A fundamental factor in the field of cardiology is LDL cholesterol. Because without cholesterol, there is no atherosclerosis. Therefore, effective lipid management is paramount for the prevention of cardiovascular events. The new ESC guideline has incorporated the latest evidence into its recommendations. However, intensive research continues to enable new treatment options in a timely manner.
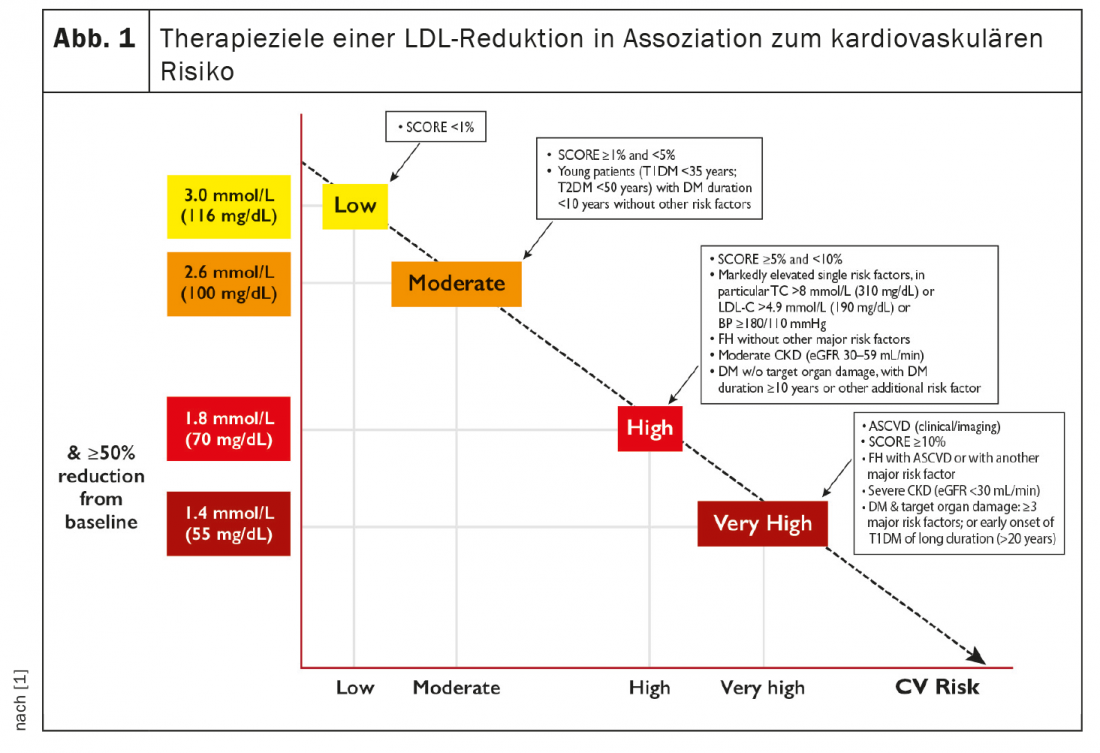
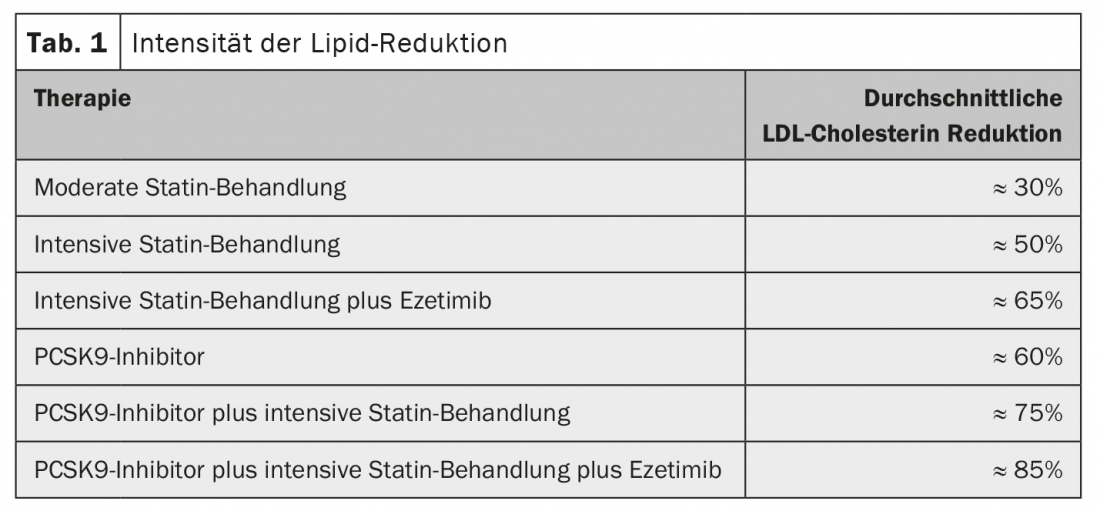
Intensive research efforts in recent years have established a clear link between LDL cholesterol and cardiovascular disease. Accordingly, LDL-C is a significant factor in the development of atherosclerosis. This has now been addressed by the new ESC guidelines for lipid management presented by Prof. François Mach, MD, Geneva. The guideline advocates significant LDL-C lowering with statins, ezetimibe, or PCSK9 inhibitors to <1.4 mmol/L (55 mg/dL) in patients at very high risk. This is because clinical studies have clearly shown that without a lower limit for LDL-C levels, the lower the LDL-C levels achieved, the lower the risk of future cardiovascular events. Intensification of therapy should be based on risk and baseline LDL cholesterol (Fig. 1) . For this, cardiovascular risk is defined, target LDL parameters are set, and the best lipid-lowering strategy is chosen. Depending on the therapy strategy, a reduction of between 30% and 85% can be achieved (Tab. 1) . The new therapy concept also provides for an early start, significantly more aggressive treatment and the use of combination therapies.
Focus Lipoprotein(a)
Lipoprotein(a) (Lp[a]) combines proinflammatory, prothrombotic, and proatherogenic properties and is closely associated not only with atherosclerosis but also with aortic stenosis. However, with respect to the frequency distribution of cardiovascular risk, there is no normal Gaussian curve but an extreme leftward shift. The vast majority have serum concentrations below 20-30 mg/dl. Only a few people have very high concentrations, but these are then associated with a very high risk. An Lp(a) >50 mg/dl indicates increased cardiovascular risk. Elevated levels can be lowered with antisense oligonucleotides, lipoprotein apheresis, or even PCSK9 inhibitors. The focus is primarily on optimal LDL-C reduction. New RNA drugs are currently in clinical trials.
A look into the future
Currently, intensive research is being conducted on molecular therapeutic options for dyslipidemias. Already well advanced in development is the possibility of PCSK9 siRNA, which appears to be interesting mainly because of the application form required only twice a year. An average reduction in LDL-C of 52% was observed over an 18-month period. Safety data to date are very promising. Currently, there are no indications of liver or kidney problems or muscular side effects. In addition, there are development programs that address ANGPLT3 as well as Apo-CIII. Genetic studies have clearly shown that these proteins are causal for the development of coronary heart disease.
Source: DGK 2020
Literature:
- 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to rescue cardiovascular risk. European Heart Journal 2020; 41: 111-188.
CARDIOVASC 2020; 19(4): 28 (published 10/12/20, ahead of print).