One study suggests that patients with low HR-positive/HER2-negative tumors could be considered and treated similarly to patients with triple-negative tumors. Should the current definitions of HR positivity and their clinical relevance therefore be reconsidered?
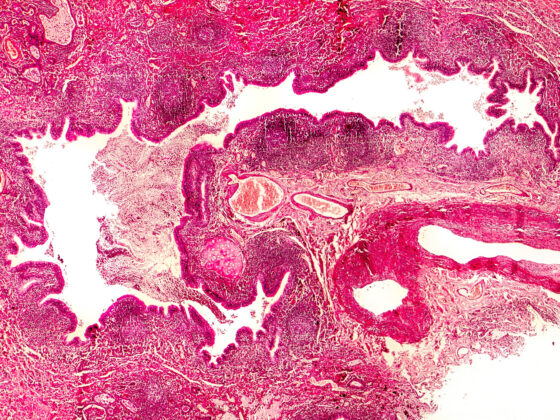
The treatment of breast cancer with low HR positivity is not clearly defined in the guideline. Various studies have shown that they are closer to ER/PgR-negative or triple-negative breast carcinomas (ER-, PgR and HER2-negative) in terms of tumor biology and prognosis than ER-positive (> 10 % positive tumor cells). Therefore, based on a population-based 15-year cohort, patient characteristics and the outcome of low-positive HR tumors were compared with HR-negative or strongly positive HR tumors. A total of 38,560 women who were diagnosed with early invasive breast cancer between 2004 and 2018 as part of the Munich Cancer Registry (MCR) with 4.9 million inhabitants were included. Descriptive analyses of prognostic factors, treatment and outcome analyses according to the Kaplan-Meier method, cumulative incidence taking into account competing risks, and multivariate analyses (Cox regression and Fine-Gray model) were performed.
861 patients (2%) had a weakly positive, 4862 (13%) a negative and 32,837 (85%) a strongly positive HER2 tumor. Within the HER2-negative cohort, the survival of HR-low-positive tumors was significantly worse than that of HR-strong-positive tumors, while no significant difference in survival was found between HR-low-positive and HR-negative tumors. The analyses for time to local recurrence, time to lymph node recurrence and time to metastasis showed similar results. In contrast, no statistically significant differences between the three HR groups were found in the HER2-positive cohort in the multivariate analyses. Regardless of HER2 status, patients with low HR-positive tumors do not appear to benefit significantly from endocrine therapy. The authors conclude that the current definitions of HR positivity and their clinical relevance should be reconsidered and that patients with low-positive HR status with HER2 negativity should be classified and treated similarly to patients with triple-negative tumors.
Current therapy management at a glance
For a long time, the treatment of early breast cancer was based on a histopathological classification of subtypes. It has now become clear that breast cancer in BRCA germline mutation carriers is a biologically distinct entity. Histologically, over 80% of breast carcinomas in these patients are classified as invasive ductal. The biology of the BRCA-mutated tumor cell offers an approach for targeted therapies, as BRCA1 and -2 mutations increase the effectiveness of PARP inhibitors. PARP (poly-[ADP-Ribose-]polymerase) inhibitors disrupt DNA repair mechanisms, for example after chemotherapy.
Basically, treatment management with a molecular biological approach targets ligands, blocks binding sites of their receptors or inhibits signaling pathways within the cells. The development of targeted active substances has been very dynamic in recent years. Several targeted active substances are currently available:
- HER2 antibodies
- Antibody-drug conjugates coupled to HER2 antibodies or TROP2 antibodies
- Tyrosine kinase inhibitor
- mTOR inhibitors
- CDK4/6 inhibitors
- VEGF antibodies
- PI3 kinase
- PARP inhibitor
- Immune checkpoint inhibitors
Literature:
- Schrodi S, Harbeck N, Mahner S, et al.: Outcome of breast cancer patients with low hormone receptor positivity: Analysis of a 15-year population-based cohort. DKK Abstract #114, Oncol Res Treat 2022; 45 (suppl 1): 5. DOI: 10.1159/000521004
- Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF): S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Mammakarzinoms, Version 4.4, 2021, AWMF
Registernummer: 032–045OL, www.leitlinienprogramm-onkologie.de/leitlinien/mammakarzinom (letzter Zugriff am 06.12.2023) - www.onkopedia.com/de/drug-assessment/guidelines/olaparib-lynparzatm-mammakarzinom-der-frau-mammakarzinom-des-mannes-brca-mutiert-adjuvant/@@raw/addendums/nutzenbewertung.pdf (letzter Zugriff am 06.12.2023)
- www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/krebsarten/brustkrebs/therapie/molekularbiologische-therapie.html (last accessed on 06.12.2023).
InFo ONKOLOGIE & HÄMATOLOGIE 2023: 11(6): 34