While modern pharmacotherapies are now available for hepatitis B and C, phlebotomy remains the treatment of choice for hemochromatosis. In most cases of chronic hepatitis, antiviral therapy is indicated. Treatment of non-alcoholic and alcoholic fatty liver is largely through lifestyle modification.
In addition to non-alcoholic fatty liver disease (NAFLD), chronic liver diseases with the highest prevalence include alcohol-mediated hepatopathy (AFLD), chronic hepatitis B and C, and hemochromatosis. PD Dr. med. Christine Bernsmeier, University Hospital Basel, gave an up-to-date overview of diagnosis and treatment options in her presentation at the FOMF Update Refresher in Basel [1].
Suspicion of fatty liver – what to do?
Laboratory chemistry and histology are indistinguishable between NAFLD and AFLD. History is critical: if there was a history of critical alcohol use, it is likely AFLD. In all individuals with metabolic risk factors, liver enzymes should be determined and ultrasonography should be performed. If there is evidence of steatosis, noninvasive fibrosis markers should be determined. Whether or not a liver biopsy is needed is best decided by the gastroenterologist.
NAFLD is one of the most common hepatopathies today and is associated with metabolic syndrome. NFLD has a variable course and, like alcoholic fatty liver, can lead to cirrhosis and cancer of the liver, hepatocellular carcinoma (HCC). The prevalence of nonalcoholic fatty liver disease is increasing worldwide, and it is one of the most common reasons for liver transplantation, the speaker notes. “It’s really a relevant condition these days,” Dr. Bernsmeier said. To date, there is no approved drug therapy in Switzerland. The treatment focuses on lifestyle modification. The goal is a 7-10% weight loss through dietary changes and exercise. “This can be used to cure NAFLD,” she said. Reductions in insulin resistance, steatosis, NAS scores, and fibrosis through lifestyle interventions are considered proven [2–4]. The NAFLD Activity Score (NAS) is composed of steatosis, inflammation, and ballooning scores. The following parameters are included: Age, blood glucose, body mass index, platelet count, albumin, and AST/ALT ratio. This can be used to quantify disease activity. A score of 5 or above is associated with a greater likelihood of NASH (nonalcoholic steatohepatitis). Regarding lifestyle factor exercise, ≥3h of weekly physical activity in 3-5 training sessions is required. With regard to nutrition, in addition to reducing the amount of calories and fructose consumption, it is important to ensure an adequate intake of fluids (water). Alcohol consumption should be reduced (women <20 g/day, men <30 g/day), preferably stopped.
AFLD is histologically indistinguishable from NAFLD, the speaker explained. The clinical picture is also similar, with symptoms usually appearing at a late stage of the disease. Measurement of the two aminotransferases ALT (alanine aminotransferase) and AST (aspartate aminotransferase) provides a differential diagnosis. The AST/ALT ratio, the de-ritis quotient, can be used to estimate the extent of liver damage. For ASD:ALD>2, consider an AFLD. In confirmed AFLD, the most important thing is alcohol abstinence. There is no drug therapy so far. Not very common, but a severe condition with high mortality is a “flare” of alcoholic hepatitis. Clinical signs include right upper abdominal pain, icterus, fever, hepatic encephalopathy. Elevated bilirubin levels are detectable in the blood, ASD>ALD and leukocytosis is often measurable. If one is unsure, one can also use the Maddrey score [5]. Sonographically, a large liver is characteristic. Histologically, the main finding is a very strong neutrophilic inflammatory infiltrate. In the further course, a biopsy is advisable. For treatment of a “flare” of alcoholic hepatitis, corticosteroids may be considered as pharmacotherapeutic treatment options (e.g., prednisone 40 mg for 4 weeks). Response to therapy should be evaluated after 7 days. Strict abstinence from alcohol by patients is essential.
Hepatitis B and C are nowadays well treatable
The two most common of the five viral hepatitides, hepatitis B and C, can be acute and chronic. Modern drugs with long-term benefits are now available for both conditions.
Hepatitis B (HBV): History is critical. Risk factors for hepatitis C (affected persons in the family, blood transfusions, HIV, tattoos) should definitely be collected. The course of hepatitis B can be acute or chronic, symptomatic or asymptomatic. Increased liver values are often measurable in laboratory diagnostics. Serological HBs antigen and HBs and HBc antibodies should be raised as part of screening. HBs and HBc antibodies are immunoglobulins directed against the HBs antigen (hepatitis B surface antigen) and the HBc antigen (hepatitis B core antigen), respectively. If there is evidence of infection, HBe antigen and antibody should be requested for confirmation, as well as HBV DNA to detect possible viral replication. Ultrasound examination is extremely important to check for possible sequelae such as fibrosis or cirrhosis, as well as to check for possible hepatocellular carcinoma. Hepatitis B sufferers have an increased risk of hepatocellular carcinoma even without the presence of cirrhosis, especially those of Asian or African descent. Whether cirrhosis has developed can be determined by fibroscan. The FibroScan® is a device specifically designed to measure liver fibrosis based on the principle of transient elastography [6]. Histology is not required in all cases, but can be very informative. If chronic hepatitis has been diagnosed, antiviral therapy is indicated, regardless of whether HBe antigen is negative or positive. The exception is patients who are anti-HBc positive and are being treated with immunosuppressive agents for any reason. One must always ask whether antiviral therapy is possible under immunosuppressive therapy to prevent viral replication and a new “flare”.
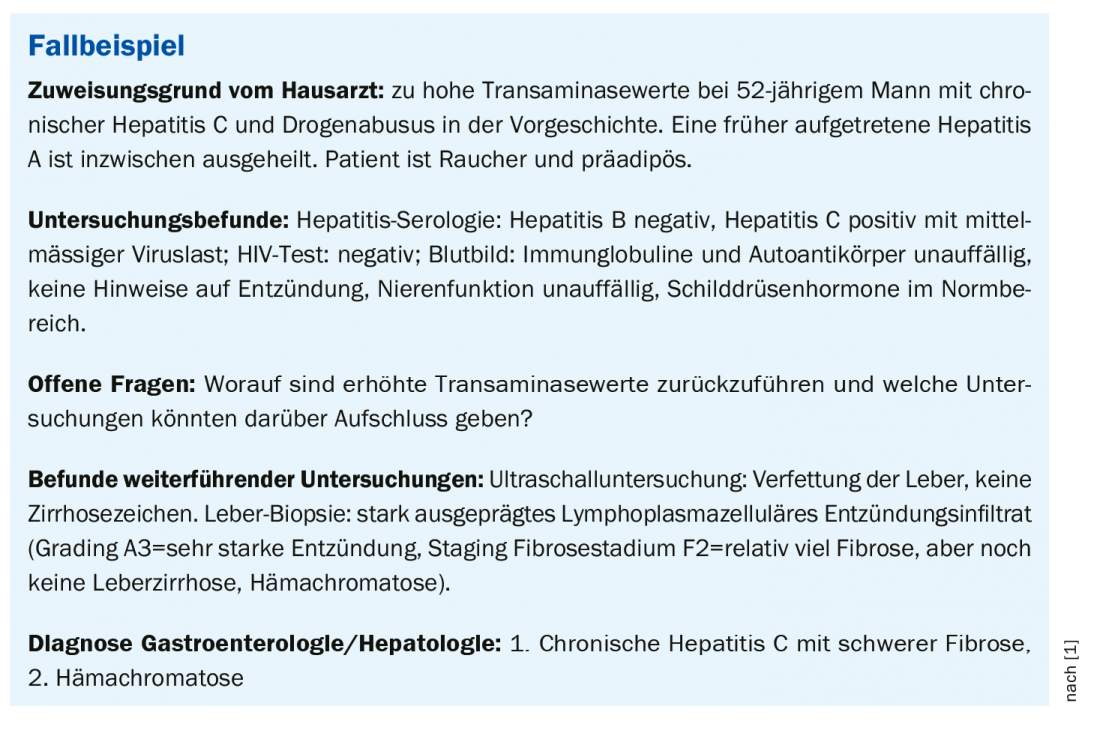
In addition to interferon therapy, there is the option of treatment with nucleotide/nucleoside analogues (NUC) (box). NUC are drugs that suppress viral replication over the long term. A disadvantage is that these preparations should be taken for at least five years or permanently. Entecavir, tenofovir, and tenofoviralafenamide are currently available antiviral agents in the NUC class of compounds and exhibit very low resistance development (Overview 1).
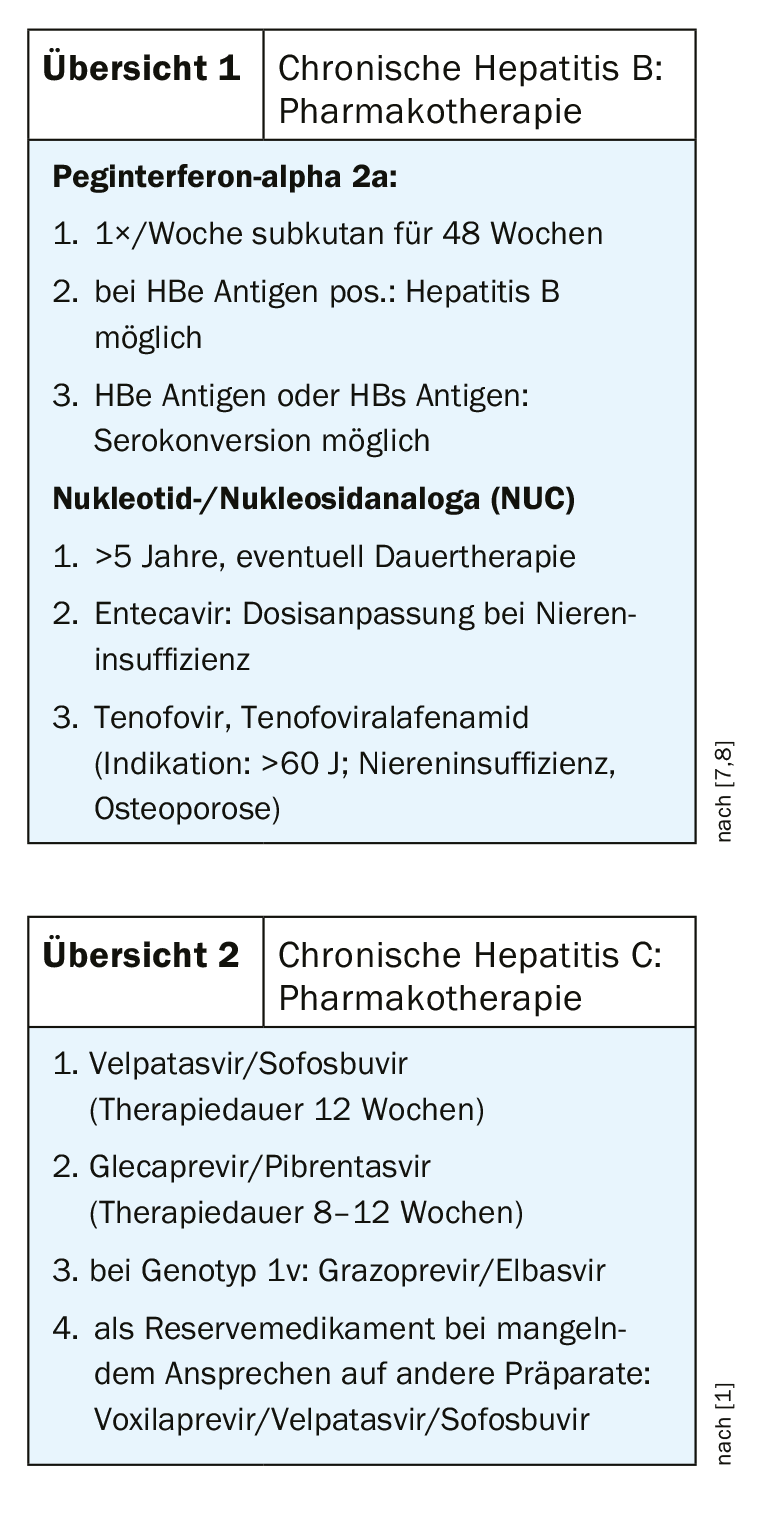
Hepatitis C (HCV): For HCV, history is also an important component of the workup (family, partners, intravenous drugs, blood transfusions, tattoos). In addition, it must be clarified whether the course is asymptomatic, whether icterus is present, and what the situation is with regard to extrahepatic manifestations. Laboratory diagnostics should include the following: AST, ALT, bilirubin, albumin, INR, creatinine. Hepatitis serology consists of HCV antibodies, HCV RNA as a confirmatory test. Sonographically, as in hepatitis B, one looks for signs of cirrhosis and for focal lesions. If there are signs of cirrhosis, screening for heaptocellular carcinoma is recommended. FibroScan® correlates very well with histological fibrosis stages [6]. Histology provides information about inflammatory activity and fibrosis/cirrhosis. In terms of treatment options, many new therapeutic options have been developed in recent years. Nowadays it is a curable disease. As with hepatitis B, the medical history is very important. One of the following treatment regimens can achieve a cure in most patients: Velpatasvir/Sofosbuvir (therapy duration 12 weeks), Glecaprevir/Pibrentasvir (therapy duration 8-12 weeks) (Overview 2) . For genotype 1v, grazoprevir/elbasvir is recommended. Voxilaprevir/velpatasvir/sofosbuvir is considered a reserve drug in case of lack of response to other preparations. To decide which therapy is most suitable, there is an app that generates suggestions as to which therapy is most promising based on data input of various relevant parameters. Relevant parameters include genotype, co-infections, fibrosis, cirrhosis, concomitant diseases, renal function, medications, previous therapy attempts). In addition, a link is provided under which, in the case of polymedication, one can check whether there are relevant drug interactions and which preparation is most suitable in view of this.
Bloodletting for hemochromatosis
Hemochromatosis is an autosomal recessive inherited disease. The frequency is approximately 1:400. Most often, a mutation is present in the HFE gene encoding the hereditary hemochromatosis protein. Iron status with ferritin and transferrin saturation is important, as well as sonography and histology. In terms of treatment options, bloodletting still has an important therapeutic value today. About 100 phlebotomies of 500 ml each are required until the excess iron is removed from the body, the speaker adds.
Source: FOMF Basel
Literature:
- Bernsmeier C: Topic presentation. Slide presentation, PD Dr. med. Christine Bernsmeier, University Hospital Basel, Update Refresher, Basel, 29.01.2020.
- Sullivan S, et al: Randomized trial of exercise effect on intrahepatic triglyceride content and lipid kinetics in nonalcoholic fatty liver disease. Hepatology 2012; 55(6): 1738-1745.
- Wong VW, et al: Community-based lifestyle modification program for non-alcoholic fatty liver disease: A randomized controlled trial. J Hepatol 2013; 59(3): 536-542.
- Vilar-Gomez E, et al: Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology 2015; 149(2): 367-378.
- Maddrey Scores, www.mdcalc.com
- FibroScan®, www.fibroscan.com
- EASL Clinical Practice Guidelines. J Hepatol 2017; 67(1): 145-172.
- Berg T, et al: Long-term response after stopping tenofovir disoproxil fumarate in non-cirrhotic HBeAg-negative patients – FINITE study. J Hepatol 2017; 67(5): 918-924.
HAUSARZT PRAXIS 2020; 15(4): 30-31