A detailed ophthalmologic examination with eye pressure measurement should be performed in everyone from about the age of 40 (depending on the risk profile). Adherence and persistence of patients with glaucoma disease are significantly reduced, as in other chronic asymptomatic diseases. Good collaboration between the primary care physician and the ophthalmologist is important to identify interactions between the various medications prescribed.
What is glaucoma?
Glaucoma is a progressive disease of the optic nerve that can lead to blindness if left untreated. After age-related macular degeneration, it is the second most common cause of irreversible blindness in the industrialized world. Glaucoma can manifest at any age, but the incidence of the disease increases significantly with age. It is assumed that in Switzerland 2.5% of all persons over 40 suffer from glaucoma. It is remarkable that more than half of the affected patients are unaware of their disease [1].
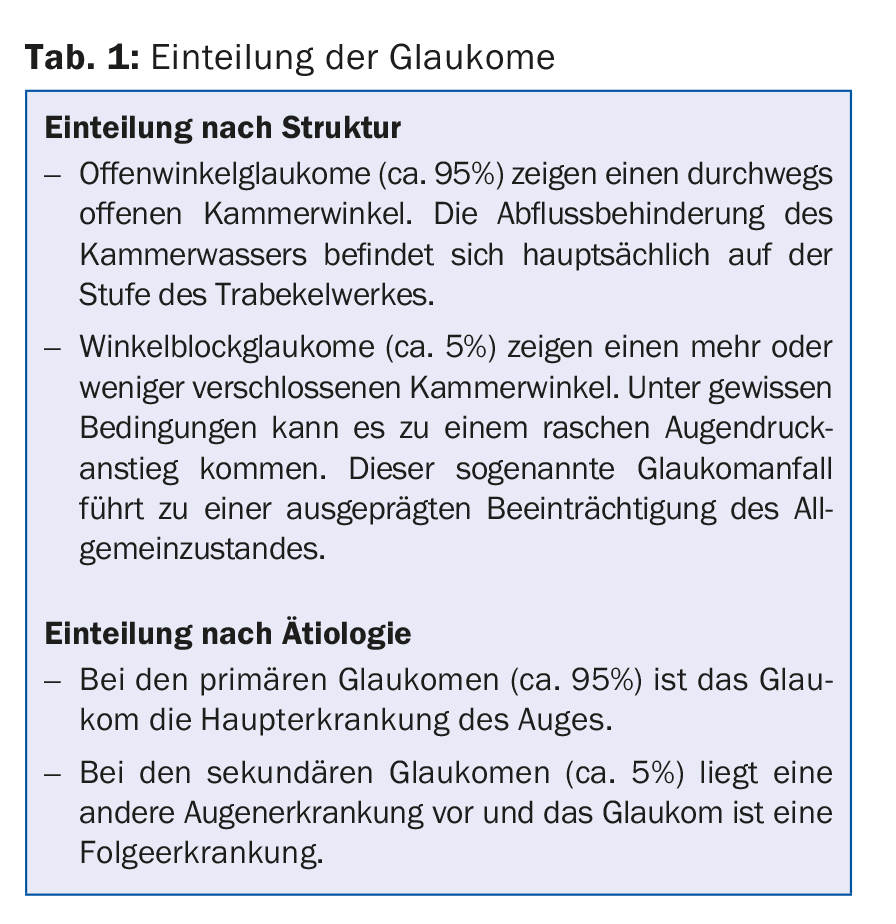
Glaucomas can be classified either by their structure or by their etiology (Table 1).
What exactly happens in the eye during glaucomatous disease?
Each eye has a measurable internal pressure that is controlled by the ratio of aqueous humor production and aqueous humor outflow. In glaucoma, there is a mismatch of these two components, with outflow through the chamber angle being particularly impaired. If the intraocular pressure rises above the tolerable pressure for the eye in question, progressive damage occurs at the weakest point, the optic nerve. The increasing optic nerve damage leads to a slow decrease of the visual field.
Symptoms of glaucoma disease
Glaucoma belongs to the group of practically symptomless chronic diseases. Exceptions are congenital glaucoma, in which children are often photophobic and show increased tearing in addition to markedly enlarged corneal diameters, and acute glaucoma described above.
It is astonishing that patients hardly notice a slowly increasing eye pressure increase and thus can have eye pressure values up to more than 40 mmHg without showing symptoms. Since the visual field deficits first affect the periphery, the patient usually does not notice a reduction in the visual field until the disease is in an advanced stage.
Which patients should definitely see an ophthalmologist?
In a healthy person without an ophthalmologic history, it is recommended to take the first eye pressure measurement at the age of 40-45 years, usually in the course of determining the first pair of reading glasses. This examination should be performed by an ophthalmologist, since measuring eye pressure alone without examining the entire eye is nonsensical. However, if risk factors are present, the first ophthalmologic examination must take place earlier.
Risk factors
Familial risk factors: glaucoma disease in the next of kin.
Personal risk factors: Age, race, gender, refractive abnormalities (such as high myopia), circulatory abnormalities (systemic hypotension, migraine, Raynaud’s symptomatology). The role of arterial hypertension and diabetes mellitus are still controversial.
There are medications that can promote the development of glaucoma (such as cortisone). In addition, anticholinergic and sympatomimetic drugs can trigger a glaucoma attack in patients with a narrow-angle constellation.
Local risk factors: The main risk factor is elevated eye pressure. In addition, there are deposits in the eye (pseudoexfoliation, pigment dispersion), which settle in the chamber angle, thereby impairing the outflow of aqueous humor and can lead to an increase in eye pressure.
Investigations
The ophthalmologist takes a medical history to determine the risk profile. During the examination, the refraction and visual acuity of the eye are determined. The eye is examined at the slit lamp to measure eye pressure and identify any local risk factors. Optimal intraocular pressure ranges from 8-21 mmHg.
If glaucoma is suspected, additional examinations are ordered: Determination of the visual field, morphological imaging of the optic nerve, visualization of the chamber angle using a contact lens, and various eye pressure measurements, including a detailed examination of the cornea.
Management
In a patient with suspected glaucoma, the ophthalmologist first decides, based on the examination results, whether it is a borderline case or whether glaucoma is already present. In borderline cases, it is important to inform the patient precisely about the disease and the possible consequences. We recommend regular checks of intraocular pressure, optic nerve function (visual field), and morphology (visualization of the optic disc using color photographs and computer-aided measurements).
In manifest glaucoma, the main risk factor in particular must be treated. The therapy of elevated intraocular pressure can be performed with medication, laser or surgery.
We have five different drug groups available for drug therapy:
Prostaglandin agonists: These improve aqueous humor outflow. They are easy to use (usually once daily) and have few systemic side effects. On the other hand, they can cause certain local changes (discoloration of the iris and the surrounding skin of the eyelids).
Beta-blockers: used once or twice a day, they reduce the production of aqueous humor. They are well tolerated locally, but sometimes show serious systemic side effects, especially in patients with cardiac and pulmonary disease. We recommend intensive cooperation with the family doctor in charge.
Alphaagonists: act on both aqueous humor production (reducing production) and aqueous humor outflow (improving). They are applied twice a day and may have systemic side effects in addition to local, mostly allergic ones (important: possible interference with certain systemic drugs).
Carboanhydrase inhibitors: Used two to three times daily, they again decrease aqueous humor production. They belong to the sulfonamide group and can lead to dangerous complications in patients with sulfonamide allergy.
Miotics: Are now only needed in patients with angle closure glaucoma.
The main problem with glaucoma drug therapy is patient adherence and persistence. Research shows that
- the adherence rate in glaucoma patients (similar to other chronic asymptomatic diseases) is only 30-70% [2].
- the number of bottles used is important: with two bottles and the use of more than three drops per day, non-adherence is 67% [3]. This is the reason for the increasing number of combination preparations (with two drugs per bottle).
- the persistence of patients – i.e. the number of those patients who use the medication continuously – drops to 25% after one year [4].
Therefore, it is essential to inform the primary care physician about the patient’s ophthalmologic therapy.
Other risk factors must also be controlled and, if necessary, treated. Vascular risk factors are important, especially blood pressure: 24-h blood pressure curves can be used to identify nocturnal irregularities. Specifically, I would like to emphasize artificially induced (often by overtreatment of arterial hypertension) nocturnal blood pressure drops (systolic below 90 mmHg and diastolic below 50 mmHg), which can lead to progression of glaucoma disease.
When is surgical therapy considered? This depends on the stage of glaucoma and the age of the patient. In a younger patient with advanced disease, surgical intervention is planned early. Certain forms of glaucoma sometimes respond quite well to laser therapy. However, since the eye pressure lowering effect of laser therapy only lasts for a certain period of time, this procedure is mainly considered for older patients.
In the surgical field, new surgical forms have recently been added to the known surgical forms (improvement of outflow by a trabeculectomy or by insertion of an outflow-improving tube). These MIGS (“Minimally Invasive Glaucoma Surgery”) are easier to perform but are less effective at lowering eye pressure. It remains to be seen which form of therapy will prevail.
Aftercare of a surgical procedure is performed by the attending ophthalmologist and usually consists of local application of anti-inflammatory drops.
Acknowledgments: The author thanks Prof. Dr. J. Stürmer, Winterthur, for critical review of the manuscript.
Literature:
- Quigley HA: The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90: 262-267.
- Terminology and Guidelines for Glaucoma.4th edition. Savona: European Glaucoma Society, 2014.
- Patel SC, et al: Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surgery 1995; 26(3): 233-236.
- Schwartz GF, et al: Adherence and persistence with glaucoma therapy. Survey of Ophthalmology 2008; 53(Suppl 1): S57-62.
HAUSARZT PRAXIS 2016; 11(9): 28-30











