Personalized immunotherapy is on track to replace chemotherapy in first-line non-small cell lung cancer. However, this only works for every second patient. Chemo vs. immuno-oncology – who will win the race in the future?
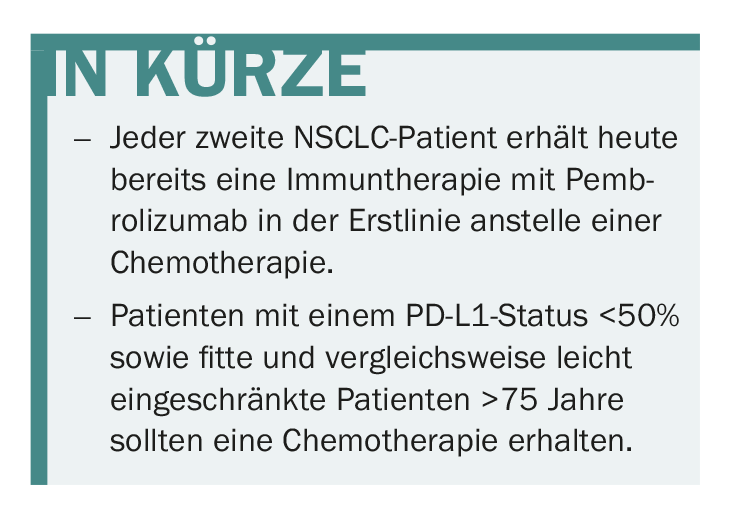
Already, about 50% of patients with NSCLC are no longer treated with standard first-line chemotherapy, but receive targeted therapy with pembrolizumab. The introduction of first-line immunotherapy is considered a major breakthrough in the treatment of lung cancer. For example, the use of pembrolizumab increased patients’ median progression-free survival (mPFS) by 4.3 months to now 10.3 vs. 6 months with chemotherapy. The KEYNOTE-024 pivotal trial also showed that overall survival increased to 30 months with pembrolizumab compared with 14.2 months with chemotherapy.
Nevertheless, it should be noted that PD-L1 status matters for the effect of pembrolizumab in first-line lung cancer. While patients with more than 50% PD-L1-positive tumor cells benefited from first-line pembrolizumab, patients with less than 50% PD-L1-positive cells are still more likely to benefit from first-line chemotherapy.
Current combination therapies under test
After these first noticeable successes of immunotherapy, it will be interesting to see in the future whether combination therapies including an immunotherapeutic agent can further enhance the effects or make immunotherapy equally accessible to people with insufficient PD-L1 expression. In the KEYNOTE-021 trial, the combination of pembrolizumab and chemotherapy proved superior to chemotherapy alone, increasing progression-free survival by 4.1 months, for example. In contrast, the IMpower-150 trial evaluated the interaction of chemotherapy plus immunotherapy and angiogenesis inhibitor, which ultimately provided patients with a progression-free survival benefit of up to 8.3 months compared with chemotherapy alone. Equally promising seems to be the combination of two immunotherapeutics – nivolumab and ipilimumab – and this independent of the PD-L1 status of the patients, as the current CheckMate-012 study showed.
The medium-term goal is clear from these different efforts: chemotherapy should move further back in the treatment regimen for NSCLC or even be used in combination with immunotherapy. The hope of oncologists is to be able to abandon the extremely toxic chemotherapy altogether sooner rather than later – at least in the first-line treatment of lung cancer.
Patient age matters
However, with the use of immunotherapy, another question is coming into focus: What role does a patient’s age play in the treatment decision? This is not a trivial matter, because older patients over the age of 65 undergo a whole series of physiological changes, including the process known as immune senescence. If the immune system naturally decreases in activity in old age, the question arises whether immunotherapy for older patients can be successful at all.
Chemotherapy as a systemic treatment approach is already well studied in older NSCLC patients and its evidence is sufficiently supported by studies. For immunotherapy, however, the data situation is still insufficient. Nevertheless, a few studies indicated that elderly patients >75 years had no measurable survival benefit and thus did not benefit from immunotherapy. Therefore, until further notice, the recommendation is that primarily fit and comparatively mildly impaired elders above the age of 75 should be offered chemotherapy. Patients in this age group are very unlikely to benefit from immunotherapy. Ultimately, however, the therapy decision is made jointly by the patient and the physician.
Does it all add up?
The cost of immunotherapy with pembrolizumab is offset by a response rate of approximately 20% and a lifetime gain in the unselected patient population of approximately three months. The question of cost-effectiveness in the first-line setting certainly arises. The consequence can only be to always select patients in advance according to the respective PD-L1 status and to personalize the therapy based on this. In this case, for example, patients benefit from longer survival with significantly better quality of life compared to chemotherapy.
Source: 33rd German Cancer Congress, February 21-24, 2018, Berlin.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(2): 3.