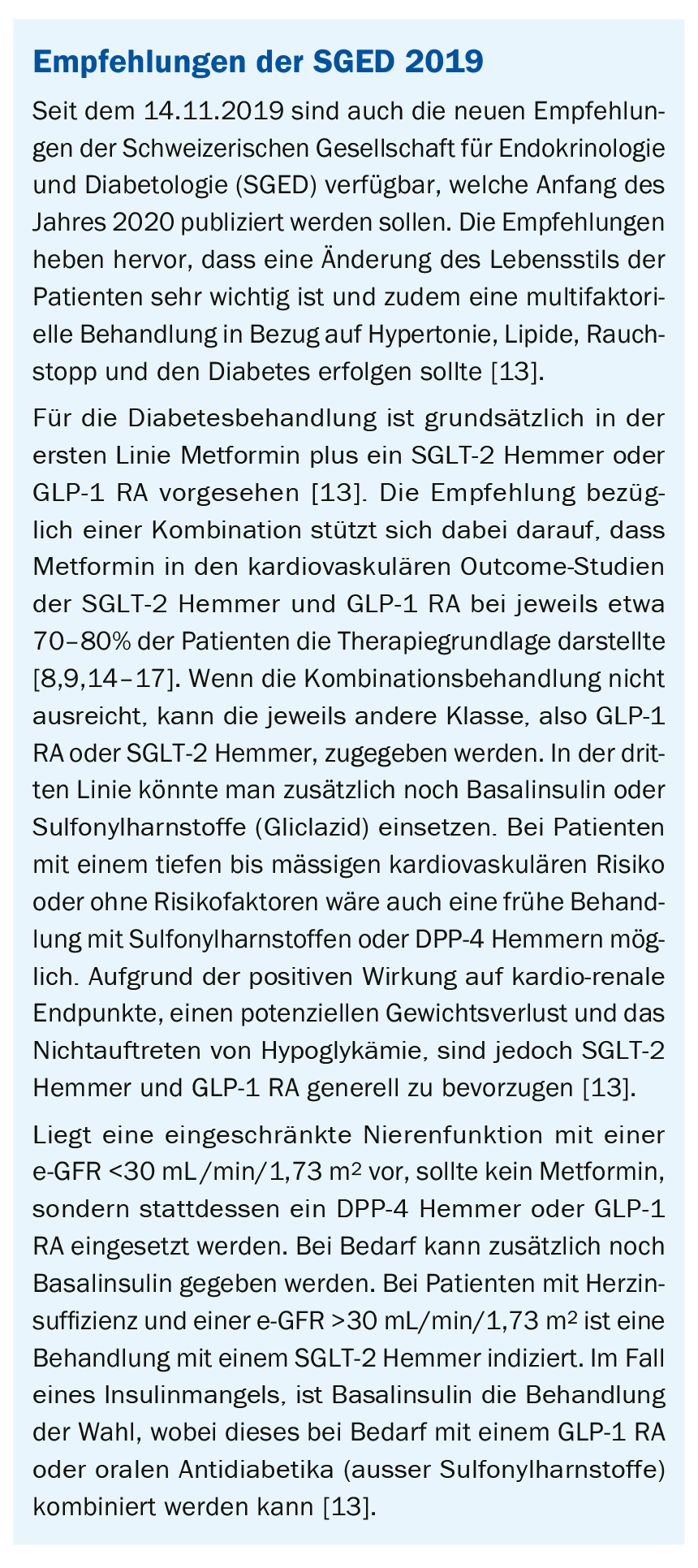
Type 2 diabetes is associated with an increased risk of both cardiovascular events and the development of chronic kidney disease. These aspects are therefore increasingly finding their way into current recommendations for diabetes treatment. The most important innovations of the ESC and ERA-EDTA Guidelines 2019 are presented below.
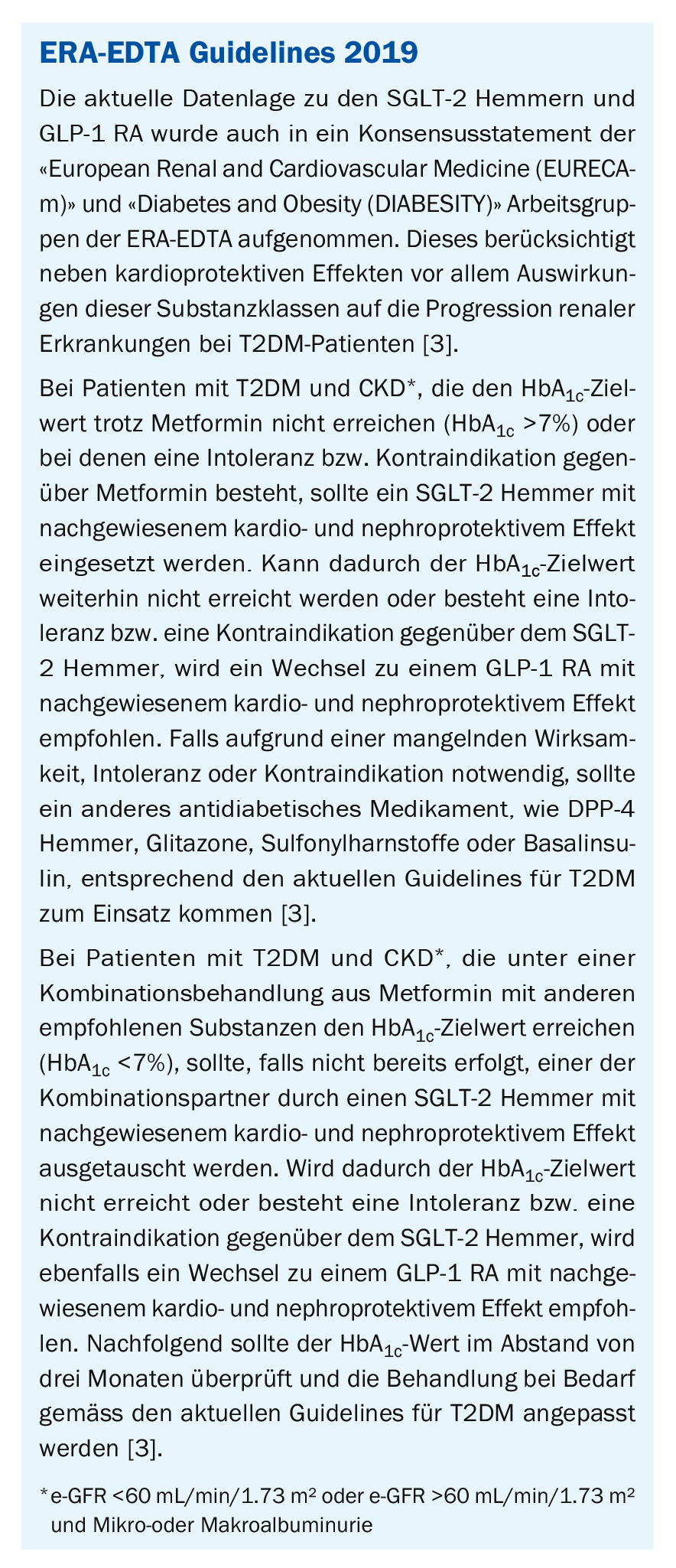
The combination of diabetes, chronic kidney disease (CKD), hypertension, and dyslipidemia contributes significantly to the development of cardiovascular disease [1]. For this reason, the current European Society of Cardiology (ESC) guidelines take into account new data from clinical trials on the management of these aspects [1]. The following is a summary of the most important new features of the 2019 ESC guidelines focusing on cardiovascular and renal risks in type 2 diabetes mellitus (T2DM) [2]. In addition, a brief update is provided on a recent consensus statement from the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) regarding the nephro- and cardioprotective properties of sodium-dependent glucose transporter-2 (“SGLT-2”) inhibitors and glucagon-like peptide-1 (“GLP-1 RA”) receptor agonists [3].
Cardiovascular risk assessment in patients with diabetes.
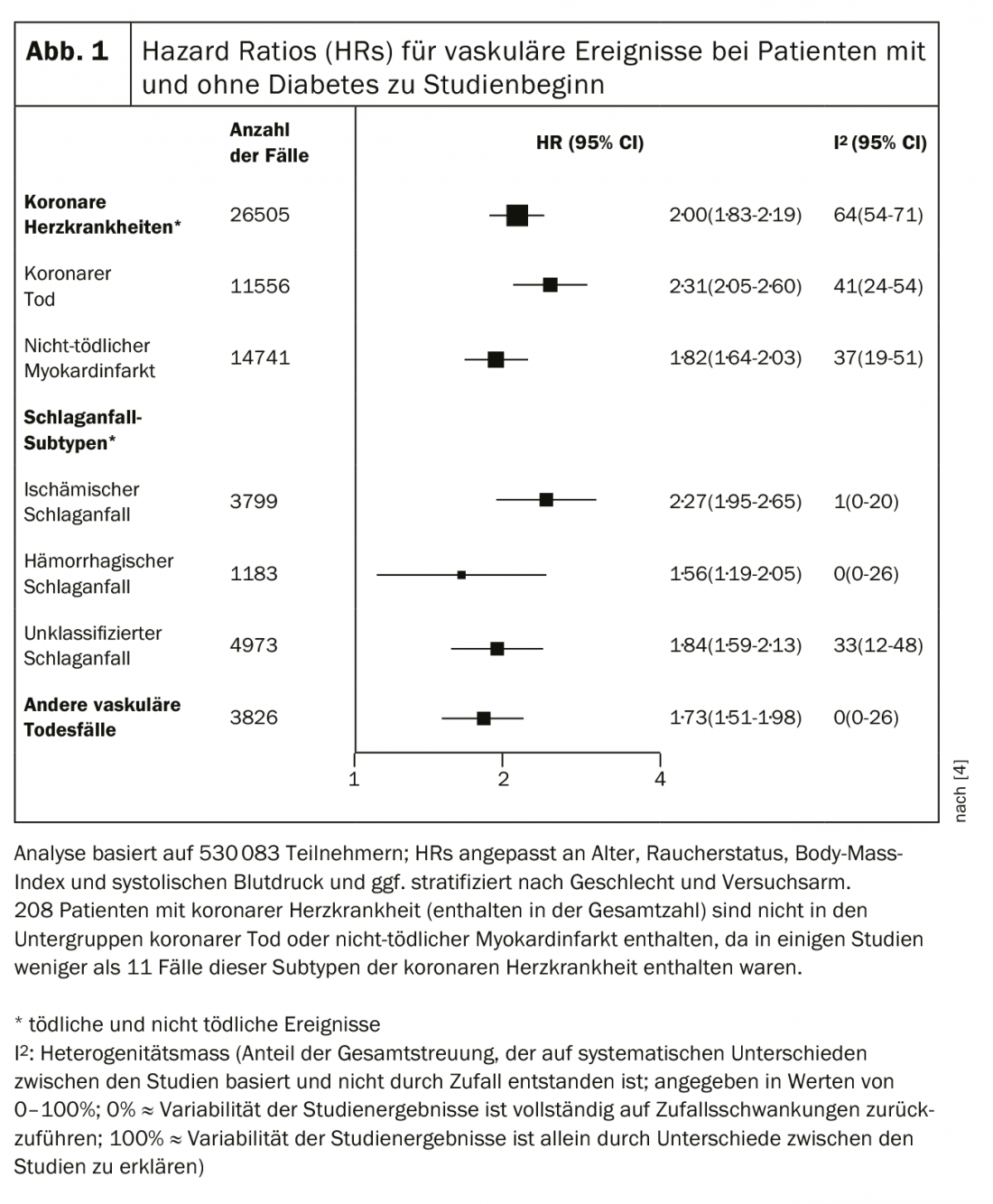
The risk of cardiovascular disease is clearly related to the duration of diabetes and the presence of comorbidities, including CKD and other cardiovascular risk factors [1]. According to the Emerging Risk Factor Collaboration, a meta-analysis of 102 prospective studies, patients with diabetes have twice the risk of vascular events (coronary heart disease, ischemic stroke, and vascular death), independent of other risk factors (Fig. 1) [4]. In this context, both the relative and absolute risk of vascular events are increased in the presence of long-standing diabetes or microvascular complications, including renal disease or proteinuria [2].
Age at onset of diabetes also plays an important role. Data from the Swedish National Diabetes Registry show that this is an important prognostic factor for survival and cardiovascular risk in type 1 and type 2 diabetes [5,6]. In this regard, diagnosis of T2DM at a young age is associated with the greatest loss of life years, which in turn argues for intensive risk factor management [2,6].
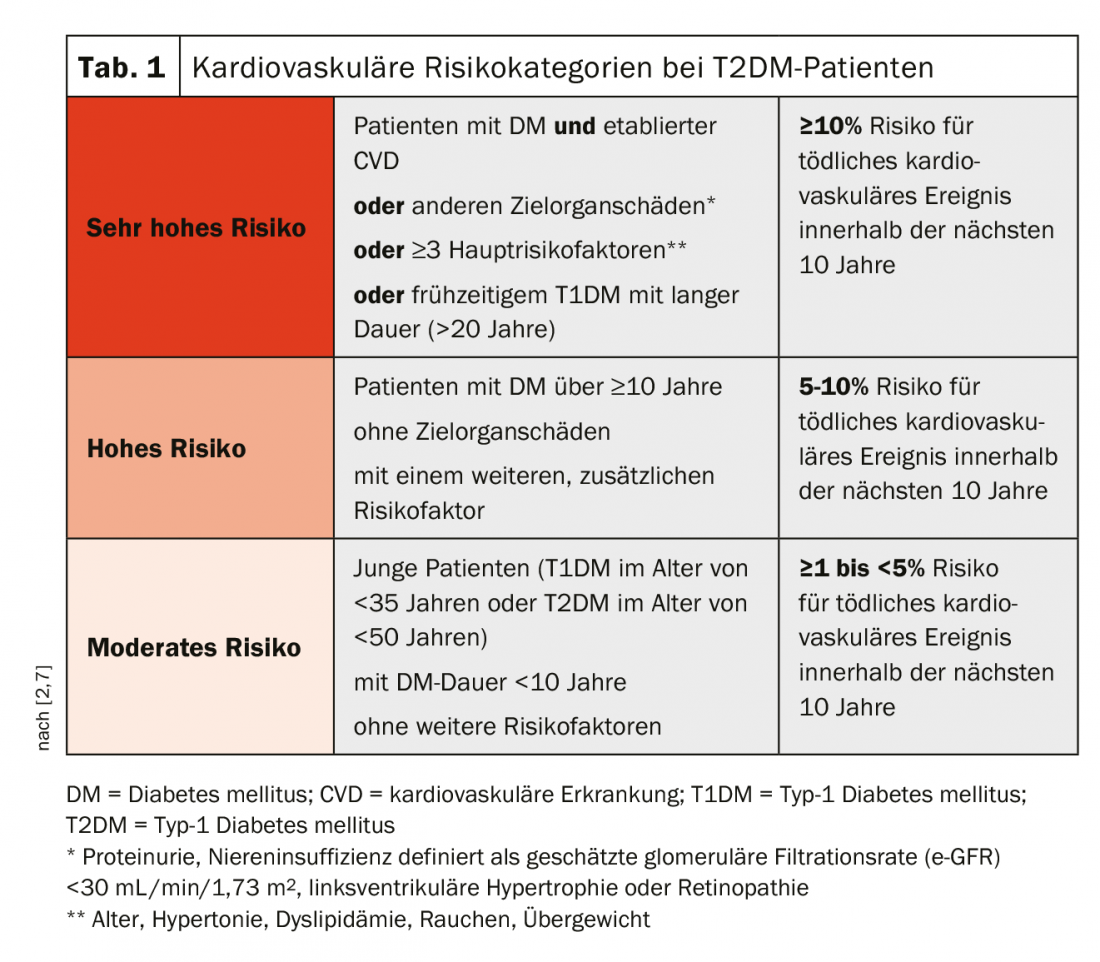
To address these aspects accordingly, new cardiovascular risk categories – moderate, high, and very high risk – have been introduced in the current ESC Guidelines, focusing mainly on the duration of diabetes and the presence of risk factors (Table 1) [2].
Clinical evaluation of cardiovascular injury.
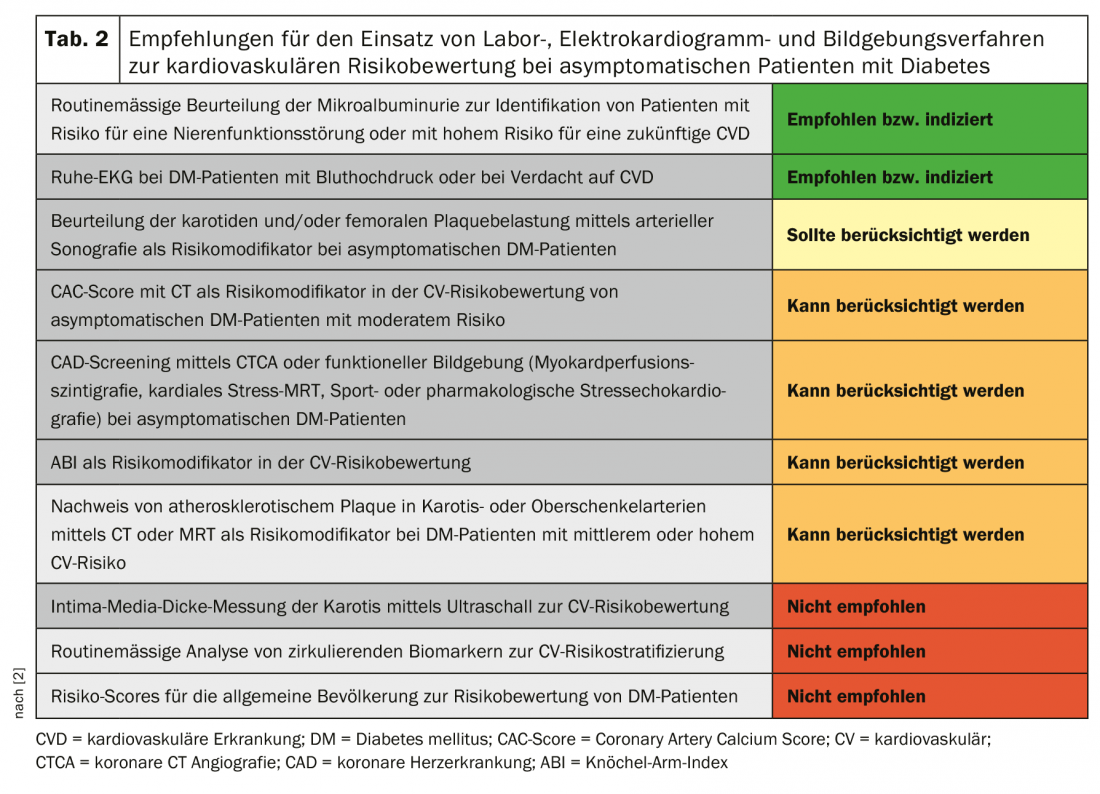
With regard to the clinical evaluation of cardiovascular injury, some innovations have also been made in the current ESC guidelines. In particular, new recommendations on the assessment of atherosclerosis by imaging techniques have been added. A summary of all recommendations regarding laboratory, electrocardiogram, and imaging techniques for cardiovascular risk assessment is provided in Table 2, with changes from the 2013 ESC guidelines highlighted in each case [2].
Glucose-lowering treatment for cardiovascular disease prevention.
In recent years, a large number of cardiovascular outcome studies have been published, particularly regarding the use of dipeptidyl peptidase-4 (DPP-4) inhibitors, SGLT-2 inhibitors, and GLP-1 RA. Here, the DDP-4 inhibitors showed cardiovascular safety (with the exception of saxagliptin, which was associated with an increased risk of hospitalization for heart failure) but no cardiovascular benefit. In contrast, the GLP-1 RA liraglutide, semaglutide, and dulaglutide and the SGLT-2 inhibitors empagliflozin, canagliflozin, and dapagliflozin were additionally shown to have cardiovascular benefits [1]. Among them, only empagliflozin and liraglutide were associated with a significant reduction in the risk of cardiovascular death [8,9]. Based on these data, new treatment recommendations for the use of glucose-lowering agents to prevent cardiovascular disease were presented in the current ESC guidelines [2].
In contrast to the previous version of the 2013 ESC guidelines, metformin is now no longer recommended as first-line treatment in all DM patients. Instead, it should be used only in overweight T2DM patients without cardiovascular disease and at moderate cardiovascular risk [2]. The recommendations are based primarily on data from the UK Prospective Diabetes Study (UKPDS), in which metformin treatment reduced the risk of myocardial infarction by 39%, coronary death by 50%, and stroke by 41% in overweight T2DM patients without cardiovascular disease over a median period of 10.7 years [2,10].
Instead of metformin, the use of the SGLT-2 inhibitors empagliflozin, canagliflozin, or dapagliflozin and the GLP-1 RA liraglutide, semaglutide, or dulaglutide to reduce the risk of cardiovascular events is now recommended in the first-line treatment of T2DM patients at high or very high cardiovascular risk. Only empagliflozin or liraglutide are indicated to reduce the risk of cardiovascular death [2].
According to these adapted recommendations, new treatment algorithms were developed. An overview for patients with T2DM and atherosclerotic cardiovascular disease (ASCVD) or high or very high cardiovascular risk can be found in Figure 2 [2].
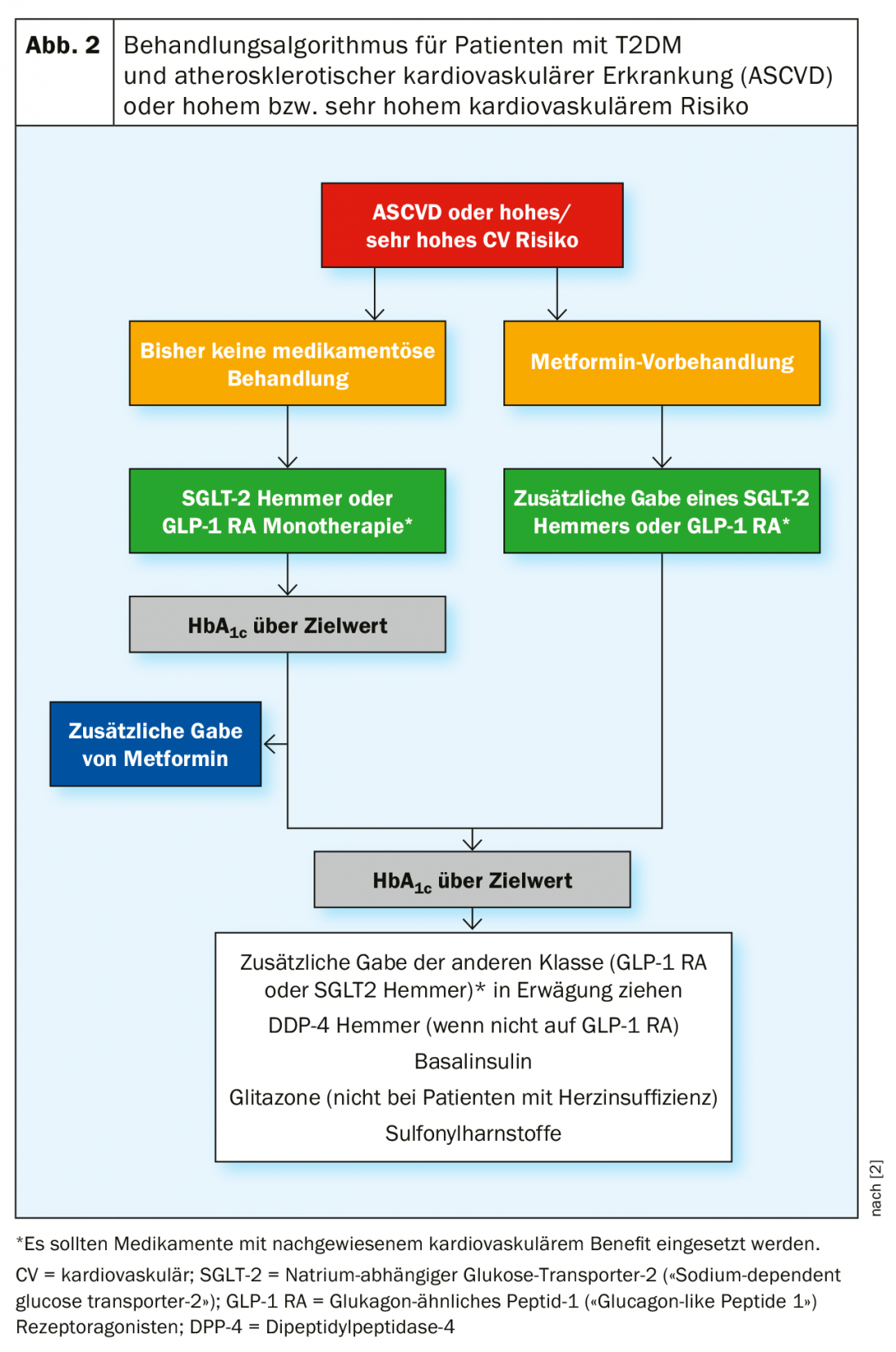
If prior non-drug treatment was given, monotherapy with an SGLT-2 inhibitor or GLP-1 RA is now indicated in the first line, and drugs with proven cardiovascular benefit should be used. If the target HbA1c cannot be achieved with this treatment, additional administration of metformin is recommended. In metformin-pretreated patients, an SGLT-2 inhibitor or GLP-1 RA should also be used [2].
If the HbA1c is still above the target value despite the combination of SGLT-2 inhibitor or GLP-1 RA with metformin, additional administration of the other class, i.e. GLP-1 RA or SGLT-2 inhibitor, can be considered first. If the patient is not on GLP-1 RA, the use of a DPP-4 inhibitor is also possible. Other alternative treatment options include basal insulin, glitazones (except in patients with heart failure), or sulfonylureas [2].
In T2DM patients without ASCVD or with moderate cardiovascular risk, metformin monotherapy is initially indicated. If this does not result in achieving the HbA1c target, DPP-4 inhibitors, GLP-1 RA, glitazones, and, if the estimated glomerular filtration rate (e-GFR) is appropriate, SGLT-2 inhibitors can be used. If the HbA1c remains above target, the other three treatment options are available after an SGLT-2 inhibitor or a glitazone. In contrast, after a DPP-4 inhibitor or GLP-1 RA, only SGLT-2 inhibitors or glitazones are recommended [2].
If this still does not lead to the desired HbA1c target value, the additional administration of other substance classes should be continued according to the recommendations given. In the last instance, the additional use of sulfonylureas (later generation with lower risk of hypoglycemia) or basal insulin (with lower risk of hypoglycemia) can be considered [2].
Treatment of DM patients to reduce the risk of heart failure.
DM patients have about a two- to fivefold increased risk of developing heart failure [11]. In addition, the presence of both conditions simultaneously increases the risk of hospitalization for heart failure and the risk of death from any or a cardiovascular cause [2]. Accordingly, heart failure risk should also be considered when treating DM patients. In this context, empagliflozin, dapagliflozin, and canagliflozin are recommended to reduce the risk of hospitalization due to heart failure, as all SGLT-2 inhibitors showed corresponding data in their respective outcome studies [1,2].
Metformin can be used in DM patients with heart failure as long as e-GFR is stable and >30 mL/min/1.73 m². GLP-1 RA and the DPP-4 inhibitors sitagliptin and linagliptin have a neutral effect on the risk of hospitalization for heart failure and may also be used in this context. Saxagliptin, on the other hand, is not recommended due to its negative effect on hospitalization rates in DM patients with prior heart failure or at increased risk of heart failure. Pioglitazone and rosiglitazone should also not be used in this patient group because they increase the risk of heart failure. The use of insulin may be considered when advanced systolic heart failure with reduced ejection fraction is present [2].
Management of CKD in T2DM
CKD developing in the context of DM is a major health problem associated with the highest risk of cardiovascular disease and therefore should be managed appropriately. However, recent data suggest that some of the newer oral antihyperglycemic drugs have beneficial renal effects. Thus, all SGLT-2 inhibitors showed renal benefit as a secondary endpoint of the respective cardiovascular outcome trial, and canagliflozin also achieved superiority over placebo in the CREDENCE trial with a renal primary endpoint [1]. Accordingly, SGLT-2 inhibitors are recommended to reduce the progression of diabetic kidney disease if e-GFR is 30 to <90 mL/min/1.73 m². In addition, treatment with the GLP-1 RA liraglutide or semaglutide should be considered if e-GFR is >30 mL/min/1.73 m² [2].
In brief: other important innovations of the ESC guidelines
Coronary revascularization: Revascularization of patients with coronary artery disease can in principle be performed by coronary artery bypass grafting or percutaneous coronary intervention. As shown in a recent meta-analysis of 11 randomized clinical trials with a total of 11,518 included patients, coronary artery bypass grafting is associated with lower mortality overall, especially in the presence of DM or higher coronary complexity [12]. Accordingly, according to current ESC guidelines, coronary artery bypass grafting should be preferred in DM patients with stable coronary artery disease and suitable anatomy for both procedures with increasing complexity of disease progression. Only in single- or branch-vessel disease with proximal stenosis of the ramus interventricularis anterior and in affected left coronary artery with low disease complexity, good recommendations can be made for both procedures [1,2].
Individualized Target Blood Pressure: Blood pressure management recommendations were revised to better reflect the effects of age and existing comorbidities. In general, it is recommended to treat all DM patients with a blood pressure of >140/90 mmHg. Younger DM patients should have a systolic blood pressure of >120 and <130 mmHg and patients over 65 years of age should have a systolic blood pressure of >130 and <140 mmHg. Diastolic blood pressure should be >70 and <80 mmHg. Depending on the presence of other diseases and individual tolerance of treatment, these target values can be modified as needed [1,2].
New lipid target values according to cardiovascular risk categories: The lipid target values have been adjusted to be consistent with the new cardiovascular risk categories. Thus, in T2DM patients at moderate cardiovascular risk, an LDL-C value <2.6 mmol/L (<100 mg/dL) should be achieved. The target value at high risk is <1.8 mmol/L (<70 mg/dL) and at very high risk is <1.4 mmol/L (<55 mg/dL), and in both cases the LDL-C reduction should be at least 50%. Depending on the LDL-C level, moderate- and high-risk patients can generally be managed with statin ± ezetimibe, whereas in very high-risk patients with persistently elevated LDL-C levels despite statin therapy, a PCSK9 inhibitor is recommended [1,2].
Aspirin in primary prevention: The new risk factor classification may also be helpful in deciding when the use of aspirin for primary prevention is appropriate. The recommendations here are that it can be considered in DM patients at high or very high cardiovascular risk in the absence of clear contraindications. In contrast, aspirin is not recommended for moderate risk [1,2].
Conclusion
The current version of the ESC Guidelines introduced a number of innovations to reflect the growing evidence from an increasing number of available studies. First, cardiovascular risk was reclassified, which in turn formed the basis for further recommendations. In addition, the interpretation of cardiovascular outcome studies in T2DM therapy has been included in the guidelines, providing a focus on the management and prevention of cardiovascular disease. In this context, there was a repositioning of metformin in T2DM management and a corresponding adjustment regarding the use of SGLT-2 inhibitors and GLP-1 RA in the first line of therapy. In addition, new recommendations have been developed for treatment with SGLT-2 inhibitors and GLP-1 RA to slow a decline in renal function in T2DM patients with CKD. Furthermore, there were changes regarding the selection of revascularization techniques, individualization of blood pressure targets, lipid targets with recommendations for the use of PCSK9 inhibitors, and the role of aspirin in primary prevention. Ultimately, this was not only an update of the existing guidelines, but above all also took into account a large number of individual patient-related aspects.
Take-Home Messages
- Current ESC guidelines divide T2DM patients into three risk categories: moderate, high, and very high cardiovascular risk.
- Metformin should be used as first-line therapy only in overweight T2DM patients without cardiovascular disease and at moderate cardiovascular risk.
- For high or very high cardiovascular risk, SGLT-2 inhibitors or GLP-1 RA are recommended in the first line to reduce the risk of cardiovascular and renal events, with empagliflozin and liraglutide additionally indicated to reduce the risk of cardiovascular death.
- To reduce the risk of hospitalization due to heart failure, the use of SGLT-2 inhibitors is recommended.
- The current ERA-EDTA guidelines recommend the use of SGLT-2 inhibitors as monotherapy or combination therapy in T2DM patients with CKD, depending on the efficacy and tolerability of pretreatment.
Literature:
- Grant PJ, Cosentino F: The 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J, 2019. 40(39): 3215-3217.
- Cosentino F, et al: 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J, 2019.
- Sarafidis P, et al.: SGLT-2 inhibitors and GLP-1 receptor agonists for nephroprotection and cardioprotection in patients with diabetes mellitus and chronic kidney disease. A consensus statement by the EURECA-m and the DIABESITY working groups of the ERA-EDTA. Nephrol Dial Transplant, 2019. 34(2): 208-230.
- Sarwar N, et al: Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet, 2010. 375(9733): 2215-2222.
- Rawshani A, et al: Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet, 2018. 392(10146): 477-486.
- Sattar N, et al: Age at Diagnosis of Type 2 Diabetes Mellitus and Associations With Cardiovascular and Mortality Risks. Circulation, 2019. 139(19): 2228-2237.
- Williams B, et al, 2018 ESC/ESH Guidelines for the management of arterial hypertension. European heart journal, 2018. 39(33): 3021-3104.
- Zinman B, et al: Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med, 2015. 373(22): 2117-2128.
- Marso SP, et al: Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med, 2016. 375(4): 311-322.
- UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet, 1998. 352(9131): 854-865.
- Nichols GA, et al: The incidence of congestive heart failure in type 2 diabetes: an update. Diabetes Care, 2004. 27(8): 1879-1884.
- Head SJ, et al: Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet, 2018. 391(10124): 939-948.
- Lehmann R: Personal communication from Prof. R. Lehmann – Chairman of the SGED/SSED Working Group.
- Neal B, et al: Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. The New England journal of medicine, 2017. 377(7): 644-657.
- Wiviott SD et al: Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. The New England journal of medicine, 2019. 380(4): 347-357.
- Husain M, et al: Oral Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. The New England journal of medicine, 2019. 381(9): 841-851.
- Gerstein HC, et al: Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet (London, England), 2019. 394(10193): 121-130.