Chronic tinnitus is a common symptom of the auditory system that can lead to serious disease burden, especially when combined with comorbidities. Therapy recommendations are aimed at reducing stress in the long term. A high value is placed on patient education. Treatment is based on the etiology and severity of the tinnitus on the one hand and on comorbidities on the other.
The updated version of the S3 guideline “Chronic Tinnitus” was published under the auspices of the German Society of Otolaryngology, Head and Neck Surgery (DGHNO-KHC) [1]. Chronic tinnitus (Latin for “ringing”) is defined as ringing in the ears that has been present for at least three months and causes distress to those affected. It is not a uniform clinical picture, but chronic tinnitus can take many forms.
According to current knowledge, tinnitus, whether symptomatic or idiopathic, can have a variety of causes, but is often based on a primary pathophysiological process in the inner ear. Central nervous processing often leads to pathologically exaggerated neuronal stimulus responses in severely affected individuals with tinnitus (e.g., exaggerated directing of attention to the tinnitus, anxiety, sleep disturbances). These are explained by psychophysiological and neurophysiological processing mechanisms of the tinnitus stimulus.
Diagnostic clarification and “tinnitus counselling
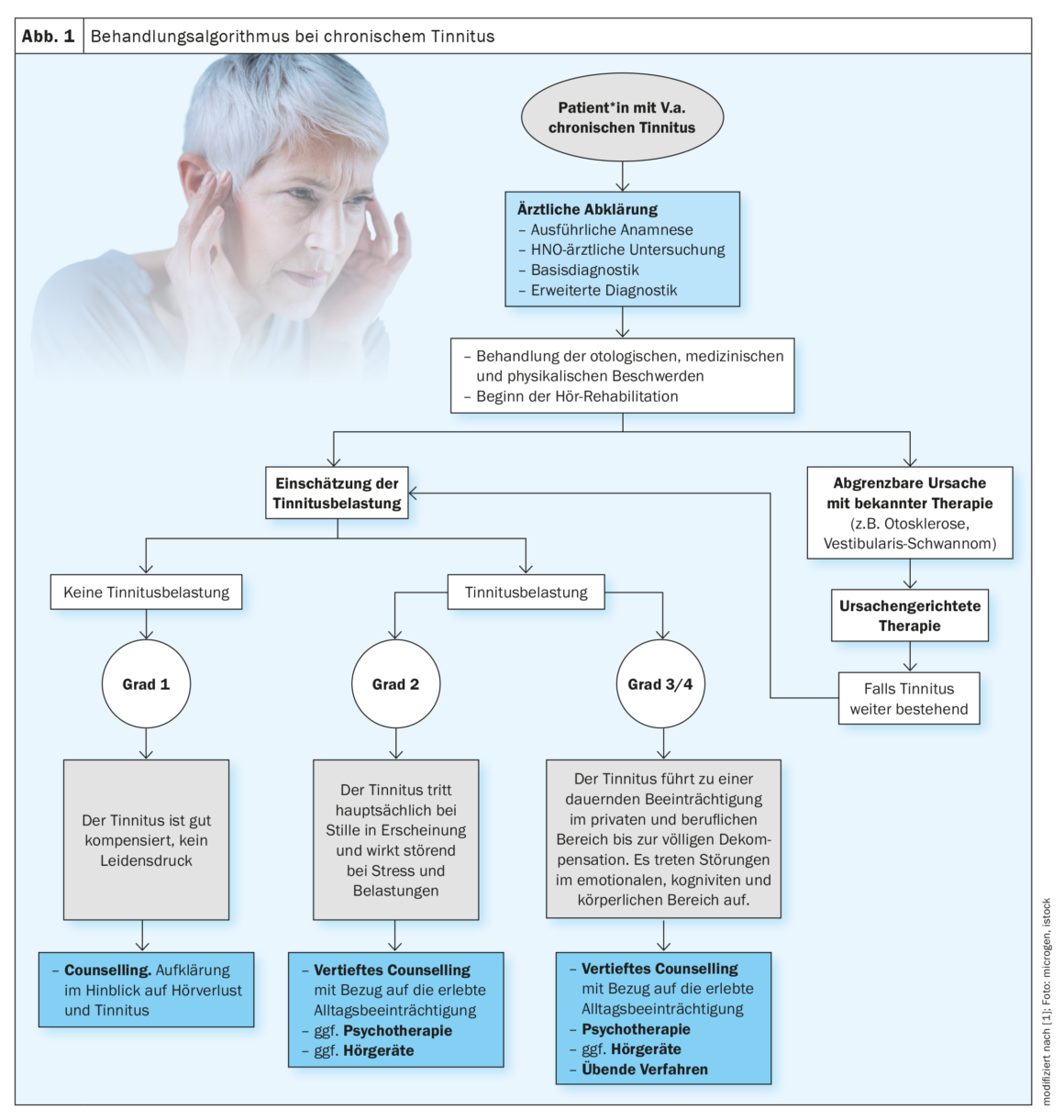
The cause and severity of tinnitus, as well as the extent of subjective distress, can be defined by extensive diagnostic testing. Education of the affected persons is an essential aspect of the clarification. During the diagnostic procedure, the audiological characteristics of the ringing in the ears and any hearing loss, as well as psychosomatic comorbidities and other concomitant diseases should be recorded. Based on this, a detailed and scary counseling should take place. Therapy must be tailored to this differential diagnostic assessment. A primary goal is to enable individuals to cope with the ear noise. The purpose of a therapy is therefore also to bring the brain from a stressful tinnitus perception as far as possible to the tinnitus habituation. To date, there are no monotherapies for tinnitus. The guideline discusses a wide range of interventions for which studies have been conducted in tinnitus patients.
Hearing aids, hearing therapy and cochlear implants
Evidence-based interventions include hearing aids or hearing therapy, and surgery for a cochlear implant. Some reviews generally confirm the efficacy of hearing aid fitting for tinnitus sufferers with hearing loss, although the evidence is moderate [2]. A noiser function in addition to the hearing aid does not bring any advantage for tinnitus patients. For profoundly hearing impaired patients with tinnitus, a cochlear implant fitting can provide good tinnitus suppression [3,4]. Specific auditory therapies can promote tinnitus relief by training and strengthening inhibitory effects of auditory perception [5]. This is done with targeted exercises of central auditory processing skills such as directional hearing, focusing and differentiation in noise with and without hearing aids and specifically an overhearing of tinnitus.
Tinnitus-specific psychotherapeutic procedures
As part of tinnitus-specific psychotherapy, patients should be taught that gradual habituation to the ear noise is often achievable. One goal of a sensible tinnitus therapy is that the tinnitus should in all likelihood no longer play a significant role in the daily routine of life. In the case of cognitive habituation, the ear noise still exists, but it is perceived less or no longer without active attention to the tinnitus. Tinnitus-specific cognitive behavioral therapy and grounded psychotherapy interventions are delivered in an individual or group setting. In addition to alleviating tinnitus distress and improving quality of life, an impact on comorbidities such as anxiety and depression can be achieved. Extensive studies are available demonstrating the efficacy of behavioral therapy interventions compared to waitlist control groups, as well as compared to active control groups, in terms of tinnitus burden [6]. The effectiveness is shown to be similar for the various forms of behavior therapy and, to a limited extent, for Internet-based behavior therapy. In addition to frequently and sufficiently evaluated behavioral therapy methods, more depth-psychologically oriented, psychodynamic interventions are also used in tinnitus therapy.
Music therapy interventions and retraining therapy.
Tinnitus retraining therapy may be considered as a long-term therapeutic measure for chronic tinnitus. The core of retraining therapy (TRT) is acoustic therapy with frequency-unmodulated noise, which was developed and introduced in the Anglo-American region based on the neurophysiological model [7–9]. A general use of tones, auditory scenes and broadband or narrowband noise in the range of tinnitus frequency has been tested and mainly sold in many approaches and application forms for tinnitus treatment. Effectiveness could not be proven for any of the procedures or studies on this were not even initiated.
Music therapy techniques are useful in terms of auditory skills training, but studies demonstrating efficacy in relation to chronic tinnitus are not available. The gradation of the recommendation level was based on the absence of evidence of efficacy. Tinnitus frequency interrupted (notch) music is offered as a smartphone app or in conjunction with hearing aids. It does not work any better for chronic tinnitus than normal, unmodified music. Various methods of stimulation by sounds, noises, auditory scenes, etc. have been proposed and tested. Because of this variety of methods, an overarching positive recommendation cannot be made. There is insufficient evidence for the efficacy of acoustic neuromodulation using the CR (coordinated reset) procedure.
Pharmacotherapeutic approaches
Overall, the guideline states that there is currently insufficient data for the efficacy of drug treatments specifically for tinnitus. However, it is recommended to treat psychiatric comorbidities of tinnitus. For example, antidepressants are often used successfully – not to improve the tinnitus itself, but to treat the accompanying depression and/or anxiety symptoms or a distressing sleep disorder [10]. Benzodiazepines should be used as bridging agents only with strict indications, e.g., as part of the initiation of antidepressant therapy, because of the substantial risks of side effects. There is no evidence for betahistine in the treatment of chronic tinnitus [11]. Drug manipulation of neurotransmission by gabapentin or glutamate antagonists proved to be mostly ineffective with respect to tinnitus symptoms.
Ginkgo biloba is the most commonly used herbal preparation for tinnitus. In a systematic review by Spiegel et al. positive effects of EGb761® (ginkgo extract) versus placebo in dementia in combination with tinnitus could be demonstrated [12,13].
As a basic premise for this analysis, it is assumed that ginkgo extract has a positive effect on tinnitus and dizziness symptoms, which has already been demonstrated elsewhere. When using ginkgo preparations, it should be kept in mind that the risk of bleeding may be increased in patients with underlying coagulation disorders [14].
Other measures
In addition to the drugs mentioned above, the guideline also discusses other drugs. In addition, there are separate sections on a wide variety of non-drug therapies. The guideline advises against the use of transcranial electrical stimulation methods for chronic tinnitus due to a lack of evidence. Transcutaneous or invasive vagus nerve stimulation alone or in conjunction with acoustic stimulation should also be avoided. The guideline authors also consider bimodal acoustic and electrical stimulation to be inappropriate for chronic tinnitus. And invasive electrostimulation of the brain should also be avoided in chronic tinnitus. This also applies to transcutaneous electrical nerve stimulation and low-level laser therapy.
On the other hand, manual medical and physiotherapeutic therapy should be offered for chronic tinnitus if modulations of the tinnitus are present due to comorbid changes in the cervical spine (CS) and masticatory apparatus [15,16]. Manual medical and physiotherapeutic therapies have a positive effect on the severity of tinnitus symptoms and on complaints in the cervical spine. A combination of physiotherapeutic and manual therapy in addition to patient education showed positive effects in tinnitus patients with concomitant craniomandibular dysfunction. Regarding dietary supplements (e.g., vitamins, minerals, or phytotherapeutics), there is currently no evidence of efficacy regarding tinnitus based on RCTs.
| Take-Home Messages Chronic tinnitus is often accompanied by hearing loss. The subjective distress caused by tinnitus varies greatly and is largely dependent on psychosomatic comorbidities, but also on the severity of the hearing loss. Counseling, psychotherapeutic interventions, and hearing improvement measures are recommended in the guideline. Psychophysiologically based therapeutic procedures target a tinnitus situation. Hearing aids are recommended for the treatment of concomitant hearing loss, and a cochlear implant may be considered if necessary. Tinnitus-specific psychotherapies can be delivered as individual or group therapies or combined as part of a multimodal approach. According to the guideline, there is insufficient evidence for tinnitus-specific drug treatment (including dietary supplements), and the same applies to sound/music therapies and neuromodulation procedures such as transcranial magnetic stimulation or electrical stimulation. Common comorbidities of tinnitus, such as anxiety disorders and depression, should be treated according to the guidelines, whereby drug therapy options can also be used. |
according to [1] |
Literature:
- Mazurek B, et al: S3 Guideline: Chronic Tinnitus 2022; ENT 70: 795-827.
https://doi.org/10.1007/s00106-022-01207-4 - Sereda M, et al: Sound therapy (using amplification devices and/or sound generators) for tinnitus. Cochrane Database Syst Rev 2018: 12: p. CD013094.
- Punte A, et al: Cochlear implantatio n as a durable tinnitus treatment in single-sided deafness. Cochlear Implants Int 2011; 12: 26-29.
- Pan T, et al: Changes in the tinnitus handicap questionnaire after cochlear implantation. Am J Audiol 2009; 18: 144-151.
- Hesse G: Neurootological-psychosomatic habituation therapy. Therapeutic approaches to chronic tinnitus. HNO 2008; 56: 686-693.
- Fuller T, et al: Cognitive behavioura l therapy for tinnitus. Cochrane Database Syst Rev 2020; 1: p. CD012614.
- Jastreboff PJ, et al: Neurophysiological model of tinnitus. Hear Res 1994; 80: 216-232.
- Jastreboff PJ: Tinnitus retraining therapy. Br J Audiol 1999; 33(1): 68-70.
- Henry JA, et al: Clinical trial to compare tinnitus masking and tinnitus retraining therapy. Acta Oto Laryngologica 2006; 126: 64-69.
- Baldo P, et al: Antidepressants for patients with tinnitus. Cochrane Darabase Syst Rev 2012(9): CD003853.
- Wegner I, et al: Betahistine for tinnitus. Cochrane Database Syst Rev 2018; 12: CD013093.
- Spiegel R, et al: Ginkgo biloba extract EGb 761® alleviates neurosensory symptoms in patients with dementia: a meta-analysis of treatment effects on tinnitus and dizziness in randomized, placebo-controlled trials. Clin Interv Aging 2018; 13: 1121-1127.
- Drug Information, www.swissmedicinfo.ch,(last accessed 04/26/2023).
- Posadzki P, et al: Adverse effects of herbal medicines: an overview of systematic reviews. Clin Med (Lond) 2013; 13(1): 7-12.
- Michiels S, et al: Does multi-modal cervical physical therapy improve tinnitus in patients with cervicogenic somatic tinnitus? Man Ther 2016; 26: 125-131.
- Delgado de la Serna P, et al: Effects of Cervico-Mandibular Manual Therapy in Patients with Temporomandibular Pain Disorders and Associated Somatic Tinnitus: A Randomized Clinical Trial. Pain Med 2020; 21(3): 613-624.
HAUSARZT PRAXIS 2023; 18(5): 33-35