Allergies are among the most widespread diseases. Most of those affected suffer from hay fever, pollen asthma and contact allergies. In early childhood, apart from atopic eczema, food allergies are typical, most frequently to hen’s eggs. What’s new in food and contact allergies was discussed at the Allergo Update 2017 in Berlin.
Primary food allergies are usually immediate-type reactions, while secondary food allergies are predominantly pollen-associated, reported Professor Dr. Kirsten Beyer, a pediatrician and immunologist at the Charité Hospital in Berlin. Chicken egg allergies are most common in young children. In German-speaking countries, approximately every 50th child is affected in the first year of life [1]. Often, chicken egg allergy begins as early as 4-6 months of age, Beyer said. As risk factors for early sensitization to chicken egg, she mentioned neurodermatitis – about 12% of infants with neurodermatitis also have a chicken egg allergy – and cesarean delivery; the proportion here is as high as about a quarter [2]. The good news: Half of the affected children were clinically tolerant within one year in a large European study [1].
Common cross-sensitization: birch pollen and nuts
About one in four children with allergic rhinitis also has a secondary food allergy as a result of cross-sensitization, for example between birch pollen and nuts (hazelnut, almond, peanut) or apples [3]. According to Beyer, secondary food allergies most often involve oral allergy symptoms such as contact urticaria of the oral mucosa. Respiratory and severe cardiovascular reactions are rare and more typical of a primary food allergy, he said. “It’s not always peanut,” Beyer emphasized. The most common triggers of anaphylactic reactions in early childhood are hen’s egg and cow’s milk, he said.
The diagnosis of a food allergy via anamnesis (possibly with symptom and food protocol or abstinence test) and skin tests (e.g. prick tests with native foods) can be improved by measuring specific IgE against single allergens, the immunologist added. The measurement of total IgE is usually not helpful. Oral provocation tests are usually required for reliable detection of a food allergy. They should be standardized and stationary.
According to the food allergy guideline, abstinence is the most important therapeutic intervention [4]. In the case of primary food allergies, allergen-specific immunotherapy is also an option, but is currently only used in controlled studies. So far, the best results have been achieved with oral immunotherapy, Beyer reported, adding that an alternative with a good safety profile is epicutaneous immunotherapy. Subcutaneous or sublingual immunotherapy with pollen allergens should only be given if pollen-related respiratory symptoms exist at the same time.
Patients with severe food allergy would also be entitled to oral provocations in the further course to document the development of tolerance, Beyer said. “One in five children with a peanut allergy loses the allergy,” she said. If the provocation, which corresponds to a boost, is negative, the foods in question should be fed three times a week, if possible, to maintain tolerance.
Around one in four Europeans has a contact allergy
Contact allergies (delayed type 4) are disproportionately more common than food allergies, usually run a less dramatic course, but can become significant hurdles in career choices. About a quarter of Europeans have contact allergy, according to a recent cross-sectional study of 2400 people from Sweden, the Netherlands, Italy, Portugal, and Germany [5], reported Professor Christiane Bayerl, M.D., dermatologist at the Helios Clinics in Wiesbaden, Germany. Atopics had no increased risk, and significant regional differences were found only for nickel, still the number 1 contact allergen, and thiomersal, a preservative in ophthalmics, blood plasma preparations, and cosmetics. In many countries, thiomersal, formerly also contained in vaccines, has rightly been removed from the standard test series, Bayerl said.
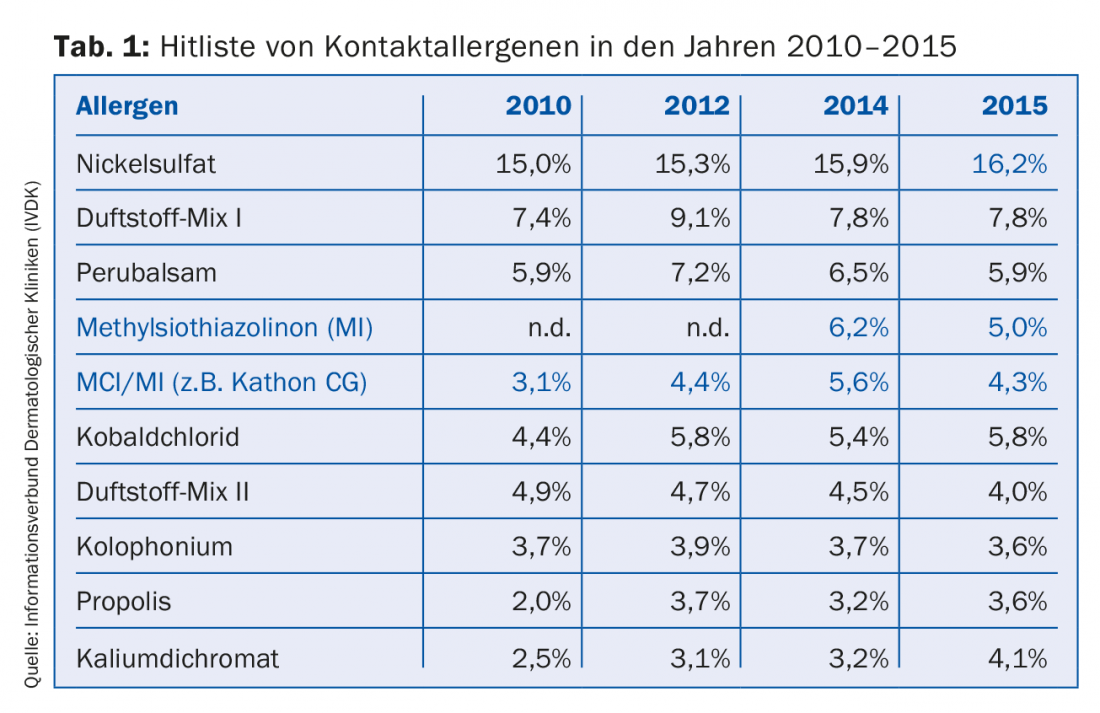
According to current figures from the Information Network of Dermatological Clinics (IVDK) in Germany, Austria and Switzerland, the hit list of contact allergens in 2015 includes nickel sulfate in first place (16%), followed by fragrance mix I (8%), Peru balsam (6%), and methylsiothiazolinone (MI) and MCI, preservatives in wound care products and cosmetics (Table 1). Contact allergies to chromates (potassium dichromate) have increased (currently 4%), Bayerl reported. Sulfites (e.g. in cosmetics and light protection products, but also in topical preparations such as antifungals and corticosteroids) would no longer be among the top ten in German-speaking countries, although they could be of occupational relevance, for example for photographers, hairdressers, winemakers/brewers, chemical workers and dentists. As a rule, contact sensitization is of low severity, with the exception of contact urticaria syndrome. With patients with periorbital eczema therefore also a possible sulfite allergy should be tested, advised the dermatologist. If possible, corticosteroids and immunomodulators should be discontinued prior to an epicutaneous test, as these substances may suppress the test response.
Not uncommon: Contact eczema due to injection of lidocaine.
Contact dermatitis – according to a survey by the Robert Koch Institute in Germany, the lifetime prevalence is 10% in children and 8% in adults [7] – can also be triggered in physicians by the injection of local anesthetics such as lidocaine. In a European study evaluating more than 400 each of hand and foot eczema, 30% combined, more than half of those affected were found to have contact allergies, often occupational.
Contact dermatitis may also develop after systemic exposure to allergens, such as drugs or food. Bayerl described the case of a 56-year-old woman who had developed itchy exanthema and scratch marks on her skin after consuming shiitake mushrooms or having skin contact. As it turned out, they were shiitake grown on the log, imported from China. Aromatic resins in the wood or fungicides may have been the triggers of the dermatitis, Bayerl speculated.
Patients frequently mention possible allergies to amalgam and toner dust. In patients with oral lichenoid lesions and amalgam fillings, amalgam contact allergy is quite possible, Bayerl reported. In a prospective cohort study of 53 patients with oral lichenoid lesions, 59% were found to have amalgam contact allergy. In 10 patients the fillings were removed and in all of them the lesions in the oral cavity improved, in three they healed completely [9].
However, there is no evidence of a harmful effect of toner dust, reported occupational physician Professor Dr. Dennis Nowak of the University Hospital in Munich. An association between toner dust and contact dermatitis is considered equally unlikely. According to Bayerl, a corresponding application by a tax office employee in Germany as an occupational injury was rejected by the Münster Higher Administrative Court.
Literature:
- Xepapadaki P, et al: Allergy 2016; 71(3): 350-357.
- Bellach J, et al: J Allergy Clin Immunol 2016, epub August 12.
- Mastrorilli C, et al: Allergy 2016; 71: 1181-1191.
- Worm M, et al: Allergo J Int 2015; 24: 257.
- Diepgen TL, et al: Br J Dermatol 2016; 174: 319-329.
- Information Network of Dermatological Clinics (IVDK) in Germany, Austria and Switzerland, www.ivdk.org/en.
- Bergmann KH, et al: Allergo J Int 2016; 25: 22-26.
- Agner T, et al: JEADV 2016; doi: 10.1111/jdv.14016.
- Thanyavuthi A, et al: Dermatitis 2016; 27: 215-221.
HAUSARZT PRAXIS 2017; 12(3): 38-40
DERMATOLOGIE PRAXIS 2017; 27(2): 35-36











