A new molecular genetic classification of gastric cancer into four subtypes was recently proposed as part of the Cancer Genome Atlas project, which identifies all gene defects in all known cancers. This typing should enable new approaches for targeted molecular-based therapies in the future. New therapeutic options were discussed at the annual meeting of the German, Austrian and Swiss Societies for Hematology and Medical Oncology.
(as) Gastric carcinoma is associated with a poor prognosis. Little has changed in this regard in recent years. Despite advances in diagnostic techniques, over 80% of tumors are not detected until advanced stages. However, 2014 may herald a paradigm shift in the understanding of the disease: Gastric cancer, previously treated as a single entity, is emerging as a genetically complex disease with multiple molecular genetic subtypes.
Four subtypes
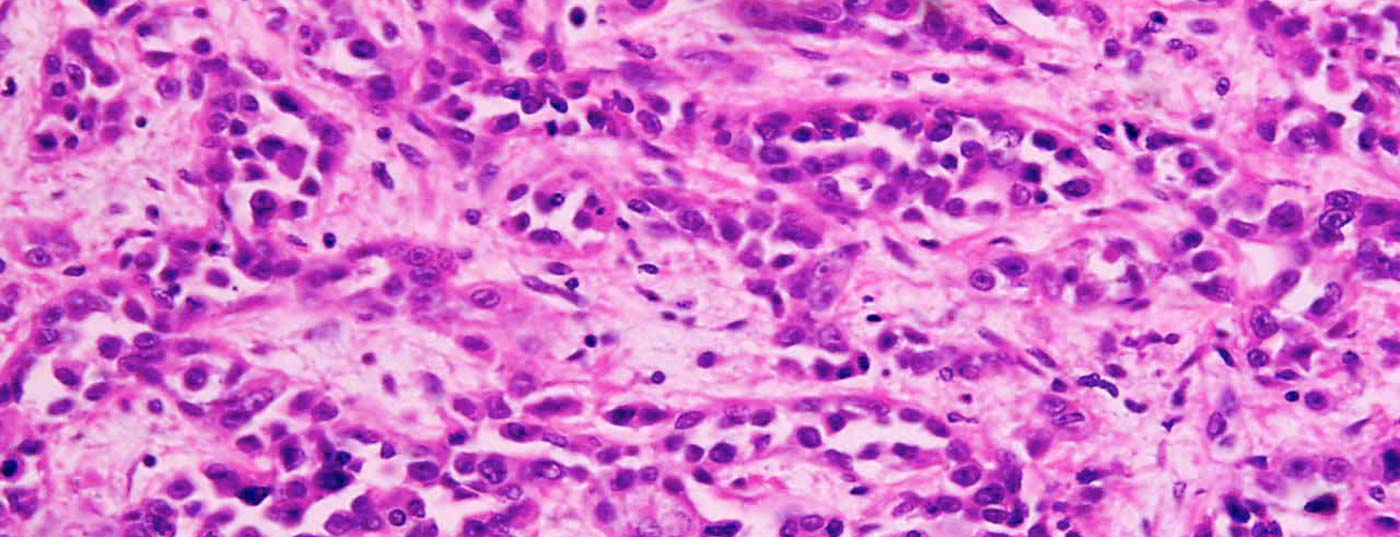
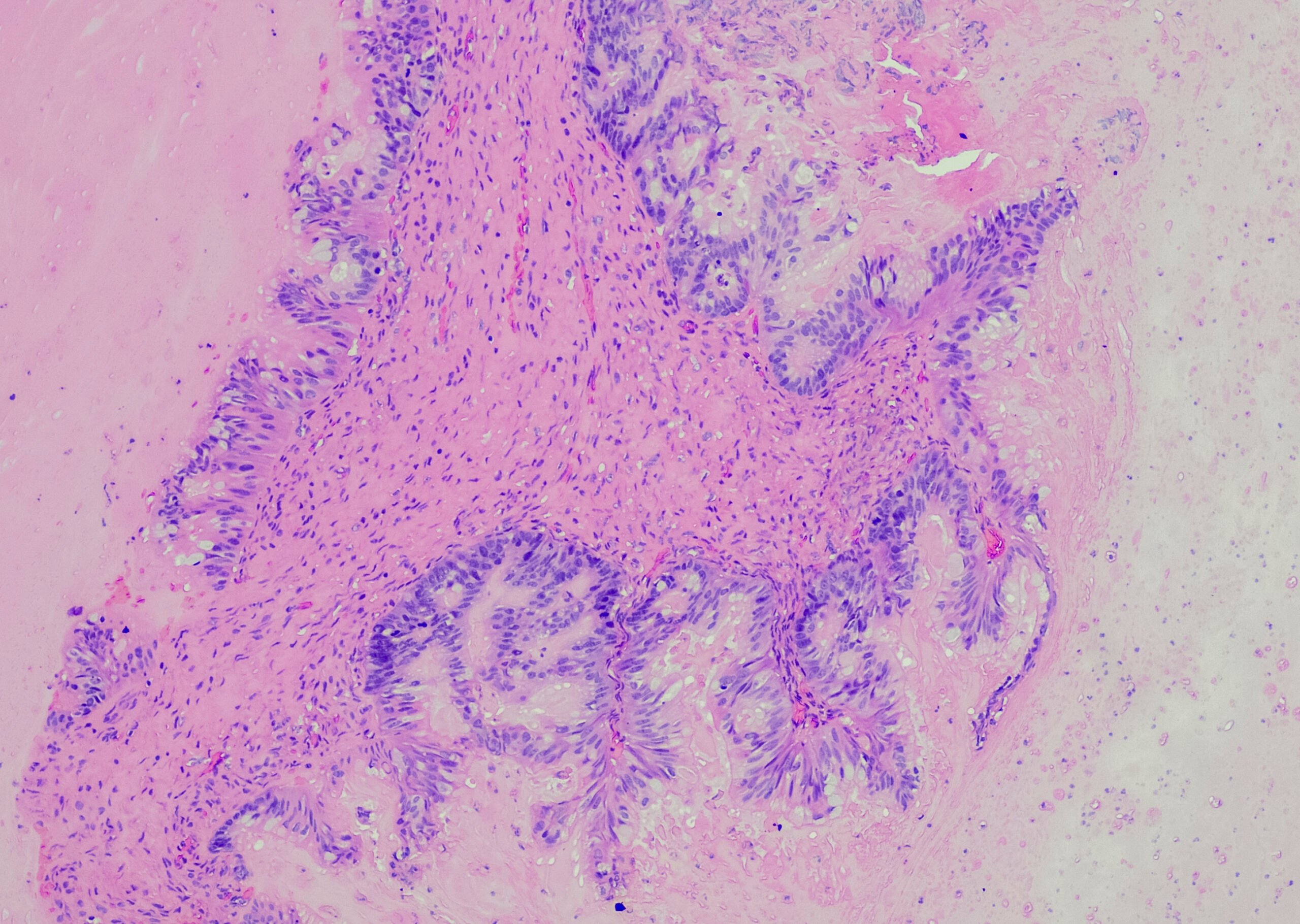
The classification of gastric carcinoma based on tumor location or histology (adenocarcinoma at the esophagogastric junction, fundus, corpus, or antrum) is now completed by molecular genetic classification, reported Prof. David Cunningham, London. Researchers from the Cancer Genome Atlas Research Network had molecularly analyzed biopsies from 295 untreated gastric cancer patients for DNA methylation status and sequenced messenger RNA and micro RNA to determine which genes and key proteins were involved in each cancer cell. The results, recently published in Nature, suggest a classification into four subtypes [1].
In the first subtype, Epstein-Barr virus (EBV) and mutations in the metabolic pathway of the oncogene PIK3CA were detected. EBV is detectable in about 9% of gastric cancer tumor cells; it may promote carcinogenesis in cooperation with the gastric germ Helicobacter pylori. The second subtype, MSI, is characterized by the presence of microsatellite instability. The third subtype, GS, is characterized by genomic stability with diffuse histology and is accompanied by specific mutations. The fourth subtype, CIN, is characterized by chromosomal instability and occurs in 50% of all cases. What relevance this classification will have in the selection of therapy in the future is not yet foreseeable, Cunningham said.
Surgery alone is not enough
Accurate staging is essential in the treatment of gastric cancer. Even localized tumors are treated multimodally. Since the majority of tumors are diagnosed at an advanced stage, neoadjuvant and adjuvant therapeutic approaches are necessary for resectable gastric carcinomas in addition to surgical therapy. In the UK MAGIC trial of 503 patients with operable gastric cancer, the group led by first author Cunningham showed that perioperative chemotherapy with epirubicin, cisplatin, and 5-fluorouracil significantly improved overall survival at five years from 23 to 36% [2]. This corresponds to a 13% increase in 5-year survival. “Even with optimal surgical care, however, the risk of microscopic dissemination remains,” Cunningham said. “The patient’s prognosis depends on staging after neoadjuvant chemotherapy.”
New algorithms and tumor pathways
In metastatic gastric cancer, chemotherapy prolongs survival and improves symptom control, reported Prof. Florian Lordick, MD, Director of the Leipzig University Cancer Center. Combination therapy consisting of a platinum derivative and a fluoropyrimidine has been shown to be superior to monotherapy. The less toxic oxaliplatin can be used instead of cisplatin, and oral capecitabine is used instead of intravenous 5-FU. In some countries, a three-drug combination with docetaxel or epirubicin is used – but this is associated with increased toxicity and is not recommended, the expert said.
In recent years, the molecular perspective has been added to the treatment of gastric carcinoma: Instead of treating carcinomas based solely on tumor location, molecular biology insights into specific tumor pathways help guide treatment decisions. In approximately 15 -20% of cases, HER2 overexpression can be detected in gastric carcinoma, similar to breast carcinoma. In a study of 594 HER2-positive gastric cancer patients in whom the disease had already metastasized, the monoclonal antibody trastuzumab in combination with cisplatin and a fluoropyrimidine prolonged survival from 11 to 16 months [3].
Tumor stabilization as the goal of second-line therapy
Lordick described ramucirumab, a monoclonal antibody that targets vascular endothelial growth factor receptor 2 (VEGFR2), as an advance in quality of life for patients with metastatic gastric cancer. The angiogenesis inhibitor is the first monoclonal antibody for the treatment of patients with advanced gastric cancer. The compound is considered as monotherapy for patients who experience tumor progression after first-line therapy. In this group of patients (n=355), treatment with ramucirumab versus “best supportive care” had prolonged median overall survival from a median of 3.8 to 5.2 months [4]. No new toxicities or side effects had occurred.
Source: Advanced Training Gastric Carcinoma, Annual Meeting of the German, Austrian and Swiss Societies for Hematology and Medical Oncology (DGHO), October 12, 2014, Hamburg (D).
Literature:
- The Cancer Genome Atlas Research Network: Comprehensive molecular characterization of gastric adenocarcinoma. Nature 2014 Sept; 513: 202-209.
- Cunningham D, Allum WH, Stenning SP, et al: Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006; 355(1): 11-20.
- Bang YJ, et al: Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 2010; 376(9742): 687-697.
- Fuchs CS, et al: Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 2014; 383(9911): 31-39.
InFo ONCOLOGY & HEMATOLOGY 2014; 2(10): 27-28.