In pulmonary hypertension, the pulmonary vessels are narrowed or blocked. This can lead to increased stress on the right ventricle and ultimately insufficiency. However, diagnostics are not always given the care that is needed. Even a moderate increase has a negative impact on the prognosis of those affected.
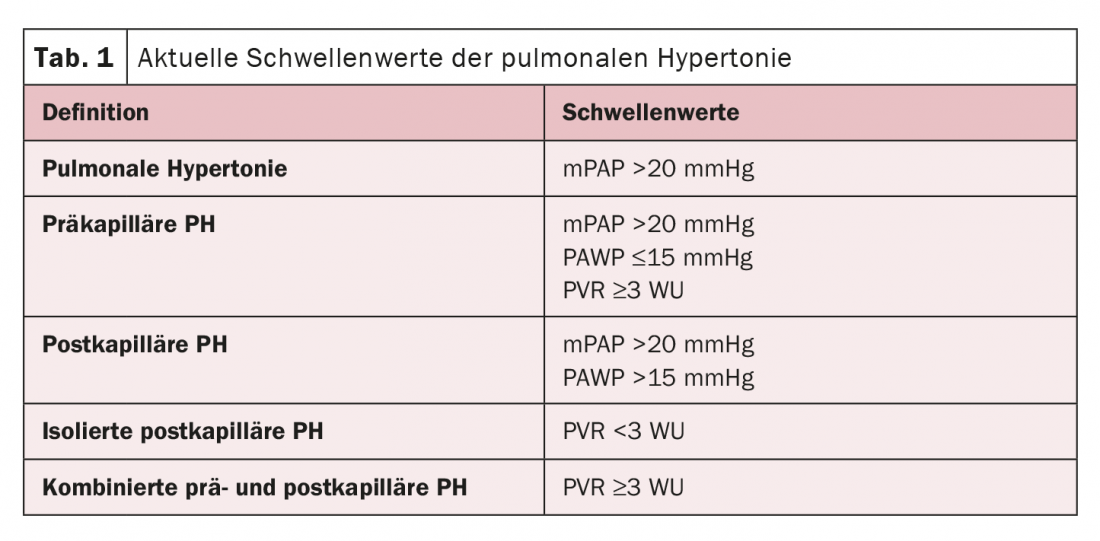
If pulmonary hypertension (PH) is also suspected, an echocardiographic examination is usually performed in the clinical setting. However, the underlying cause often cannot be visualized, warned Prof. Stephan Rosenkranz, MD, Cologne (D). The right heart catheter is then needed to define the disease. Regarding thresholds, there has been a recent proposal from the World Symposium that may be incorporated into the new ESC/ERS guidelines expected in the fall (Tab. 1). The rationale for lowering the threshold is that there is a correlation with mortality and hospitalization even at a moderate increase. Several study results have shown that even a small increase in pressure from any cause is significant for patients, the expert said. These findings currently have no implications for the treatment of arterial PH. This is because the studies on the efficacy and safety of PH medications available to date have been performed with the threshold ≥25 mmHg. In clinical practice, PH patients usually present with significantly higher values anyway. The gray area between 20 mmHg and 25 mmHg, which seems to be prognostically relevant, only comes into play in special patient groups.
However, the importance of right heart failure even in moderate pressure elevation cannot be dismissed. Systemic congestion as a result of hemodynamic changes and RVLV interaction with often decreased systemic output then come into play. Both have a great influence on many other organ systems.
High-quality measurements as a basis
The right heart catheter examination is the basis of further therapeutic procedures and should be performed in a high quality. The quality of hemodynamic measurements in particular often leaves much to be desired, the expert emphasized. In this context, pressure measurement alone is not enough. The other parameters in the pulmonary stroma must also be recorded. In addition to measured parameters, calculated parameters are also included, which are also important for patient prognosis. These include, for example, the transpulmonary gradient (TPG) as the difference between PAPm and PAWP, and transpulmonary resistance (PVR). Further, the diastolic pulmonary gradient (PAPd-PAWP) and pulse pressure (PAPs-PAPd) are considered. With regard to treatment decision, PAWP measurement is crucial for distinguishing pre-capillary from post-capillary PH.
A comprehensive study also took a closer look at pulmonary resistance. It was shown that the threshold value of >3 WU is very likely too high. The results demonstrate that a PVR >2.1 WU is associated with an increased risk of mortality.
Source: Pulmonary Hypertension – New Aspects from Different Perspectives, Working Group Meeting, 04/20/2022, 1:30-15:00 p.m.
Congress: 88th Annual Meeting of the German Society of Cardiology (DGK)
CARDIOVASC 2022; 21(2): 22