New therapeutic approaches work with virtual reality, hyperthermia, buprenorphine, and psilocybin, among others. New evidence is available on light therapy, ketamine treatment, and folic acid substitution. Gain or disorientation – that is the question.
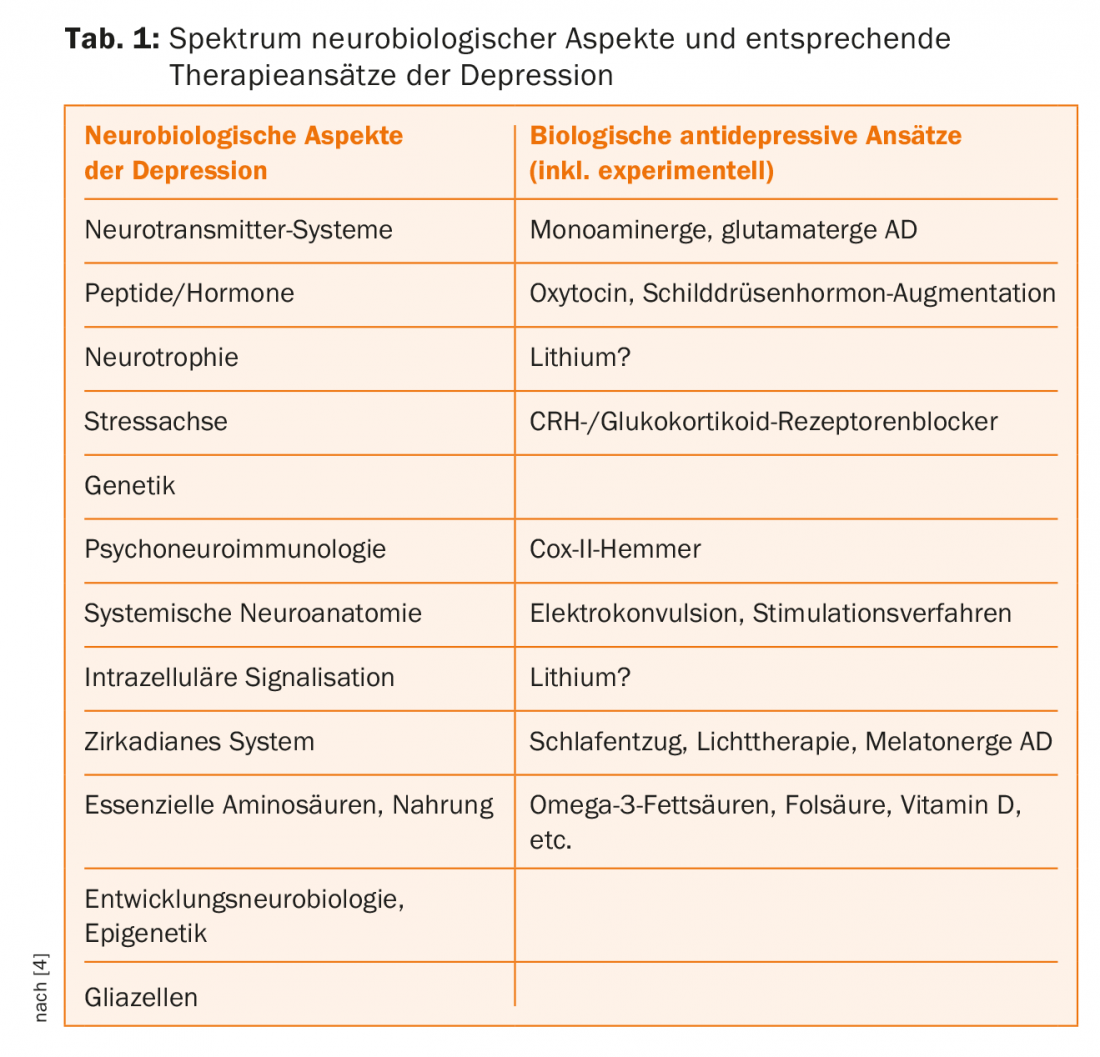
Depression is one of the most burdensome diseases with an increasing tendency in terms of years of life lived or lost due to the disease [1]. On the other hand, despite billions of dollars of investment, no fundamentally new therapeutic principles have been able to establish themselves on a broader clinical scale for more than half a century, and we still have to face substantial resistance to therapy. In addition, there is a high heterogeneity of neurobiological and psychological approaches to the etiology of depression and the fact that there is simply no integrative pathophysiological model of depression. This is also reflected in the diagnosis, which for over a century has been based on psychopathological criteria, but despite the clear concept of a biological part in the genesis, knows no biological diagnostic criteria, except for the exclusion of a physical underlying or concomitant disease.
Today, we still prefer to treat depression with monoaminergic medication, psychotherapy, and, as the most effective principle [2], electroconvulsive therapy. In addition, we take social factors into account. Certainly, these methods have been refined, more specific and with fewer side effects. Qualitatively fundamental new approaches have been investigated, but no method has yet gained acceptance. These include stimulation techniques such as transcranial magnetic or direct current stimulation, as well as vagus nerve and deep brain stimulation. There have also been and still are approaches on the drug level, for example, to act on the stress axis (CRH receptor antagonists, mifepristone), on the immunological level (celecoxib), on glutamatergic neurotransmission (ketamine), or on hormonal balance as with oxytocin. However, depending on their efficacy and side-effect profile, these approaches have since been abandoned or at best play a marginal role in everyday clinical practice as add-on treatments for treatment-resistant depression.
But the search continues. Thus, over the past year, several interesting newer antidepressant approaches or new findings on approaches already known but not widely established have been published. These can be classified as somatic or technical procedures and drug procedures. New findings on psychotherapeutic procedures are also available, but are not the focus here.
Somatic or technically assisted treatment approaches
The soothing effect of heat is known to everyone who sits in the first sun in spring or once used a hot water bottle. Now, researchers have investigated the antidepressant effect of a single whole-body hyperthermia in 30 depressed patients in a randomized trial [3]. In the verum group, core body temperature was successively raised to 38.5°C over 80-140 minutes using a special apparatus and then slowly cooled again over 60 minutes. A control group also received heat application, but to a much lesser extent. The verum group experienced more pronounced improvement in depression symptoms over six weeks, as measured by the Hamilton Depression Scale, than the control group. As a possible neurobiological mechanism of action, the authors cite the activation of brain areas that mediate well-being, which are activated by heat. They conclude that whole-body hyperthermia could become a simple antidepressant treatment option with few side effects, but its efficacy and optimal use remain to be explored in further studies.
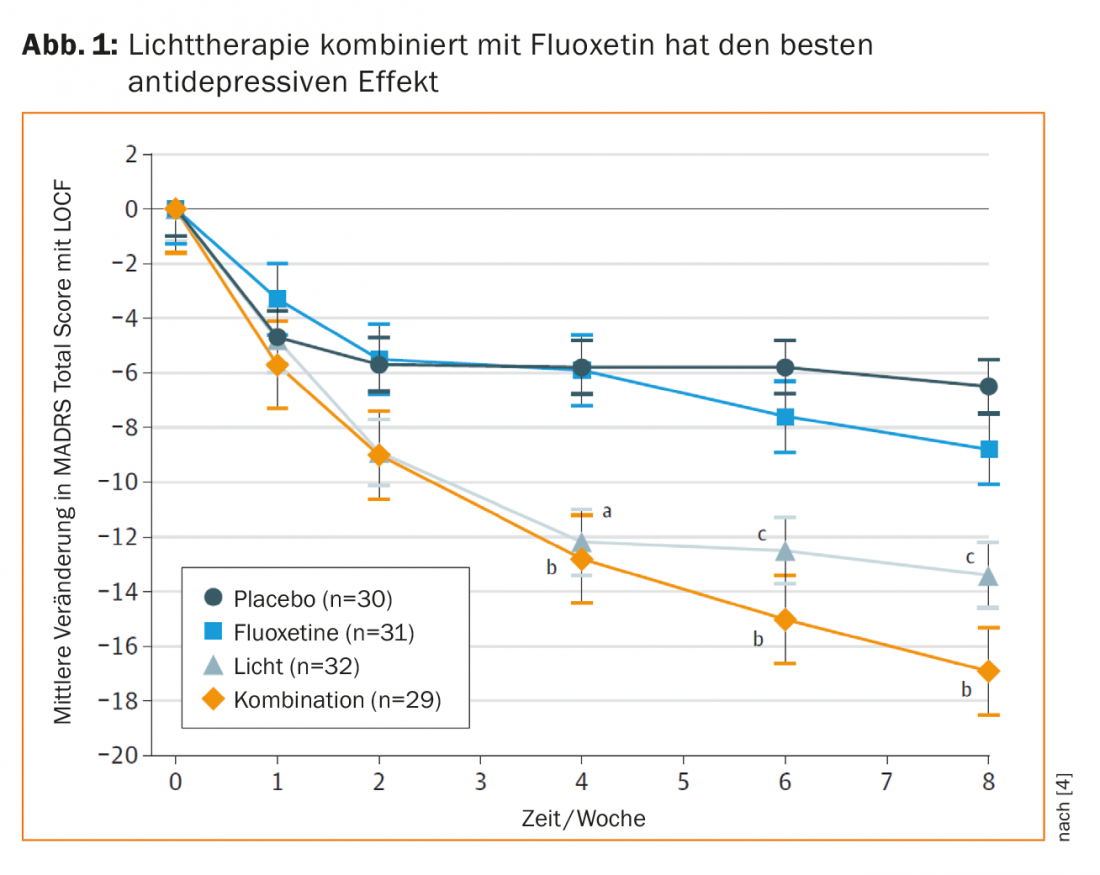
Light therapy has been established for seasonal depression for some time and the effect can also be extrapolated from spring sunshine. Now, however, researchers have also demonstrated the general efficacy of light therapy in combination with fluoxetine for depressive episodes (Fig. 1) [4]. Patients with a nonseasonal depressive episode benefited more from combination treatment than from the monotherapies or placebo. Interestingly, light treatment was statistically and otherwise at least descriptively superior to fluoxetine at the time point after four weeks. This implies the use of light therapy in depressed patients also independent of seasonal occurrence, especially since this can be implemented in practice with few side effects and low threshold.
In an impressive approach using virtual reality, the research group led by Falconer et al. [5] the effect of self-compassion. 15 depressed patients initially cared for a crying child from an adult perspective in a virtual environment. Then their own interventions were applied to themselves, now themselves in the child’s perspective. This was done three times. After the interventions, patients were significantly better and had higher self-compassion scores on appropriate scales. Even though the study was conducted as an open study, i.e., without placebo intervention, with a relatively small number of participants, it gives reason to expect that appropriate interventions could be used in an antidepressant supportive manner.
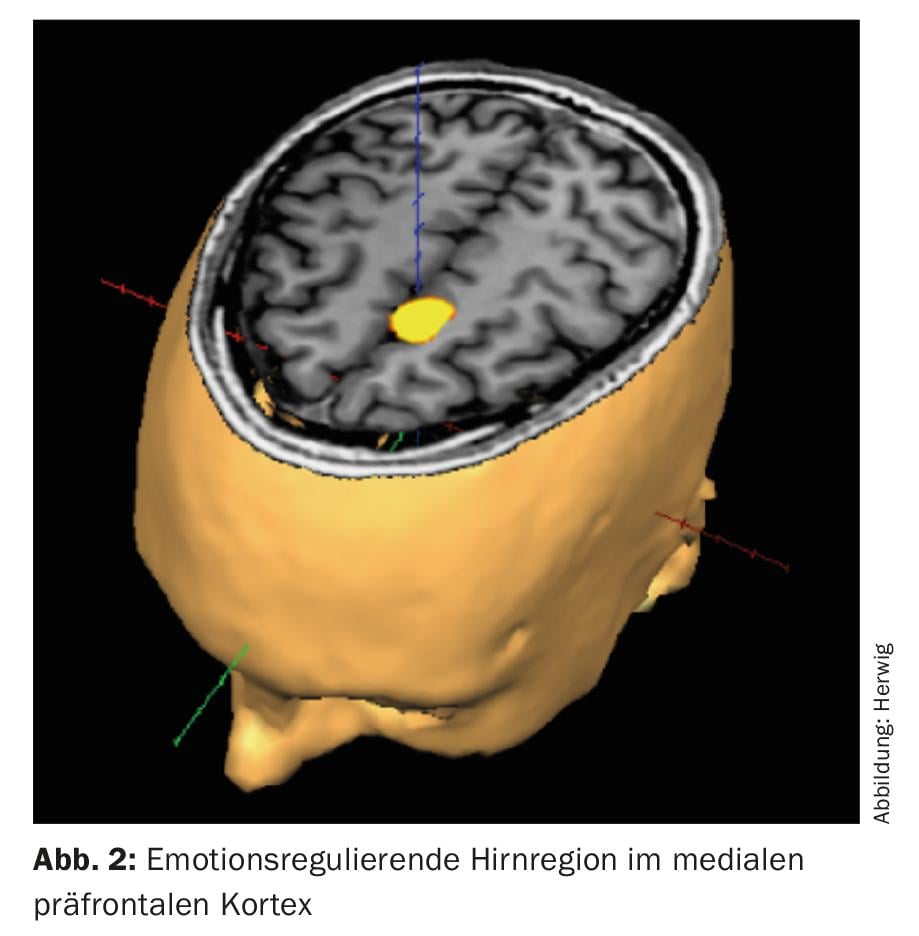
Another approach of linking neurobiological findings and possible depression-relieving psychological processes lies in neurofeedback with functional magnetic resonance imaging. Here, training of emotion regulation could already be shown in healthy subjects (Fig. 2) [6], now it was also demonstrated in depressed patients that the feedback of their own brain activity was supportive for the reduction of depression-typical cognitions [7]. Therapeutic use is under further investigation and, if successful, could represent a new dimension of an integrated neurobiological-psychotherapeutic treatment approach. However, we are still at the very beginning on the way to understanding more complex psychological-psychodynamic processes at the level of central nervous information processing [8] and a possible broader therapeutic use is still well ahead.
Pharmacological approaches
Paracelsus is said to have treated depression with opium. Now opioids are finding their way back into antidepressant treatment. In recent years, some research groups reexamined the role of opioids in antidepressant treatment given the importance of the opiate system in emotional information processing, including in depression. Fava and colleagues [9] demonstrated that the combination of buprenorphine and samidorphan, i.e., a partial μ-opioid receptor agonist and a potent μ-antagonist, combined in a sublingual tablet of 2 each mg, when administered for four weeks, led to a reduction in depressive symptoms in treatment-resistant depressed patients, and there were no withdrawal symptoms after discontinuation of the medication. However, again, the result relates to a rather small sample number and, interestingly, it was not significant for the administration of 8 mg each. Nevertheless, larger studies are eagerly awaited and pathophysiologically the path via the opiate system seems to be a promising approach if dependence risks can be kept under control in this way.
Another substance that is generally viewed with a critical eye is psilocybin. The potent hallucinogen exhibits marked serotonin agonism (5HT-2A), which in itself is associated with a possible antidepressant effect. In addition, the psychedelic effects are also seen as possibly psychodynamically therapeutically usable, as expressed in psycholytic therapy – with some tradition in Switzerland. In an open-label design study [10], twelve treatment-resistant depressed patients received psilocybin twice a week apart. The researchers observed an impressive antidepressant effect, which was still partly present after three months. Here an interesting new option arises, which purely pharmacologically is also located at the monoaminergic level, but in combination with possible psychodynamic effects opens a new dimension of linking neurobiology and psychotherapy.
There is also new evidence on a still experimental antidepressant approach, the administration of ketamine. Ketamine is a long established anesthetic in anesthesia with agonistic effects at NMDA, or glutamate, receptors. Glutamate is the most widely distributed excitatory neurotransmitter in the central nervous system. At first glance, one might say that it stimulates neurotransmission in general, but this is far too unspecific for an antidepressant effect and, moreover, pharmacologically a very short-term effect. Nevertheless, the number of positive studies has been increasing in recent years. In 2016, Singh et al. [11] of a clinically significant effect of twice-weekly intravenous application. Now there is evidence that it is not the NMDA agonist effect that is crucial at all, but the effect of a ketamine metabolite on AMPA receptors [12]. These also belong to the group of glutamate receptors and are important for synaptic plasticity, among other things. This opens up a new pathophysiological antidepressant approach, which will certainly be looked at more closely in the future.
Good food in itself creates a sense of well-being. Not to be neglected are essential nutritional contents, which in case of deficiency can lead to depressive symptoms, among other things. A recent review [13] points out aspects that are also significant for clinical practice. The authors state that augmentative administration of folic acid, omega-3 fatty acids, S-adenosylmethionine, and vitamin D may lead to antidepressant effects. Interestingly, despite normal serum folic acid levels, two-thirds of depressed patients studied were found to have reduced cerebrospinal fluid folic acid levels, the correction of which had also led to an improvement in depressive symptoms [14]. This area of possible antidepressant approaches can be given quite low-threshold attention in everyday clinical practice, with few side effects, via substitution.
Conclusions
This list, which is by no means exhaustive, shows the diversity of antidepressant approaches and thus also a certain lack of orientation. Different psychotherapy strategies were not discussed at all. Nevertheless, the new findings help to provide even more differentiated and broadly diversified offerings in everyday life.
Overall, however, the complexity of the phenomenon of depression and, at the same time, the limitations of our current knowledge are expressed here. We are also at the very beginning on the level of neurobiological markers for diagnostics and therapy response predictors for an individual selection of antidepressive measures. In addition, it should be noted that even if the antidepressant treatments currently available do have some efficacy, they reach only a small proportion, about one-fifth, of sufferers [15]. This still has its own potential, bringing together existing antidepressant procedures and sufferers.
Literature:
- DALYs GBD, Collaborators: Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet 2015; 386: 2145-2191.
- Group UER: Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 2003; 361: 799-808.
- Janssen CW, et al: Whole-Body Hyperthermia for the Treatment of Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016; 73: 789-795.
- Lam RW, et al: Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016; 73: 56-63.
- Falconer CJ, et al: Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open 2016; 2: 74-80.
- Brühl AB, et al: Real-time Neurofeedback Using Functional MRI Could Improve Down-Regulation of Amygdala Activity During Emotional Stimulation: A Proof-of-Concept Study. Brain Topogr 2014; 27: 138-148.
- Hamilton JP, et al: Effects of salience-network-node neurofeedback training on affective biases in major depressive disorder. Psychiatry Res 2016; 249: 91-96.
- Christoff K, et al: Mind-wandering as spontaneous thought: a dynamic framework. Nat Rev Neurosci 2016; 17: 718-731.
- Fava M, et al: Opioid Modulation With Buprenorphine/Samidorphan as Adjunctive Treatment for Inadequate Response to Antidepressants: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry. 2016; 173: 499-508.
- Carhart-Harris RL, et al: Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry 2016; 3: 619-627.
- Singh JB, et al: Double-Blind, Randomized, Placebo-Controlled, Dose-Frequency Study of Intravenous Ketamine in Patients With Treatment-Resistant Depression. Am J Psychiatry 2016; 173: 816-826.
- Zanos P, et al: NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature 2016; 533: 481-486.
- Sarris J, et al. Adjunctive Nutraceuticals for Depression: A Systematic Review and Meta-Analyses. Am J Psychiatry. 2016; 173: 575-587.
- Pan LA, et al: Neurometabolic Disorders: Potentially Treatable Abnormalities in Patients With Treatment-Refractory Depression and Suicidal Behavior. Am J Psychiatry 2017; 174: 42-50.
- Thornicroft G, et al: Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. 2017; 210: 119-124.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(3): 28-31.











