Renal insufficiency requiring dialysis can be the result of glomerular disease that is recognized too late, usually with nonspecific symptoms and signs. Screening for renal pathologies therefore includes not only measurement of blood pressure but also determination of serum creatinine, a blood count and urinalysis by the general practitioner. In the case of pathological findings, further clarification should be performed by a specialist. Therapy of the underlying disease always includes good blood pressure control and avoidance of nephrotoxic substances such as NSAIDs and X-ray contrast media.
If the filtering elements of the kidneys, the glomeruli, become inflamed, we speak of glomerulonephritis (GN). They cause only nonspecific symptoms and signs; however, the location and severity of glomerular damage are associated with characteristic clinical patterns of damage that often allow differential diagnosis of underlying glomerular disease. A renal biopsy helps to elucidate the specific renal disease, which in turn then allows conclusions to be drawn about whether to look for a disease limited to the kidney or even a systemic disease. While renal-specific examinations and interventions are performed by the specialist, screening for renal pathologies is the domain of the primary care physician. The recognition, treatment, and progression of glomerular damage follow some general principles that can be applied to most GN.
Clinical patterns of damage in glomerulonephritis.
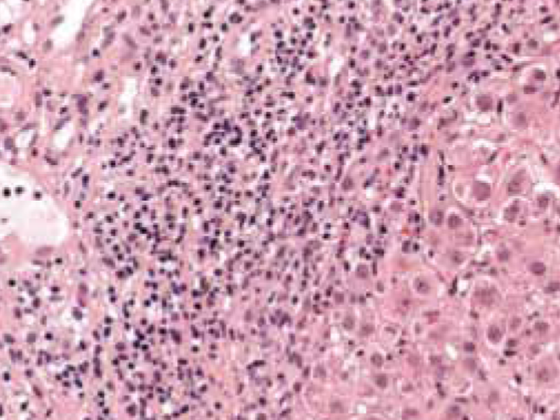
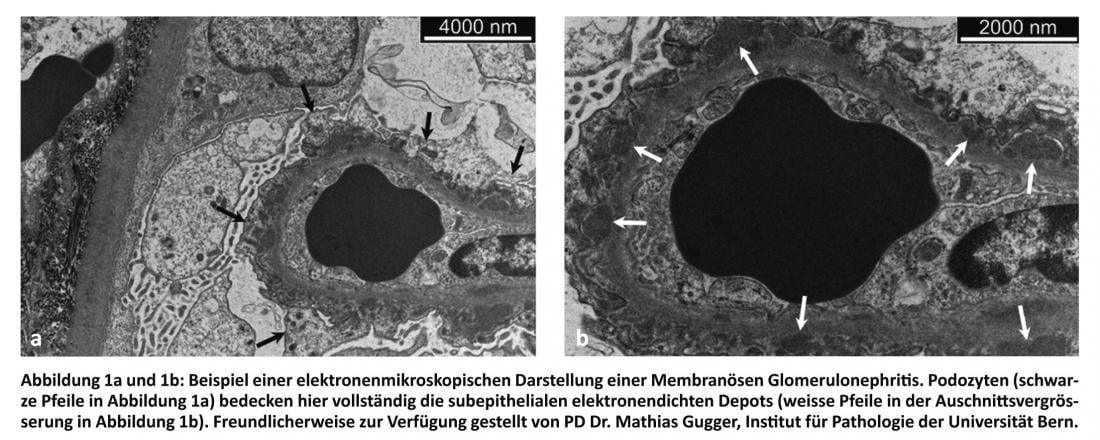
Various cell types and structures may be pathologically altered in a glomerulus. Many of these changes can be attributed to immune complex disease. Damage to the basement membrane and/or externally adjacent podocytes often results in increased permeability of the glomerular filter and consequent proteinuria (PU). Damage to the endothelium with rupture of the capillary wall or proliferation of mesangial cells is usually accompanied by microhematuria. Infiltration by inflammatory cells may result in the formation of necrosis lesions with glomerular crescent formation associated with rapid progressive GN with acute renal failure.
PU of less than 2 g daily is usually asymptomatic. Severe PU of more than 3 g daily results in the pattern of damage known as nephrotic syndrome, which, in addition to PU, is characterized clinically by edema of the dependent portions and laboratory chemically by hypoalbuminemia and hyperlipidemia. This condition is often accompanied by hypercoagulability with increased risk of leg and renal vein thrombosis with consecutive pulmonary emboli. Common causes of nephrotic syndrome in adults are diabetic nephropathy, focal segmental glomerulosclerosis (FSGS), and membranous nephropathy.
The pattern of damage in nephritic syndrome is characterized by hematuria, oliguria, arterial hypertension, and renal insufficiency. Diseases that may present with a nephritic syndrome include IgA nephropathies, infectious and postinfectious GN, lupus nephritides, and ANCA-positive and -negative small vessel vasculitides. ANCA-associated GN with crescents or anti-glomerular basement membrane-associated GN can lead to rapidly progressive loss of renal function.
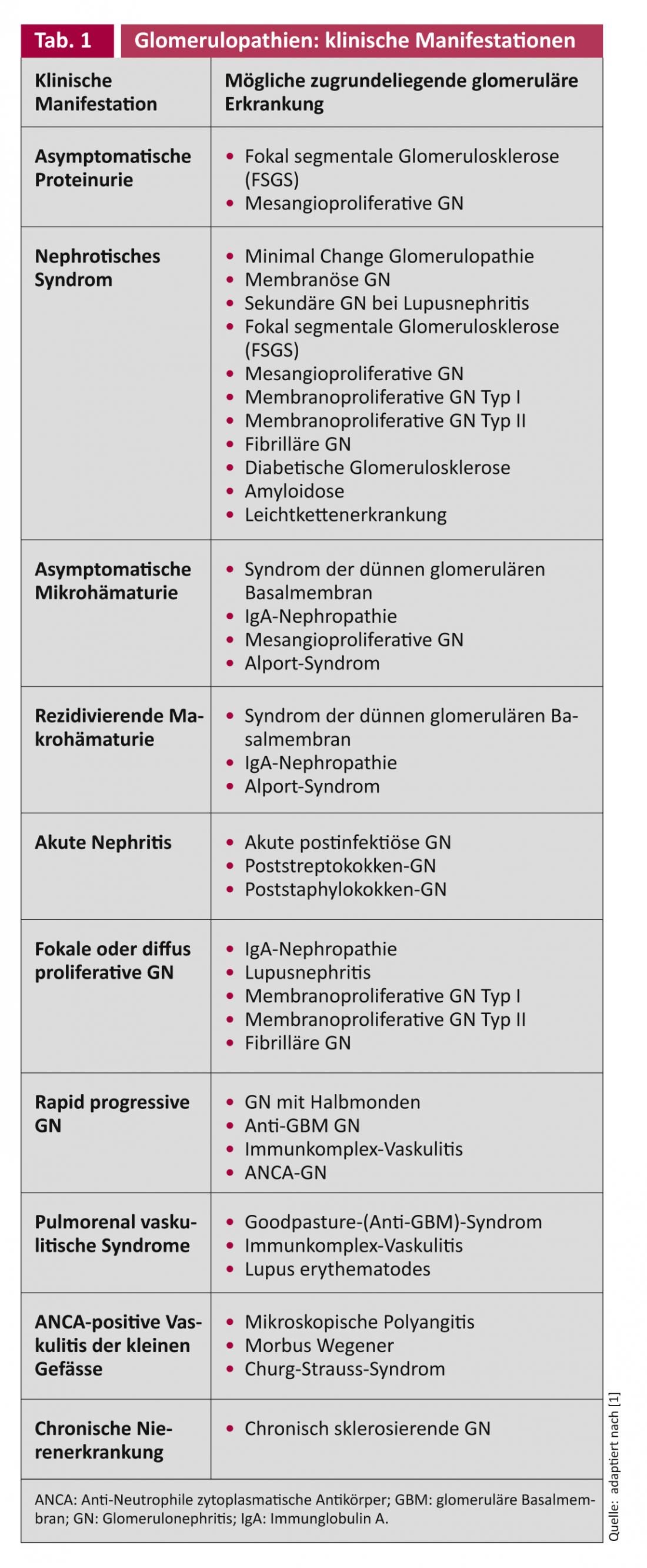
Although GN exhibit features of both nephrotic and nephritic syndromes to varying degrees, there is often a dominant pattern of damage. However, since the same glomerular disease may manifest itself clinically in different ways and, on the other hand, the same clinic may be caused by different glomerular diseases (Table 1) , in adults often only a renal biopsy leads to the elucidation of the specific glomerular pathology. If glomerular disease remains undiagnosed and thus untreated, it may develop into chronic GN with sclerosed glomeruli, interstitial fibrosis, and renal atherosclerosis with mildly impaired to predialytic renal failure. Therefore, when evaluating the renal biopsy, it is important to determine whether the lesion is active and still potentially responsive to specific therapy or whether the damage is already chronic and thus irreversible and not amenable to therapy [1].
Screening for glomerular pathologies.
Patients with glomerular damage usually present to their primary care physician with nonspecific symptoms and signs such as headache, fatigue, nausea, shortness of breath, or swollen legs. In addition to the medical history and physical examination, blood pressure should always be measured, because arterial hypertension often manifests as an early clinical sign of glomerular disease. Laboratory tests aid in the early detection, verification, and gross classification of renal disease. For this purpose, serum creatinine, urea, sodium, potassium, calcium, phosphate, uric acid and total protein are determined. In addition, a blood count and urinalysis using urine sticks and, if possible, a simple microscopic sediment evaluation (“small man biopsy”) are needed. However, in cases of urgent suspicion, there should be no delay due to a laboratory result that is not readily available, as a rapidly progressive form of kidney disease may be present. Here, it is necessary to point out the value of an orienting examination by means of urine sticks, which is available immediately.
A marked serum creatinine increase over a few days to weeks with significant loss of renal function is characteristic of rapid progressive GN. After a postrenal cause could be excluded sonographically, timely nephrological care should always be sought in this case in order to perform renal-specific examinations and interventions to preserve or regain as much renal function as possible.
Detection and quantification of a PU are of great importance for the detection and assessment of a GN. In the case of pathological findings, a urine examination using test strips should be followed by a quantitative protein and creatinine determination in a spot urine with determination of the protein-creatinine ratio (= total protein [g/l]) / Creatinine [mmol/l]; Norm: <0.030 g/mmol), which can be easily performed in any family practice and is not influenced by the level of fluid intake or urine volume. If the strip test is positive but the quantitative evidence of PU is unremarkable, a difference in urine concentration may have caused the detection limit to be undershot and should be checked. However, if the urine stix is negative and protein detection is present in total protein, urinary monoclonal light chain excretion (Bence-Jones PU) must be considered. In patients with diabetes mellitus, detection of microalbuminuria in morning urine (norm: <20 mg/l) is the most sensitive screening parameter for the presence of diabetic nephropathy. It is sometimes difficult to differentiate microalbuminuria as an expression of endothelial dysfunction, indicating increased cardiovascular risk, from incipient glomerular disease. Therefore, if microalbuminuria is detected, all available clinical signs must be used to make the differential diagnosis.
PU is subject to fluctuations during the day due to physical activity and posture, among other factors. Nevertheless, it has been shown that a morning spot urine measurement of protein and creatinine is equivalent to a 24-h collection for the determination of PU [2].
First-detected asymptomatic hematuria without other signs of nephritic or nephrotic syndrome initially requires control. Recurrent asymptomatic hematuria is caused by glomerulopathy in only about 10% of cases; much more often, the hematuria is due to postrenal pathology of the urinary tract. Erythrocytes of glomerular origin are probably present when the proportion of dysmorphic forms in the microscopic examination of the urine is one third or more. In the presence of glomerular erythrocyturia or even to exclude it and in the case of unclear recurrent hematuria, nephrological co-management should be performed, since various non-inflammatory glomerulopathies may also be present, such as thin glomerular basement membrane syndrome, which is usually benign, or Alport syndrome, a congenital defect of the α-chain of type IV collagen of the basement membranes of the inner ear and kidney. The latter is clinically conspicuous in childhood or even in adulthood by micro- or macrohematuria and bilateral sensorineural hearing loss, and a majority of affected individuals develop PU into the nephrotic range and progressive renal insufficiency.
Therapy recommendations
Treatment can be assigned to differential therapy in GN forms without identifiable secondary triggers based on histology. The situation with secondary forms is more complex, because here weighted on the one hand the triggering disease should be controlled, on the other hand in certain situations a sufficient anti-inflammatory treatment must control the secondary inflammatory process to preserve renal function. Of importance is always the therapy of the underlying disease, if known and treatable, such as adequate glycemic control in diabetic nephropathy by the primary care physician or treatment of hepatitis C in membranoproliferative GN by the hepatologist.
Regardless of the underlying disease, attention should also always be paid to good blood pressure control to minimize progression of glomerular damage in the long term. Based on the available studies, a target blood pressure of 120-140/70-90 mmHg can currently be recommended. Whether patients with glomerular disease and without coronary artery disease would benefit from target blood pressure values <120/70 mmHg is currently unclear because of the paucity of data [3]. It is recommended to let the patients control and document their blood pressure at home, also because then the practice hypertension component is omitted. Blood pressure values measured at home that are within the target range should be objectified by means of a 24-h blood pressure measurement, as this is the only way to exclude a missing day-night drop and a missing dipping.
There is evidence that reduction of microalbuminuria and PU by ACE inhibitors can be used as a surrogate marker of further nephroprotection. In case of intolerance to ACE inhibitors, angiotensin receptor blockers (ARBs) can be used as an alternative. Dual inhibition of the renin-angiotensin-aldosterone system with ACE inhibitors and ARBs should be reserved for only the most severe PU and may lead to accelerated renal function loss [4]. The same applies to the combination of the renin inhibitor aliskiren with an ACE inhibitor or ARB, which in patients with diabetes or impaired renal function with a glomerular filtration rate of <60ml/min/1.73 m² is contraindicated, as studies indicate an increased risk of developing hypotension, syncope, stroke, hyperkalemia, and worsening renal function, including acute renal failure. For other patient groups, adverse consequences of an appropriate combination therapy cannot be excluded.
Nephrotic edema is treated diuretically, with attention to the increased risk of thrombosis. If excessive salt intake exists or edema remains refractory to therapy, sodium restriction must be performed. Diuretic resistance” can be overcome by combining loop diuretics with thiazide diuretics, if necessary even combined with spironolactone.
In the presence of prolonged hyperlipidemia, as is often the case in patients with nephrotic syndrome, the use of a statin should be considered. Hypoalbuminemia of <25 g/l is considered a surrogate marker of increased thrombogenic risk in nephrotic PU, so anticoagulation should be instituted. There are nephrology guidelines, known as the “KDIGO Guidelines,” that should be consulted when accurately adjusting anticoagulation [5]. Evaluation and initiation of therapy in secondary hyperparathyroidism due to already significantly impaired renal function as well as in renal anemia should be performed by the nephrologist.
Conclusion for practice
- Nephrotic syndrome is characterized by severe proteinuria (PU) of >3 g/24 h and is associated with edema, hypoalbuminemia, hyperlipidemia, and increased thromboembolic risk.
- Nephritic syndrome is characterized by hematuria, oliguria, arterial hypertension, and renal insufficiency and may characterize rapid progressive GN.
- Glomerular damage is accompanied by nonspecific symptoms and signs. The screening of renal pathologies by general practitioners therefore always includes blood pressure measurement as well as examinations of blood chemistry, blood count and urine.
- Referral to a nephrologist should include evaluation for renal insufficiency, recurrent hematuria, and PU and suspected presence of renal hypertension.
- If serum creatinine rises rapidly as a sign of renal function loss and sonographic exclusion of a postrenal cause, renal function must be preserved or recovered by prompt nephrologic diagnosis and therapy.
- Regardless of the underlying disease, the therapy of glomerular disease always includes the adjustment of blood pressure around 120-140/70-90 mmHg according to current studies and the objectification of blood pressure by means of 24-h blood pressure measurement.
Nasser Dhayat, MD
Prof. Dr. med. Markus Mohaupt
Literature:
- Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO Clinical Practice Guideline for Glomerulonephritis. Chapter 2: General principles in the management of glomerular disease. Kidney inter Suppl 2012;2:139-274.
- Price CP, et al: Use of protein:creatinine ratio measurements on random urine samples for prediction of significant proteinuria: a systematic review. Clin Chem 2005;51:1577-1586.
- Current guidelines for the treatment of arterial hypertension of the Deutsche Hochdruckliga e.V. DHL, update 2011, last update: 16.11.2011. www.hochdruckliga.de/tl_files/content/dhl/downloads/DHL-Leitlinien-2011.pdf
- Volpe M, et al: Inhibition of the renin-angiotensin-aldosterone system: is there room for dual blockade in the cardiorenal continuum? J Hypertens 2012;30:647-54.
- Jenette JC, Falk RJ: Glomerular Clinicopathologic Syndromes. In: Greenberg A (ed.): Primer on Kidney Diseases. Philadelphia: Elsevier Saunders, 2009:149.
CARDIOVASC 2012; no. 5; 6-10.