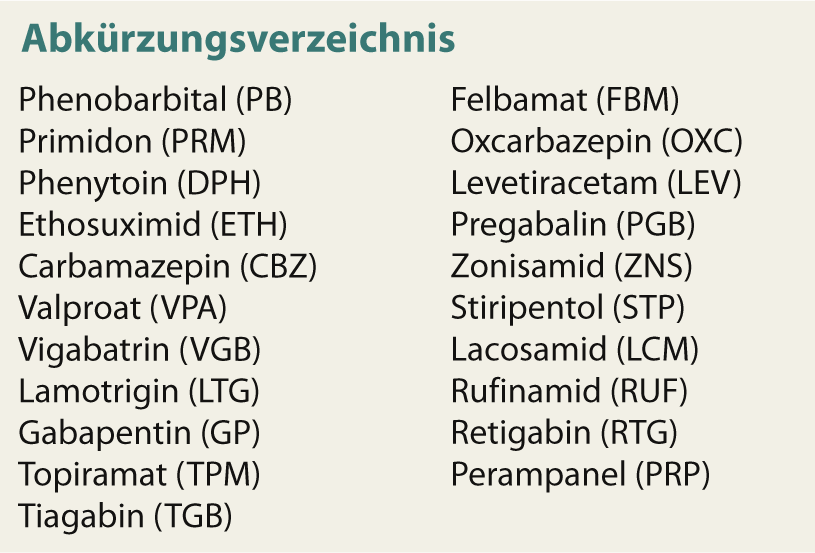
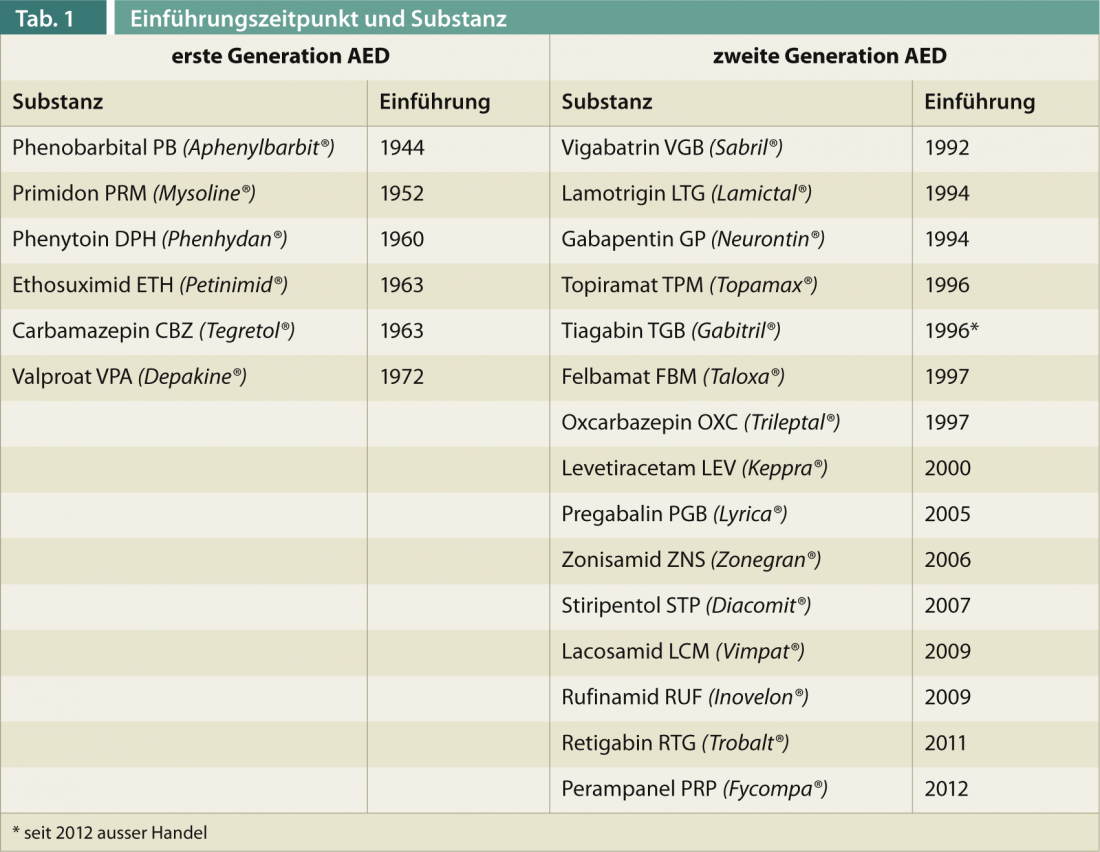
The first-generation antiepileptic drugs (AEDs) (Table 1) – valproate was last approved in Switzerland in 1972 – are characterized by complex pharmacokinetics. In particular, the induction and inhibition of hepatic enzymes, especially of the cytochrome P type, results in potentially relevant drug-drug interactions with risk of loss of efficacy and undesirable overdoses with medication changes. Furthermore, the spectrum of side effects, especially in terms of chronic effects (osteoporosis, polyneuropathy, cerebellar atrophy, etc.), is sometimes serious. Second-generation AEDs have entered the pharmacotherapy of epilepsy since the 1990s. They differ from the above mainly in fewer side effects and better pharmacokinetics, but not in significantly better efficacy. Contrary to initial hopes, they, like the old AEDs, have no antiepileptogenic effect, i.e., they have no proven effect on epilepsy as a disease and continue to act only symptomatically to prevent seizures.
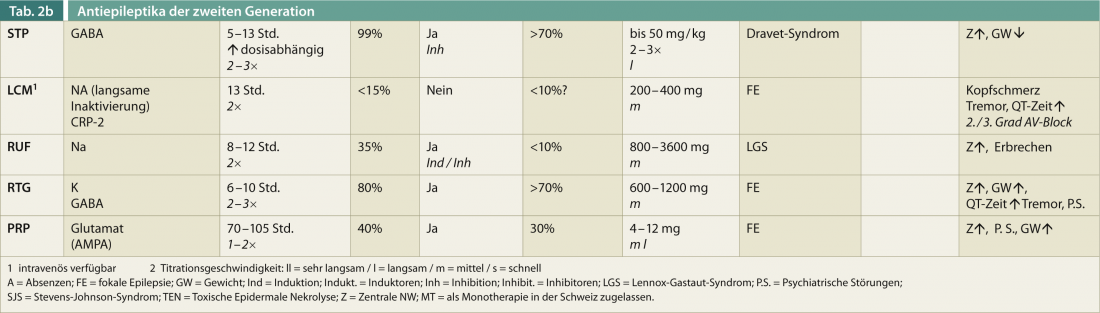
The drugs approved in the last five to ten years are characterized in particular by their specific effect on specific epilepsy syndromes in the sense of orphan drugs (RUF and FBM act on Lennox-Gastaut syndrome, STP on Dravet syndrome). In the opinion of the authors, however, they should not be classified as third-generation drugs because, based on the evidence to date, they do not differ in any relevant way from second-generation drugs in terms of their spectrum of action, side effects, or interactions. Their use in therapy-resistant epilepsies, after failure of other add-on medications, can be useful, as in some cases other mechanisms of action are present.
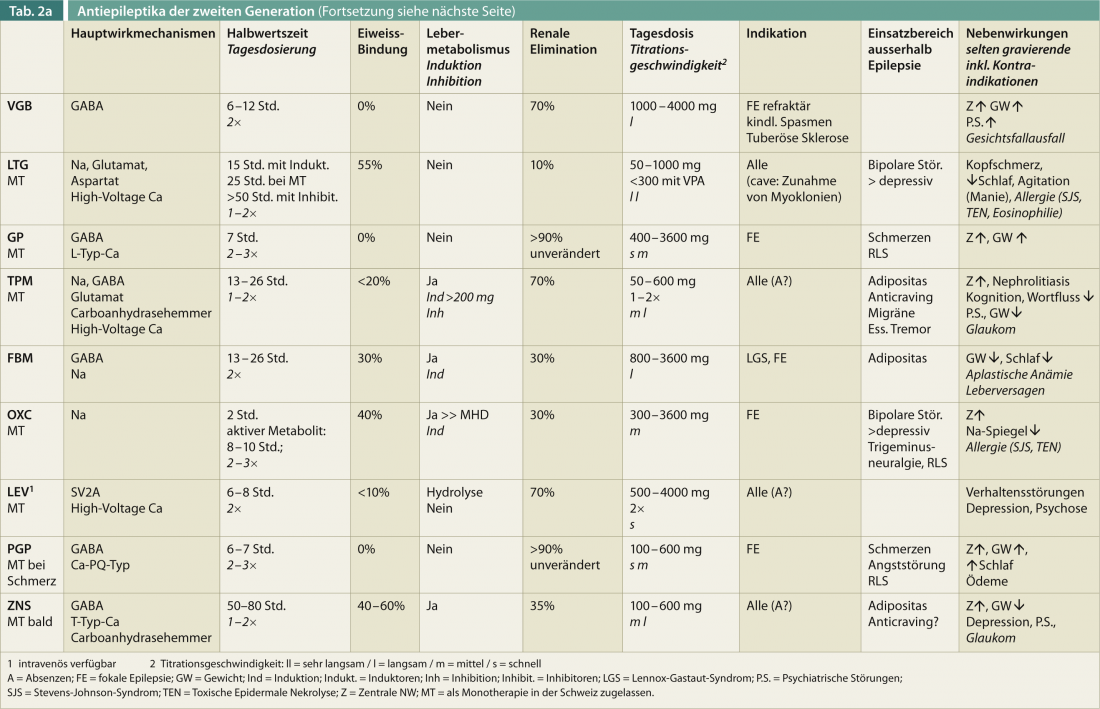
An overview of therapy-relevant properties of second-generation AEDs (without claim to completeness) should help to quickly orient oneself (Tab. 2). Age, gender, comedication, and positive effect on other diseases are essential factors for the optimal choice of an antiepileptic drug.
In the following article, benzodiazepines that target the GABA-A receptor, such as clonazepam (Rivotril®), clobazam (Urbanyl®), lorazepam (Temesta®), and midazolam (off-label in Switzerland, e.g., as a nasal spray), are not discussed. In addition to sedation – especially at the beginning – they more often show development of tolerance, sometimes also loss of effect. They are indicated primarily as emergency medications and for predictable seizure episodes (infection, menstruation, etc.) and when AEDs are switched or introduced.
Old and new mechanisms of action of anticonvulsant medication.
Known typical mechanisms of action of antiepileptic drugs include blockade of voltage-gated fast sodium channels and various calcium channels, enhancement of the inhibitory GABA effect by inhibition of degradation and reuptake or by a direct attack on gaba receptors, and reduction of synaptic glutamate action. The effects of second-generation AEDs are based in part on the same pharmacodynamic targets, but there are also differences. Thus, PRP reduces the release of the activating neurotransmitter glutamate; in contrast to older drugs, a new site of action with non-competitive pharmacodynamics at receptors is described here. LCM modulates cellular Na channels, but a specific subtype that shows longer channel opening times. Novel mechanisms of action, e.g., in LEV, include modulation of a vesicle protein (SV2) or CRP2 in LCM. In general, it is favorable to combine AEDs with different mechanisms of action. Combinations of AEDs with the same mechanism of action, especially sodium channel blockers, can lead to increased intoxications. In generalized epilepsies, it must be remembered that specific seizure types may increase and even new seizure types may occur with effects on GABA and at the sodium channel. A pharmacodynamically synergistic and effective combination therapy is that of VPA and LTG, although pharmacokinetic considerations must be taken into account here (see below).
As epileptic seizures are increasingly understood as a “network dysfunction,” targets and modes of action of AEDs will need to be reassessed in the future.
Pharmacokinetics usually less problematic
In principle, second-generation AEDs show less interaction with enzyme systems and concomitant drugs. Thus, protein binding is usually lower and the free, non-protein-bound AED fraction may play a role, especially with older substances such as DPH, and may need to be determined on a case-by-case basis. It should be noted that AEDs with weak enzyme induction such as OXC, RUF, FBM, and TPM (only at doses above 200 mg) may also attenuate the effect of hormonal contraception. Furthermore, lamotrigine levels may decrease significantly, i.e., up to more than 50%, under hormonal contraception with estrogens as well as during pregnancy. Mirror checks are indispensable here.
The inhibitory effects of concomitant VPA medication must also be considered with the new AEDs, where LTG levels may increase significantly in addition to the known increase in carbamazepine epoxide (metabolite of CBZ). Slight increases are also possible for LEV, PRP, RUF, RTG and FBM. For other drugs such as TPM and CNS, the impact is not clear. It should be borne in mind that intoxication and diminution of antiepileptic effect may also occur with second-generation AEDs when an enzyme inhibitory or enzyme inducing concomitant medication is changed. Especially in the case of enzyme inducers, the effects can still occur with latencies of several weeks. It should also be noted that the steady state for dose changes usually occurs after five half-lives.
Almost all AEDs have a linear uptake mechanism, i.e., increasing drug doses cause the blood serum concentration of the drug to increase by a factor of the dose amount. Exceptions include the exponential increase in DPH, non-linearly decreased absorption of VPA at higher doses, and saturable absorption of GP and CNS at higher doses. PRP is absorbed with a slight delay with food intake, i.e. the temporal relationship of food intake and drug intake should always be the same.
AEDs are usually taken 2×/day; GP, RTG, and the non-retarded OXC usually need to be divided into three daily doses. CNS, PRP, and in some cases low-dose monotherapies with LTG and TPM are available as single doses. Regarding daily doses, it should be kept in mind that the total dose (especially for LTG) and the number of doses should be determined depending on the combination with enzyme inhibitors or enzyme inducers.
Side effects usually less serious
More than 20% of patients discontinue antiepileptic therapy because of side effects, which are most often central in nature (fatigue, gait ataxia, double vision). Faster titration is usually somewhat better with LEV than with VPA. Approximately one-third of patients remain refractory to AED therapy because of repeated adverse events. In summary, almost 90% experience some side effect, which may be more or less severe. In Table 2, selectively relevant side effects of second-generation AEDs are presented without claiming to be complete.
The new AEDs appear to have a relatively low teratogenicity risk (only up to 12 weeks gestation). However, the overall case numbers are quite low in this regard; with the most data available for LEV – best profile in this regard – and LTG. VPA and polytherapies have the highest teratogenicity. Valproate may also tend to have a negative impact on the cognitive development of children born to valproate-taking mothers.
AED and age
For epilepsy therapy in the elderly, it should be considered that levetiracetam is the most suitable due to its pharmacological profile and few interactions, also because of its relatively low central side effects and cognitive impairment. Furthermore, the use of gabapentin and lamotrigine is reasonable, especially when behavioral disturbances or psychiatric comorbidities potentially accentuated by LEV are present. With LTG, the slow onset time must be taken into account, and the addition of a benzodiazepine (e.g., clobazam) may therefore be useful.
Indications of the AED
The indications for AEDs have been established on the basis of available studies for focal and generalized epilepsies and for specific syndromes and have been granted by the competent authorities. It should be noted that certain medications that act primarily on focal seizures-such as VGB, GP, PGB, LCM-can theoretically worsen generalized epilepsies. Accentuation of myoclonia in generalized epilepsy is possible under LTG.
According to various guidelines, VPA, followed by TPM and LTG, are first-line agents for idiopathic generalized epilepsies. Partly good experiences are also made with LEV and CNS. The use of VPA – although the most potent agent in idiopathic generalized epilepsies with generalized tonic-clonic seizures, absences (comparable to ETH), and myoclonic seizures – should always be critically questioned in women of childbearing potential (see below).
No such significant differences in efficacy among AEDs are available for focal seizures, including those with secondary generalization.LTG or LEV is recommended as the first-line agent for focal epilepsies. It is also possible to use OXC, TPM, VPA, GP, PGB and CNS. Instead of reintroducing CBZ – in Switzerland, genetic testing HLA-B*15:02 is recommended because of allergenic potency (positive in about 10-15% in Asians; <2% in white population) – OXC should also be used in slightly higher incidence of hyponatremia.
The multitude of AEDs has also been partially studied systematically with regard to effects on concomitant diseases. These comorbidities should always be considered when selecting an AED (Table 2) and contribute significantly to the treatment decision.
Individual adjustment of medication central
With more than 20 AEDs available, it should be noted that the individual choice of the optimal medication has become even more important. Thus, age, the medical and social situation, and comorbidities of our patients must always be taken into account, in addition to the type of epilepsy . Knowledge of side effects in negative and concomitant effects in positive terms should complement pharmacokinetic considerations. Patients with a high seizure frequency at the onset of epilepsy and a symptomatic etiology are at higher risk of not being controlled with medication. In cases of therapy resistance, epilepsy surgery should be considered after two years of unsuccessful therapy with two antiepileptic drugs. Overall, however, nearly two-thirds of patients (50% with the first AED plus 9% with the second) become seizure-free with generally few acute and long-term side effects.
Klaus Meyer, MD
Martinus Hauf, MD
Literature:
- Brodie MJ, Barry SJ, et al: Western Infirmary, Glasgow. Comment in Neurology 2012 May 15; 78(20): 1542-1543.
- Glauser T, Ben-Menachem E, et al: Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia 2013; 54(3): 551-563.
- Marson AG, Al-Kharusi AM, et al: The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomized controlled trial. Lancet 2007; 369(9566): 1000-1015.
- Marson AG, Al-Kharusi AM, et al: The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalized and unclassifiable epilepsy: an unblinded randomized controlled trial. Lancet 2007; 369(9566): 1016-1026.
- Costa J, Fareleira F, et al: Clinical comparability of the new antiepileptic drugs in refractory partial epilepsy: A systematic review and meta-analysis. Epilepsia 2011; 52(7): 1280-1291.
- Perucca E, Tomson T: The pharmacological treatment of epilepsy in adults. Lancet Neurol 2011; 10: 446-456.











