In addition to the metabolic syndrome, type 2 diabetes also affects the blood vessels, heart and kidneys, among other things – this has been revealed by scientific research into the pathogenesis of the disease. The main goal of treatment is primarily the prevention of macrovascular and microvascular events. Modern therapy management therefore addresses the cardio-nephrological portfolio in addition to blood glucose lowering.
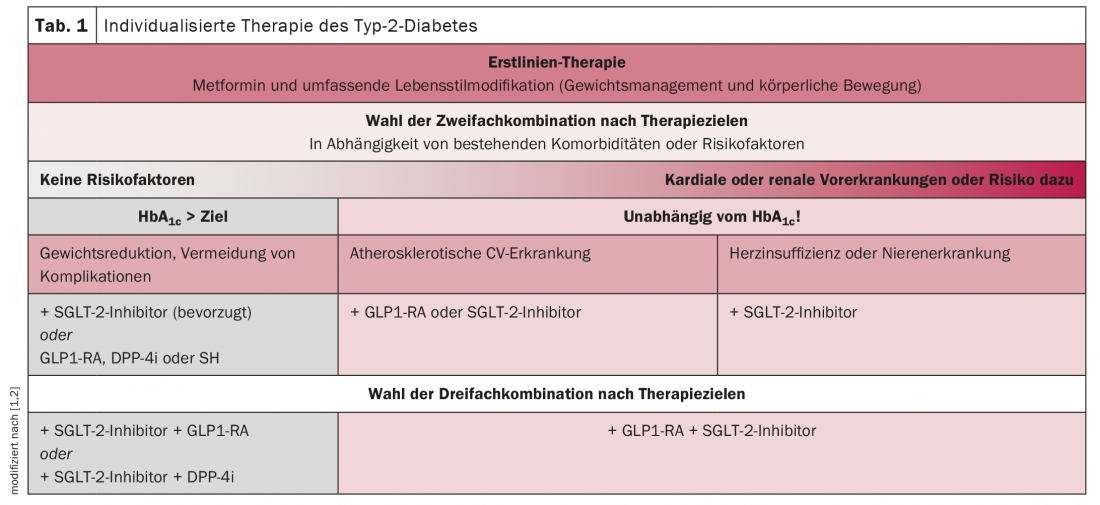
Type 2 diabetes is based on chronic hyperglycemia, beta cell dysfunction and insulin resistance. Glucose load in particular plays a major role here, because the insulin response decreases as fasting glucose rises. It is also considered a risk factor for microvascular and macrovascular sequelae, which must be avoided, reported Prof. Mathias Blüher, MD, Leipzig (D). The goal of effective treatment management is therefore to permanently lower blood glucose. Most antidiabetic drugs affect insulin secretion or insulin action. Metformin and thiazolidinediones increase insulin sensitivity; glinides, sulfonylureas, DPP-4 inhibitors, and GLP1 receptor agonists increase insulin release. In contrast, independently of insulin, SGLT2 inhibitors lowered glucose load by directly excreting glucose. In addition, studies show a beneficial effect on cardiovascular risk factors early on. These include hypertension, obesity, and albuminuria, in addition to age, gender, diabetes duration, and lifestyle. Studies show that the administration of SGLT2 inhibitors can effectively lower both blood pressure and body weight in addition to HbA1c levels.
Increased mortality risk
Professor Dr. med. Jochen Seufert, Freiburg (D), also confirms that the newer antidiabetic drugs can do more than “just” lower blood sugar. This is essential because type 2 diabetes, heart failure, and renal insufficiency additively increase mortality risk. The probability of all-cause and cardiovascular mortality increases by 60-80% in diabetic patients with heart failure. In addition, it has been shown that declining renal function may be a stronger predictor of mortality than prior myocardial infarction. The basis of multimodal type 2 diabetes therapy is lifestyle modification measures such as weight loss, exercise, and smoking cessation. If these are not sufficient, drug therapies are used. Metformin remains the drug of first choice for this purpose. However, national and international guidelines now recommend early combination with an SGLT2 inhibitor or GLP1 receptor agonist if there is a high cardiovascular risk. Through insulin secretion, glucagon suppression, and appetite suppression, GLP1 receptor agonists reduce inflammation, coagulation, and postprandial lipid levels while improving LV function. Thus, they reduce the risk of cardiovascular events, albuminuria, blood pressure, weight and, last but not least, the HbA1c level. SGLT2 inhibitors mediate beneficial cardio-renal-metabolic effects through a host of other mechanisms, including classic atherosclerotic pathways, the expert said. Outcomes include reductions in MACE, cardiovascular death, HHF, severe kidney disease, and albuminuria.
Congress: Diabetes Congress (DDG)
Literature:
- Jaeckel E, Schneider C, Simon J, Haller H: Pre-existing conditions determine modern diabetes therapy: reducing cardiac and renal complications. Diabetes Metabolism and Heart 2019; 28: 339-348.
- National health care guideline type 2 diabetes 2021; available at: www.leitlinien.de/themen/diabetes
CARDIOVASC 2021