Anaphylactic reactions are among the most severe and potentially life-threatening dramatic events in allergology. Acute treatment is provided based on international guidelines and textbook recommendations. The updated guideline also takes into account previous versions as well as international guidelines and includes a paragraph on the issue of allergy and COVID-19.
In recent years, there has been increasing worldwide data collection on the incidence of anaphylactic reactions. Retrospective studies suggest that up to 1-2% of those affected by anaphylaxis present to a maximum care hospital emergency department for anaphylactic reactions. Anaphylaxis-related deaths are estimated at one to three cases per year per million population. Figures from the German-language Anaphylaxis Registry show that food is the most common trigger of anaphylaxis in childhood. Insect venoms and pharmaceuticals are the most common triggers in adults in Germany, although there are international differences in the order of these triggers. In childhood, boys are more frequently affected by anaphylaxis than girls, probably due to the more frequent occurrence of food allergies in boys. An equalization of the sex distribution is found after puberty.
Immune globulin E-mediated allergy most common
The cause of anaphylaxis is usually an immunological reaction. IgE thereby activates mast cells and basophilic granulocytes via cross-links of high affinity IgE receptors, which is indirectly measurable in an increased expression of surface markers (CD63, CD203c) on basophils. The symptoms of anaphylactic reactions are particularly caused by mediators released mainly from mast cells and basophilic granulocytes such as histamine, prostaglandins, leukotrienes (LTB4, LTC4, and LTD4), tryptase, platelet-activating factor (PAF), heparin, proteases, serotonin, and cytokines.
The same disease with different effects
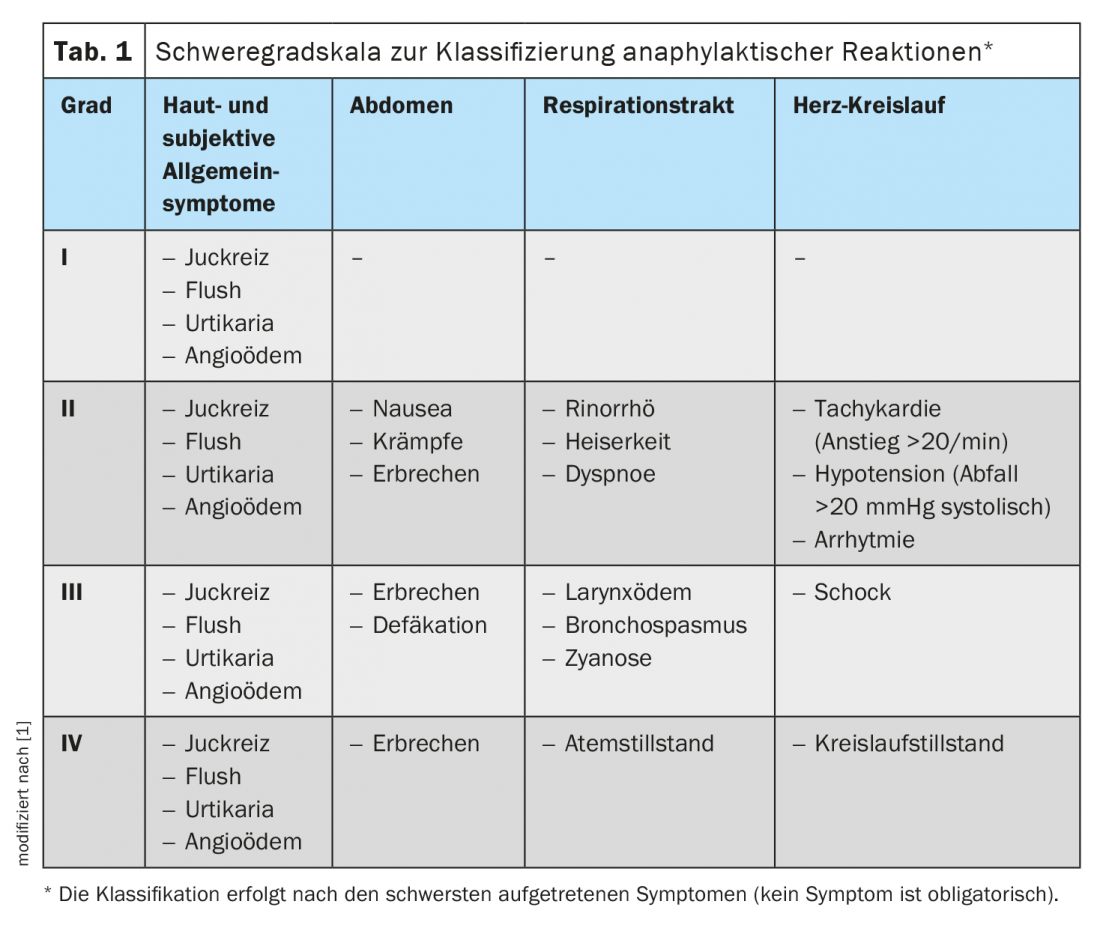
Anaphylactic reactions manifest mainly on the skin, respiratory tract, gastrointestinal tract and cardiovascular system. According to the intensity of the clinical symptoms, anaphylaxis is classified into severity grades from I to IV, as in the previous guidelines (Tab. 1) . The symptoms of anaphylactic reactions usually start acutely and can progress rapidly. Thus, within minutes, symptoms may intensify to the point of shock and death. However, the response may also spontaneously stop at any stage and regress as it progresses. In a Severity I reaction, the further development and dynamics of the reaction are not initially foreseeable. Symptoms may occur in different ways, simultaneously or sequentially. Circulatory reactions may occur primarily without prior cutaneous or pulmonary reactions. In five to 20% of cases, protracted or biphasic courses occur after successful therapy, with renewed symptoms usually after six to 24 hours. In addition to acute onset of symptoms immediately after allergen contact and biphasic courses, primary delayed-onset anaphylactic reactions are also possible, in which symptoms do not begin until hours after exposure. This particular kinetics has been impressively documented, for example, for the allergen galactose-α-1-3-galactose in mammalian meat allergy.
Risk factors of severe anaphylaxis
Certain endogenous and exogenous factors may promote the occurrence of severe anaphylaxis. Such risk factors, which exist independently of the trigger, are advanced age, severe cardiovascular diseases, existing and especially poorly controlled bronchial asthma, the use of certain drugs that promote mast cell activation or leukotriene formation (NSAIDs), and mastocytosis. For example, previous use of β-adrenoceptor antagonists and ACE (angiotensin converting enzyme) inhibitors may lead to an increase in anaphylactic symptoms. In addition, considering the trigger-related subgroups of anaphylaxis, there are data for food-induced anaphylaxis showing that allergic bronchial asthma is also an important risk factor in this case. Ultimately, the trigger itself can also be a risk factor. For example, it is known that primary sensitization to peanut or fish, among other highly potent allergens, is a risk factor for severe reactions.
Emergency therapy should be given promptly and appropriate to symptoms
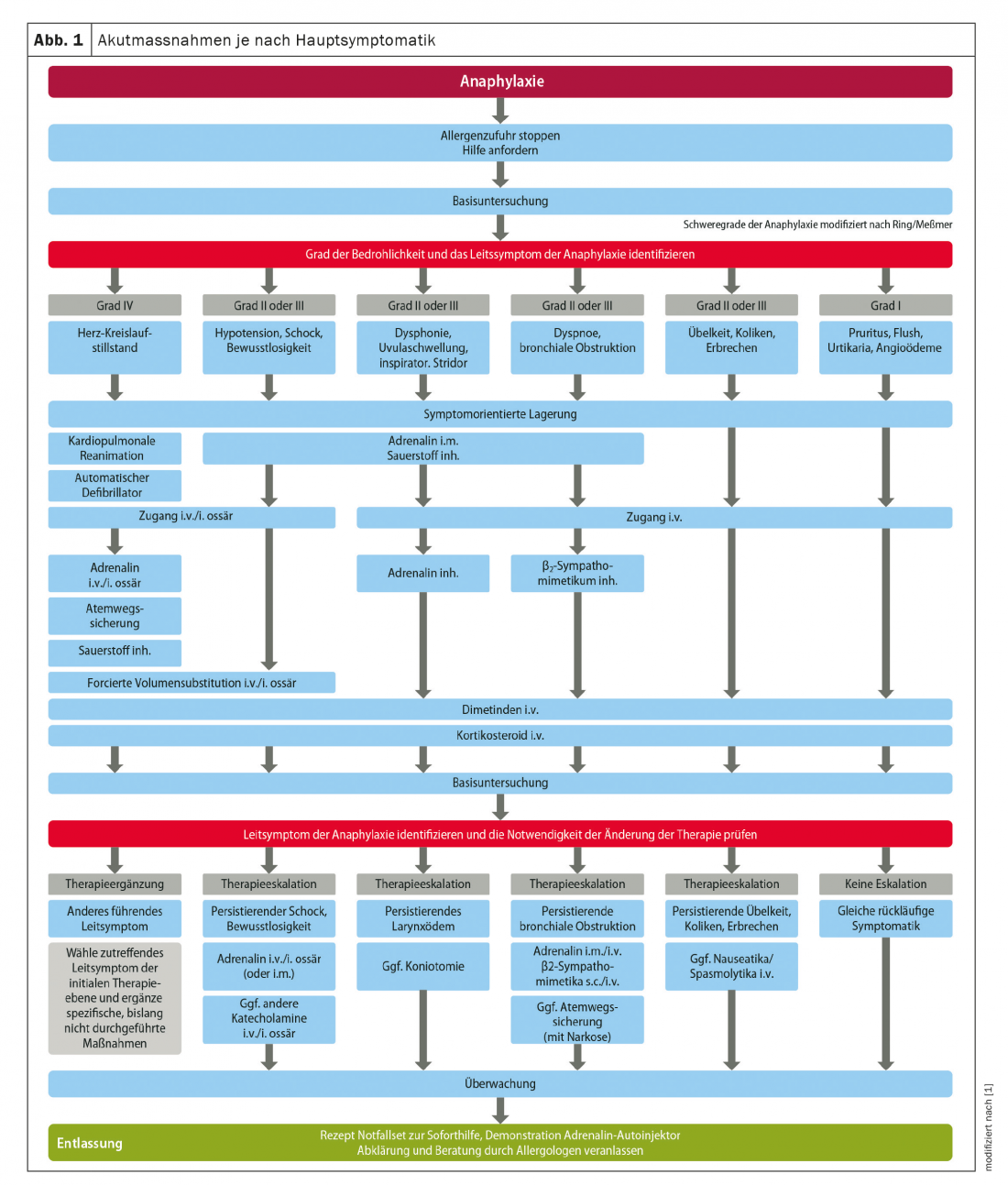
A scheme depicting the therapy for physicians and the emergency team was updated and adapted as part of the update (Fig. 1). There are no changes with regard to pharmacotherapy. The most important drug in the acute therapy of anaphylaxis is still adrenaline (epinephrine), especially the intramuscular application by autoinjector. Dopamine, norepinephrine as well as vasopressin are only used in threatening situations by emergency physicians and under intensive care conditions with monitor control. In case of manifest cardiovascular or pulmonary reactions, immediate application of oxygen via the breathing mask with reservoir bag is recommended. Hypovolemia resulting from anaphylaxis requires adults to receive one to three liters of balanced whole electrolyte solution within a short period of time, depending on the response. In infancy, initial administration of 20 ml/kg bw by hand is given as soon as possible. After reevaluation, further boluses of 20 ml/kg bw are given until hemodynamic stabilization. The central role of histamine as a mediator of allergic reactions and the effects of H1 antihistamines in acute urticaria or rhinoconjunctivitis are undisputed, but their effects on the circulation and bronchoconstriction have not been established. Antihistamines have a slower onset of action compared with epinephrine, but have a favorable benefit/side effect profile and a wide therapeutic range. An effect on the allergic reaction can therefore be assumed. Glucocorticoids, on the other hand, play a minor therapeutic role in the acute phase of an anaphylactic reaction because of the slow onset of their effect.
Don’t forget discharge management!
Discharge management after anaphylaxis has occurred should prevent the risk of a recurrence. This includes the identification of the trigger through allergy diagnostics. For certain IgE-mediated allergies, allergen-specific immunotherapy can be initiated (e.g., insect venoms). Sufficient information includes not only theoretical knowledge, but also practical training. For this purpose, training programs with practical exercises have proven effective, such as those offered by the Arbeitsgemeinschaft Anaphylaxie Training und Edukation (AGATE). Finally, a medicinal “emergency kit for immediate help” is prescribed, which should be carried by the affected person at all times. When prescribing, the “aut idem box” on the GSK prescription should be checked to ensure that the patient also receives the epinephrine autoinjector for which he or she has been trained.
Anaphylaxis after COVID-19 vaccination?
Since vaccination against COVID-19 has been performed, isolated cases of anaphylaxis have been reported from the UK and USA, leading to uncertainty among patients and vaccinators. The Anaphylaxis Guideline Group and allergy societies have commented that certain patients with allergic diseases may be at increased risk for anaphylaxis after COVID-19 vaccination, namely, patients with severe allergic reactions to drugs or vaccines and known hypersensitivity to ingredients of the COVID-19 vaccine used. In unclear cases, allergological clarification should be performed before COVID-19 vaccination. Also, the observation time after vaccination should be 30 minutes for patients at risk. Physicians and medical assistants at vaccination centers should be made aware of the possibility of anaphylaxis and the immediate measures that are then required.
Literature:
- Ring J, et al: Guideline (S2k) on acute therapy and management of anaphylaxis: 2021 update. Allergo J Int 2021(30): 1-25; https://doi.org/10.1007/s40629-020-00158-y.
HAUSARZT PRAXIS 2022; 17(6): 35-37











