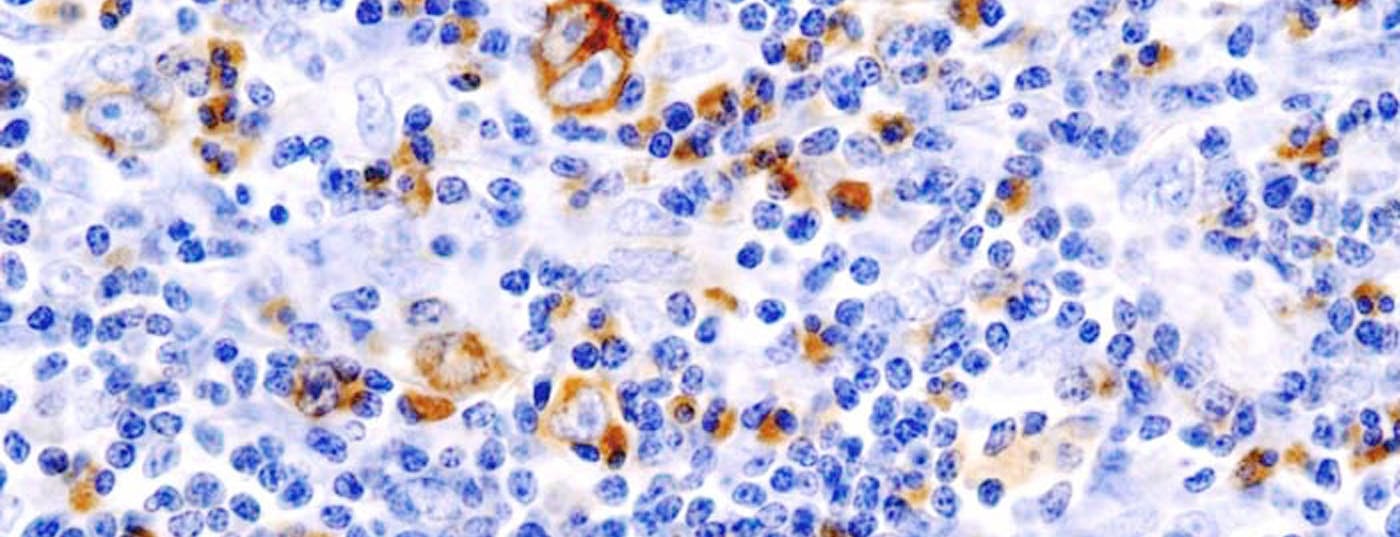
Preclinical studies show that Sternberg-Reed cells, characteristic of classical Hodgkin lymphoma, use the PD-1 pathway to evade immunodetection. Therefore, immune checkpoint inhibitors such as nivolumab, which binds to the PD-1 receptor, may be effective here. Preliminary results from the phase Ib CheckMate 039 study are promising.
(ag) By binding to the PD-1 receptor on activated T cells, nivolumab prevents natural ligands such as PD-L1 and PD-L2 from interacting with the receptor. These ligands are frequently overexpressed in Hodgkin’s lymphoma and are responsible for limiting T cell activation and proliferation. Nivolumab prevents such processes and thus stimulates the immune system in its fight against cancer cells. The compound has shown clinical activity in various solid tumors to date.
Update to CheckMate 039
Preliminary results from a study of 23 patients with relapsed or refractory Hodgkin lymphoma were presented at both the 2014 ASH Congress [1] and in the New England Journal of Medicine [2]. These are the first published analyses on a PD-1 antibody in the treatment of classical Hodgkin’s lymphoma. The hypothesis was that nivolumab increased anti-tumor activity, sometimes even in those patients who had previously received brentuximab vedotin. The dose was 3 mg/kgKG every two weeks until confirmed progression or unsustainable toxicities.
The intensively pretreated patient cohort (n=23) was from the ongoing phase Ib CheckMate 039 trial evaluating nivolumab in patients with relapsed or refractory hematologic malignancies. Data on non-Hodgkin’s lymphoma and multiple myeloma were discussed separately at the congress. Again, initial findings found promising efficacy [3].
High response
The secondary efficacy endpoint measured the following in the 23 Hodgkin’s lymphoma patients: The objective overall response rate (ORR) was 87% (n=20). Four patients achieved a complete response and 16 a partial response. In the remaining three individuals (13%), the disease was stable. There were 18 cases with prior brentuximab therapy in the entire group. Here, the ORR was as high as 89% – one patient of whom had a complete response. Progression-free survival was 86% at 24 weeks.
Turning to the primary endpoint, safety, drug-associated adverse events occurred in 78% of patients, with nearly one-quarter experiencing grade 3 toxicities. Overall, rash (22%), decreased platelet count (17%), and diarrhea, nausea, pruritus, fatigue, and fever (13% each) were most common. More severe side effects included myelodysplastic syndrome and pancreatitis, for example.
In conclusion, PD-1 blockade by nivolumab was tolerable in the cohort studied. No new safety concerns emerged compared to previous studies. For pretreated Hodgkin lymphoma patients, the high response rates are very encouraging. They suggest that the immuno-oncological approach has great potential here as well.
The PD-1 pathway appears to be of critical importance in Hodgkin lymphoma and sensitivity to PD-1 blockade is present. The FDA granted nivolumab breakthrough designation in 2014 for the treatment of Hodgkin’s lymphoma in which autologous stem cell transplantation and brentuximab failed. A large phase II study with several participating countries is in preparation.
Literature:
- Armand P, et al: Nivolumab in Patients with Relapsed or Refractory Hodgkin Lymphoma – Preliminary Safety, Efficacy and Biomarker Results of a Phase I Study. ASH 2014 Abstract #289.
- Ansell SM, et al: PD-1 Blockade with Nivolumab in Relapsed or Refractory Hodgkin’s Lymphoma. NEJM December 6, 2014. DOI: 10.1056/NEJMoa1411087.
- Lesokhin AM, et al: Preliminary Results of a Phase I Study of Nivolumab (BMS-936558) in Patients with Relapsed or Refractory Lymphoid Malignancies. ASH 2014 Abstract #291.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(1): 3.